Abstract
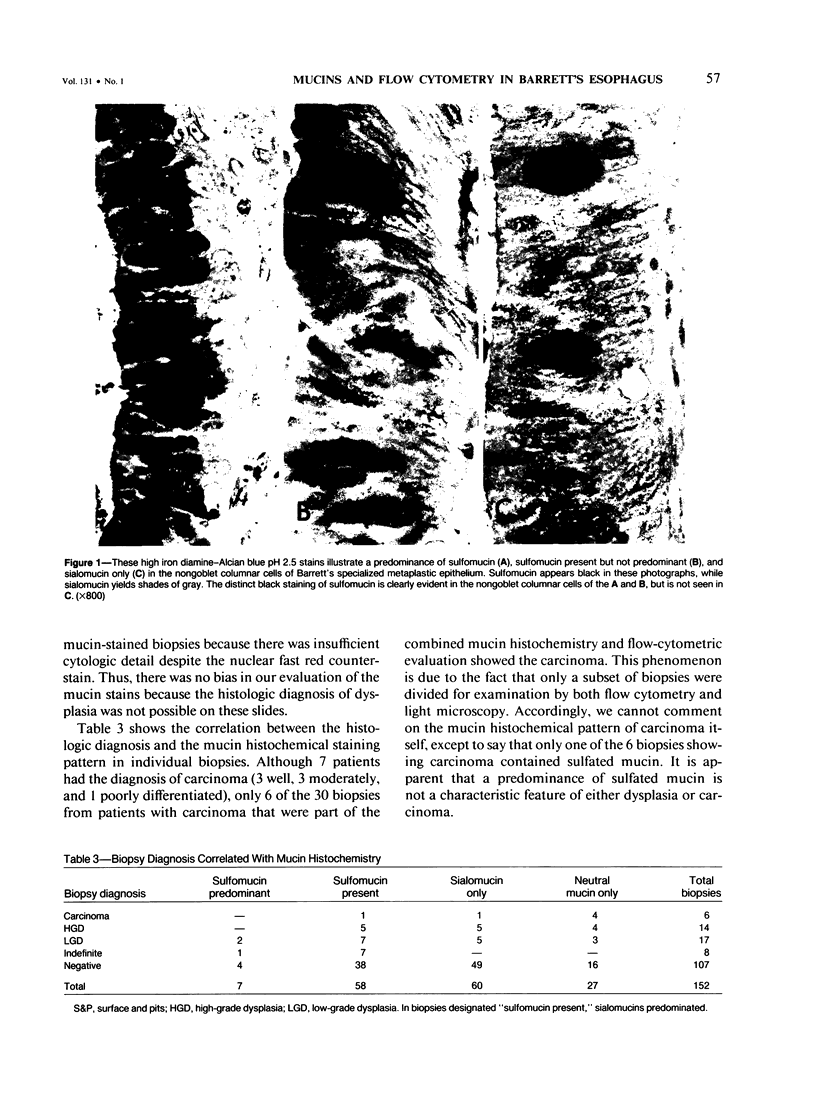
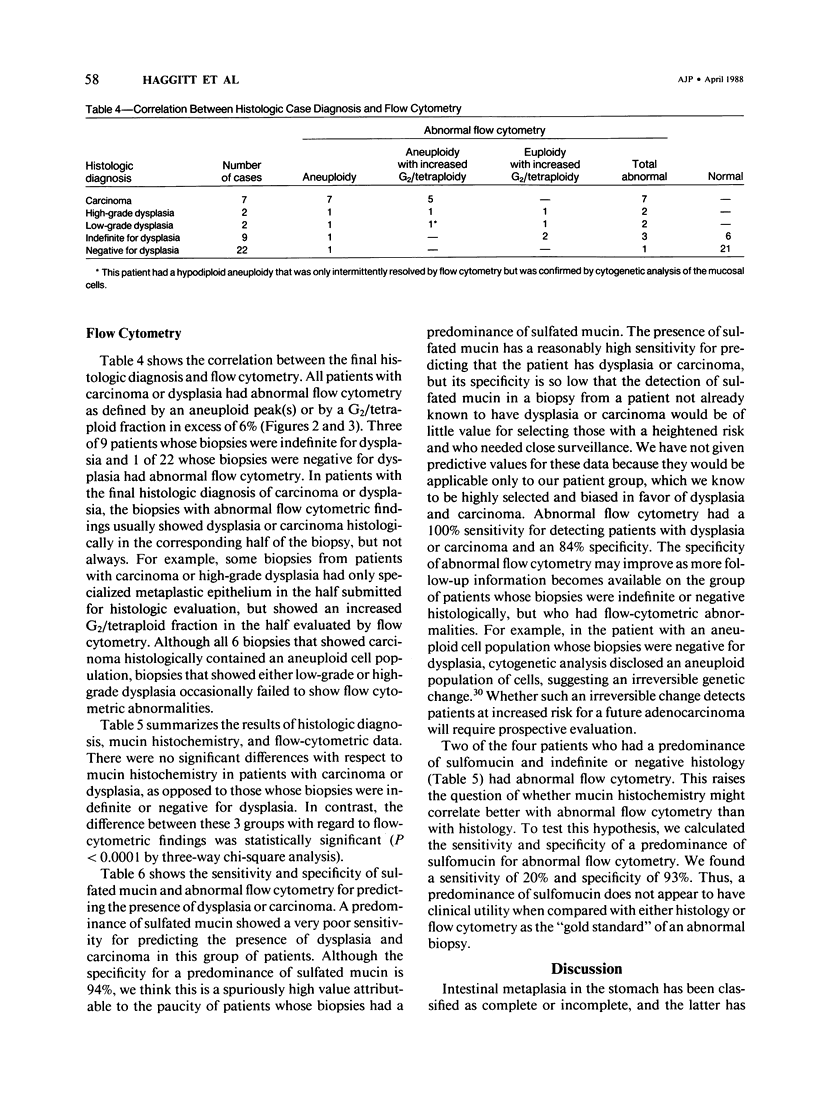
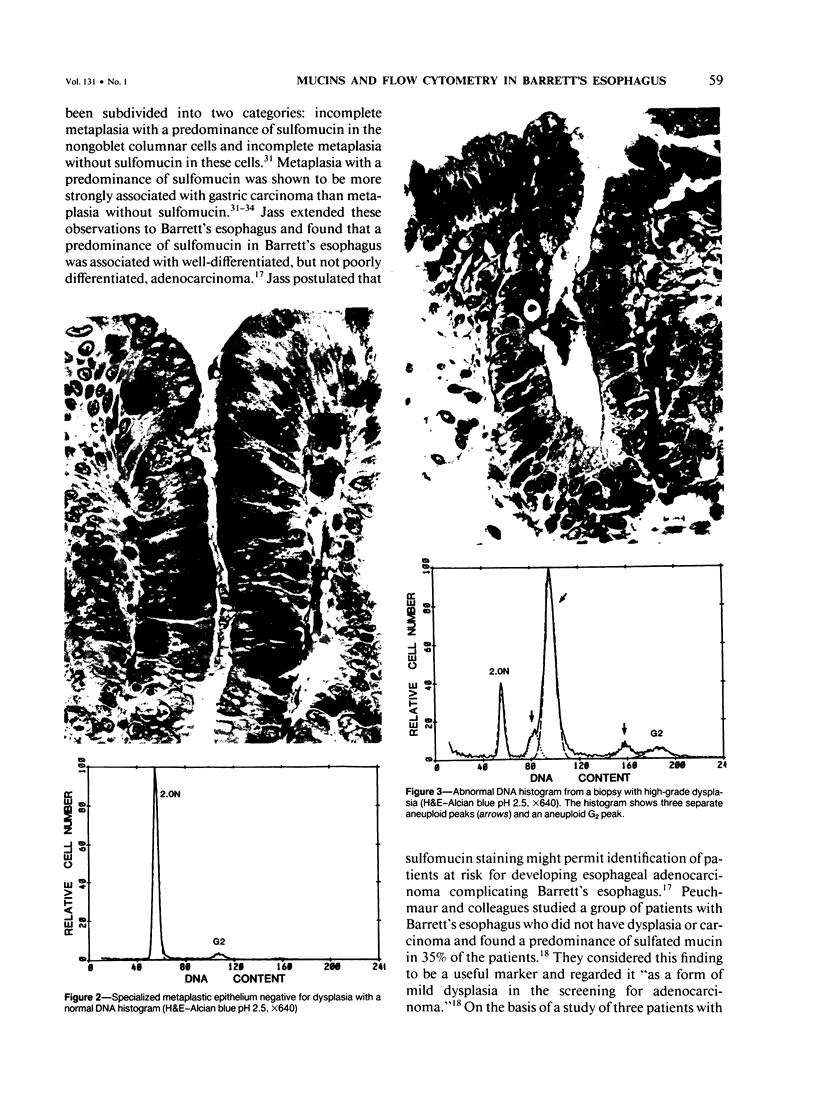
A predominance of sulfated mucin in the nongoblet columnar cells of Barrett's specialized metaplastic epithelium has been postulated to be a form of mild dysplasia and to indicate an increased risk of adenocarcinoma. Flow cytometry for the analysis of nuclear DNA content and cell cycle parameters has also been postulated to be an objective aid in the diagnosis of dysplasia and carcinoma in Barrett's esophagus. The authors investigated the relationship among sulfated mucin, flow cytometric data, and histologic diagnosis in each of 152 biopsies from 42 patients who had Barrett's specialized metaplastic epithelium. Sulfated mucin, as detected by the high iron diamine-Alcian blue stain, was present in biopsies from 8 of 11 (73%) patients with the histologic diagnosis of dysplasia or carcinoma, in 7 of 9 (78%) patients whose biopsies were indefinite for dysplasia, and in 12 of 22 (55%) patients whose biopsies were negative for dysplasia (P = 0.37). Sulfated mucins predominated in 9%, 22%, and 9% of the patients, respectively (P = 0.56). Abnormal flow cytometry (aneuploidy or increased G2/tetraploid fraction) was found in all patients with the histologic diagnosis of dysplasia or carcinoma, in 3 of 9 (33%) indefinite for dysplasia, and in 1 of 22 (5%) negative for dysplasia (P = less than 0.0001). Neither the presence nor the predominance of sulfated mucin in the specialized metaplastic epithelium of Barrett's esophagus has sufficiently high sensitivity or specificity for dysplasia or carcinoma to be of value in managing patients. Abnormal flow cytometry shows excellent correlation with the histologic diagnosis of dysplasia and carcinoma; it detects a subset of patients whose biopsies are histologically indefinite or negative for dysplasia, but who have flow cytometric abnormalities similar to those otherwise seen only in dysplasia and carcinoma.
