Abstract
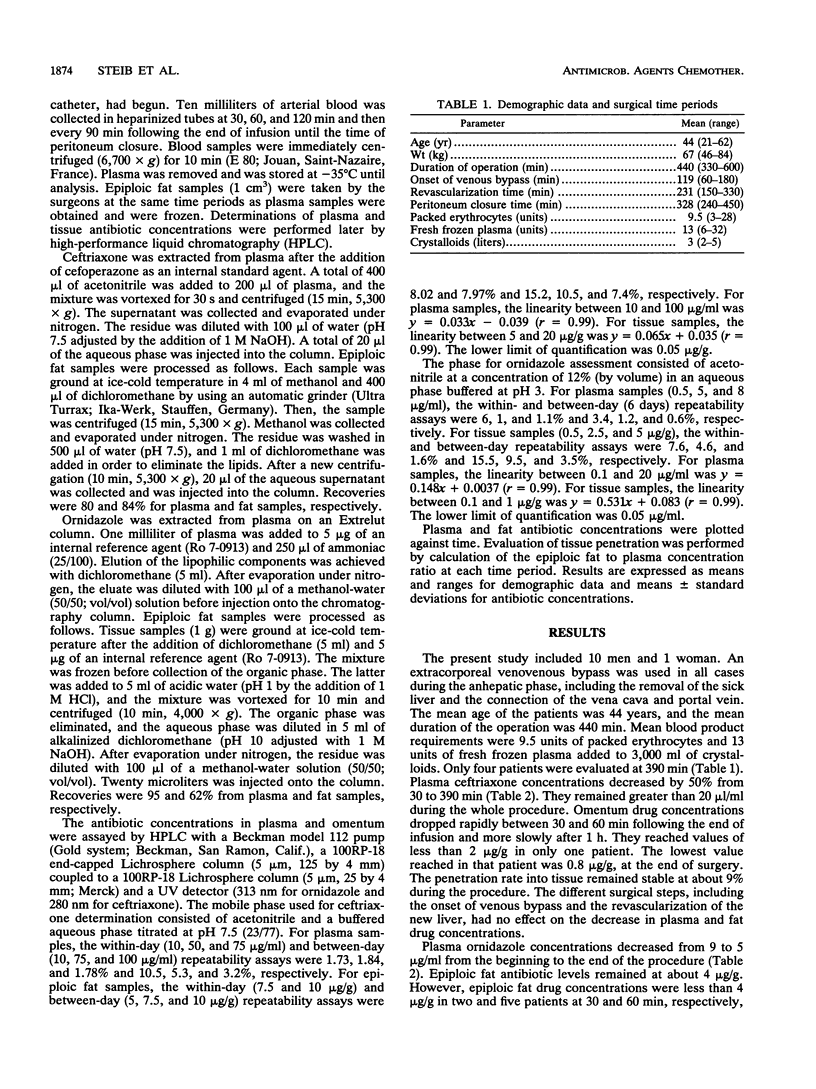
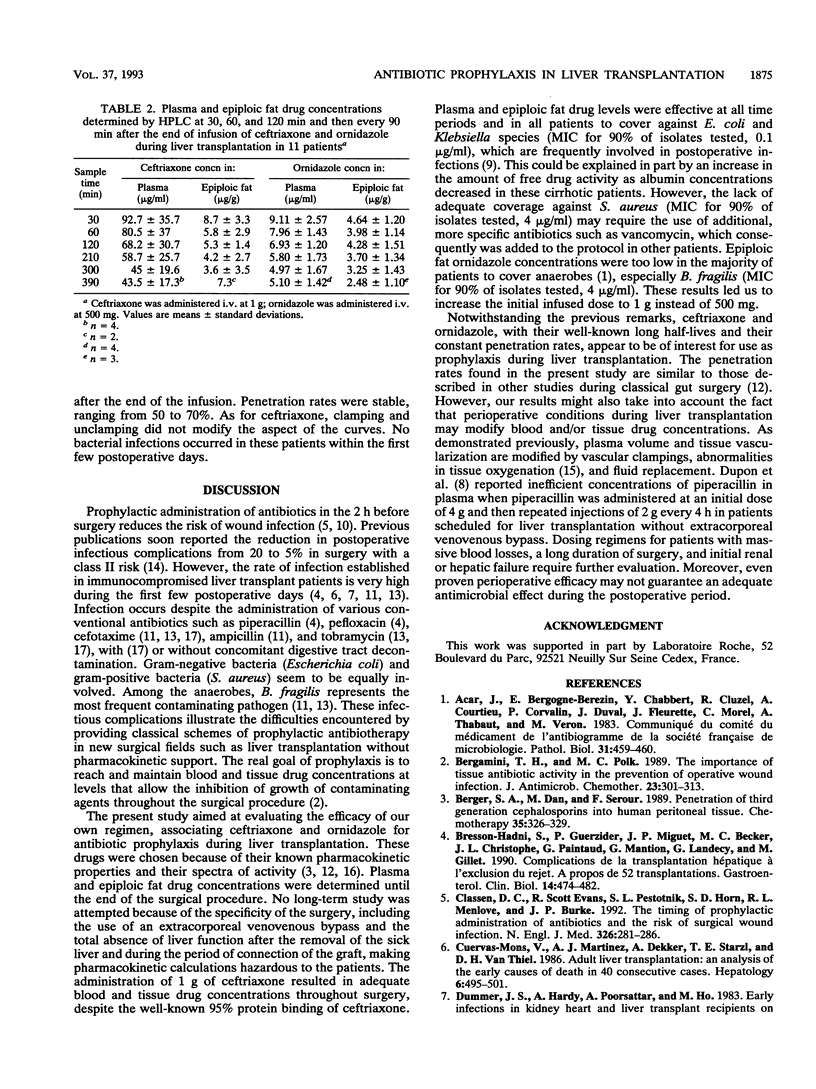
Plasma and epiploic fat drug concentrations and fat penetration of ceftriaxone and ornidazole given for antimicrobial prophylaxis were studied in 11 patients scheduled for liver transplantation. Ceftriaxone (1 g) and ornidazole (500 mg) were infused during 30 min after the induction of anesthesia. Arterial blood and epiploic fat samples were collected at 30, 60, and 120 min and then every 90 min following the end of the infusion until closure of the peritoneum. Blood samples were immediately centrifuged, and plasma and fat were stored at -35 degrees C until analysis. Ceftriaxone and ornidazole concentrations were determined by high-performance liquid chromatography. Surgery lasted 440 +/- 84 min and required a mean of 9.5 units of packed erythrocytes and 13 units of fresh frozen plasma. Plasma ceftriaxone concentrations decreased from 89 +/- 34 to 41 +/- 16.5 micrograms/ml from the beginning of the operation until the time of closure of the peritoneum. Corresponding levels in epiploic fat decreased from 8.7 +/- 3.3 to 4.5 +/- 3.5 micrograms/g. Ornidazole concentrations ranged, respectively, between 8.7 +/- 2.5 and 4.9 +/- 1.7 micrograms/ml in plasma samples and 4.6 +/- 1.2 and 2.5 +/- 1.1. micrograms/g in fat samples. Rates of penetration into the omentum remained at about 9% for ceftriaxone and between 50 and 70% for ornidazole. Tissue ceftriaxone concentrations were, in all cases, greater than typical MICs for 90% for Escherichia coli and Klebsiella isolates tested (MIC90S). They were insufficient in 40% of patients after 60 min with regard to the MIC90S for Staphylococcus aureus. Tissue ornidazole concentrations were not superior to MIC90S for anaerobes after 30 min in 50% of patients. These results show that a single dose of 1 g of ceftriaxone provides adequate coverage against gram-negative bacteria and that 1 g instead of 500 mg ornidazole may provide a protective effect against anaerobes during liver transplantation. Prophylaxis against S. aureus and Streptococcus faecalis requires more specific antibiotics. Prophylaxis for patients with significant blood loss or initial severe renal or hepatic failure needs further evaluation.