Full text
PDF




Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- BARRETT N. R. Chronic peptic ulcer of the oesophagus and 'oesophagitis'. Br J Surg. 1950 Oct;38(150):175–182. doi: 10.1002/bjs.18003815005. [DOI] [PubMed] [Google Scholar]
- Belladonna J. A., Hajdu S. I., Bains M. S., Winawer S. J. Adenocarcinoma in situ of Barrett's esophagus diagnosed by endoscopic cytology. N Engl J Med. 1974 Oct 24;291(17):895–896. doi: 10.1056/NEJM197410242911709. [DOI] [PubMed] [Google Scholar]
- Berenson M. M., Riddell R. H., Skinner D. B., Freston J. W. Malignant transformation of esophageal columnar epithelium. Cancer. 1978 Feb;41(2):554–561. doi: 10.1002/1097-0142(197802)41:2<554::aid-cncr2820410223>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- Cameron A. J., Ott B. J., Payne W. S. The incidence of adenocarcinoma in columnar-lined (Barrett's) esophagus. N Engl J Med. 1985 Oct 3;313(14):857–859. doi: 10.1056/NEJM198510033131404. [DOI] [PubMed] [Google Scholar]
- Dean P. N., Jett J. H. Mathematical analysis of DNA distributions derived from flow microfluorometry. J Cell Biol. 1974 Feb;60(2):523–527. doi: 10.1083/jcb.60.2.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haggitt R. C., Tryzelaar J., Ellis F. H., Colcher H. Adenocarcinoma complicating columnar epithelium-lined (Barrett's) esophagus. Am J Clin Pathol. 1978 Jul;70(1):1–5. doi: 10.1093/ajcp/70.1.1. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. A variant of intestinal metaplasia associated with gastric carcinoma: a histochemical study. Histopathology. 1979 May;3(3):191–199. doi: 10.1111/j.1365-2559.1979.tb02996.x. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. Sulphomucins and precancerous lesions of the human stomach. Histopathology. 1980 May;4(3):271–279. doi: 10.1111/j.1365-2559.1980.tb02921.x. [DOI] [PubMed] [Google Scholar]
- Jass J. R., Filipe M. I. The mucin profiles of normal gastric mucosa, intestinal metaplasia and its variants and gastric carcinoma. Histochem J. 1981 Nov;13(6):931–939. doi: 10.1007/BF01002633. [DOI] [PubMed] [Google Scholar]
- Jass J. R. Mucin histochemistry of the columnar epithelium of the oesophagus: a retrospective study. J Clin Pathol. 1981 Aug;34(8):866–870. doi: 10.1136/jcp.34.8.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jass J. R. Role of intestinal metaplasia in the histogenesis of gastric carcinoma. J Clin Pathol. 1980 Sep;33(9):801–810. doi: 10.1136/jcp.33.9.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee R. G. Dysplasia in Barrett's esophagus. A clinicopathologic study of six patients. Am J Surg Pathol. 1985 Dec;9(12):845–852. doi: 10.1097/00000478-198512000-00001. [DOI] [PubMed] [Google Scholar]
- Lee R. G. Mucins in Barrett's esophagus: a histochemical study. Am J Clin Pathol. 1984 Apr;81(4):500–503. doi: 10.1093/ajcp/81.4.500. [DOI] [PubMed] [Google Scholar]
- Naef A. P., Savary M., Ozzello L. Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett's esophagus with 12 adenocarcinomas. J Thorac Cardiovasc Surg. 1975 Nov;70(5):826–835. [PubMed] [Google Scholar]
- Paull A., Trier J. S., Dalton M. D., Camp R. C., Loeb P., Goyal R. K. The histologic spectrum of Barrett's esophagus. N Engl J Med. 1976 Aug 26;295(9):476–480. doi: 10.1056/NEJM197608262950904. [DOI] [PubMed] [Google Scholar]
- Peuchmaur M., Potet F., Goldfain D. Mucin histochemistry of the columnar epithelium of the oesophagus (Barrett's oesophagus): a prospective biopsy study. J Clin Pathol. 1984 Jun;37(6):607–610. doi: 10.1136/jcp.37.6.607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reid B. J., Haggitt R. C., Rubin C. E., Rabinovitch P. S. Barrett's esophagus. Correlation between flow cytometry and histology in detection of patients at risk for adenocarcinoma. Gastroenterology. 1987 Jul;93(1):1–11. [PubMed] [Google Scholar]