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bergamini T. M., Polk H. C., Jr The importance of tissue antibiotic activity in the prevention of operative wound infection. J Antimicrob Chemother. 1989 Mar;23(3):301–313. doi: 10.1093/jac/23.3.301. [DOI] [PubMed] [Google Scholar]
- Berger S. A., Dan M., Serour F., Gorea A., Levenberg A., Krispin M. Penetration of third-generation cephalosporins into human peritoneal tissue. Chemotherapy. 1989;35(5):326–329. doi: 10.1159/000238689. [DOI] [PubMed] [Google Scholar]
- Bresson-Hadni S., Guerzider P., Miguet J. P., Becker M. C., Christophe J. L., Paintaud G., Mantion G., Landecy G., Gillet M. Complications de la transplantation hépatique à l'exclusion du rejet. A propos de 52 transplantations. Gastroenterol Clin Biol. 1990;14(5):474–482. [PubMed] [Google Scholar]
- Classen D. C., Evans R. S., Pestotnik S. L., Horn S. D., Menlove R. L., Burke J. P. The timing of prophylactic administration of antibiotics and the risk of surgical-wound infection. N Engl J Med. 1992 Jan 30;326(5):281–286. doi: 10.1056/NEJM199201303260501. [DOI] [PubMed] [Google Scholar]
- Cuervas-Mons V., Julio Martinez A., Dekker A., Starzl T. E., Van Thiel D. H. Adult liver transplantation: an analysis of the early causes of death in 40 consecutive cases. Hepatology. 1986 May-Jun;6(3):495–501. doi: 10.1002/hep.1840060329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Emmerson A. M., Lamport P. A., Reeves D. S., Bywater M. J., Holt H. A., Wise R., Andrews J., Hall M. J. The in vitro antibacterial activity of ceftriaxone in comparison with nine other antibiotics. Curr Med Res Opin. 1985;9(7):480–493. doi: 10.1185/03007998509109622. [DOI] [PubMed] [Google Scholar]