- Reid B. J., Weinstein W. M., Lewin K. J., Haggitt R. C., VanDeventer G., DenBesten L., Rubin C. E. Endoscopic biopsy can detect high-grade dysplasia or early adenocarcinoma in Barrett's esophagus without grossly recognizable neoplastic lesions. Gastroenterology. 1988 Jan;94(1):81–90. doi: 10.1016/0016-5085(88)90613-0. [DOI] [PubMed] [Google Scholar]
- Riddell R. H., Goldman H., Ransohoff D. F., Appelman H. D., Fenoglio C. M., Haggitt R. C., Ahren C., Correa P., Hamilton S. R., Morson B. C. Dysplasia in inflammatory bowel disease: standardized classification with provisional clinical applications. Hum Pathol. 1983 Nov;14(11):931–968. doi: 10.1016/s0046-8177(83)80175-0. [DOI] [PubMed] [Google Scholar]
- Rothery G. A., Patterson J. E., Stoddard C. J., Day D. W. Histological and histochemical changes in the columnar lined (Barrett's) oesophagus. Gut. 1986 Sep;27(9):1062–1068. doi: 10.1136/gut.27.9.1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt H. G., Riddell R. H., Walther B., Skinner D. B., Riemann J. F. Dysplasia in Barrett's esophagus. J Cancer Res Clin Oncol. 1985;110(2):145–152. doi: 10.1007/BF00402729. [DOI] [PubMed] [Google Scholar]
- Sheahan D. G., Jervis H. R. Comparative histochemistry of gastrointestinal mucosubstances. Am J Anat. 1976 Jun;146(2):103–131. doi: 10.1002/aja.1001460202. [DOI] [PubMed] [Google Scholar]
- Sheahan D. G., Jervis H. R., Takeuchi A., Sprinz H. The effect of staphylococcal enterotoxin on the epithelial mucosubstances of the small intestine of rhesus monkeys. Am J Pathol. 1970 Jul;60(1):1–18. [PMC free article] [PubMed] [Google Scholar]
- Sjogren R. W., Jr, Johnson L. F. Barrett's esophagus: a review. Am J Med. 1983 Feb;74(2):313–321. doi: 10.1016/0002-9343(83)90635-6. [DOI] [PubMed] [Google Scholar]
- Skinner D. B., Walther B. C., Riddell R. H., Schmidt H., Iascone C., DeMeester T. R. Barrett's esophagus. Comparison of benign and malignant cases. Ann Surg. 1983 Oct;198(4):554–565. doi: 10.1097/00000658-198310000-00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith R. R., Hamilton S. R., Boitnott J. K., Rogers E. L. The spectrum of carcinoma arising in Barrett's esophagus. A clinicopathologic study of 26 patients. Am J Surg Pathol. 1984 Aug;8(8):563–573. doi: 10.1097/00000478-198408000-00001. [DOI] [PubMed] [Google Scholar]
- Spechler S. J., Goyal R. K. Barrett's esophagus. N Engl J Med. 1986 Aug 7;315(6):362–371. doi: 10.1056/NEJM198608073150605. [DOI] [PubMed] [Google Scholar]
- Spechler S. J., Robbins A. H., Rubins H. B., Vincent M. E., Heeren T., Doos W. G., Colton T., Schimmel E. M. Adenocarcinoma and Barrett's esophagus. An overrated risk? Gastroenterology. 1984 Oct;87(4):927–933. [PubMed] [Google Scholar]
- Taylor I. W. A rapid single step staining technique for DNA analysis by flow microfluorimetry. J Histochem Cytochem. 1980 Sep;28(9):1021–1024. doi: 10.1177/28.9.6157714. [DOI] [PubMed] [Google Scholar]
- Thornthwaite J. T., Sugarbaker E. V., Temple W. J. Preparation of tissues for DNA flow cytometric analysis. Cytometry. 1980 Nov;1(3):229–237. doi: 10.1002/cyto.990010309. [DOI] [PubMed] [Google Scholar]
- Witt T. R., Bains M. S., Zaman M. B., Martini N. Adenocarcinoma in Barrett's esophagus. J Thorac Cardiovasc Surg. 1983 Mar;85(3):337–345. [PubMed] [Google Scholar]
- Womack C., Harvey L. Columnar epithelial lined oesophagus (CELO) or Barrett's oesophagus: mucin histochemistry, dysplasia, and invasive adenocarcinoma. J Clin Pathol. 1985 Apr;38(4):477–478. doi: 10.1136/jcp.38.4.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwas F., Shields H. M., Doos W. G., Antonioli D. A., Goldman H., Ransil B. J., Spechler S. J. Scanning electron microscopy of Barrett's epithelium and its correlation with light microscopy and mucin stains. Gastroenterology. 1986 Jun;90(6):1932–1941. doi: 10.1016/0016-5085(86)90264-7. [DOI] [PubMed] [Google Scholar]