- Kaiser A. B. Antimicrobial prophylaxis in surgery. N Engl J Med. 1986 Oct 30;315(18):1129–1138. doi: 10.1056/NEJM198610303151805. [DOI] [PubMed] [Google Scholar]
- Kusne S., Dummer J. S., Singh N., Iwatsuki S., Makowka L., Esquivel C., Tzakis A. G., Starzl T. E., Ho M. Infections after liver transplantation. An analysis of 101 consecutive cases. Medicine (Baltimore) 1988 Mar;67(2):132–143. doi: 10.1097/00005792-198803000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martin C., Bruguerolle B., Mallet M. N., Condomines M., Sastre B., Gouin F. Pharmacokinetics and tissue penetration of a single dose of ornidazole (1,000 milligrams intravenously) for antibiotic prophylaxis in colorectal surgery. Antimicrob Agents Chemother. 1990 Oct;34(10):1921–1924. doi: 10.1128/aac.34.10.1921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paya C. V., Hermans P. E., Washington J. A., 2nd, Smith T. F., Anhalt J. P., Wiesner R. H., Krom R. A. Incidence, distribution, and outcome of episodes of infection in 100 orthotopic liver transplantations. Mayo Clin Proc. 1989 May;64(5):555–564. doi: 10.1016/s0025-6196(12)65561-x. [DOI] [PubMed] [Google Scholar]
- Polk H. C., Jr, Lopez-Mayor J. F. Postoperative wound infection: a prospective study of determinant factors and prevention. Surgery. 1969 Jul;66(1):97–103. [PubMed] [Google Scholar]
- Steib A., Freys G., Gohard R., Curzola U., Ravanello J., Lutun P., Boudjema K., Otteni J. C. Tissue oxygenation during liver transplantation. Crit Care Med. 1992 Jul;20(7):977–983. doi: 10.1097/00003246-199207000-00013. [DOI] [PubMed] [Google Scholar]
- Taburet A. M., Delion F., Attali P., Thebault J. J., Singlas E. Pharmacokinetics of ornidazole in patients with severe liver cirrhosis. Clin Pharmacol Ther. 1986 Sep;40(3):359–364. doi: 10.1038/clpt.1986.189. [DOI] [PubMed] [Google Scholar]
- Wiesner R. H. The incidence of gram-negative bacterial and fungal infections in liver transplant patients treated with selective decontamination. Infection. 1990;18 (Suppl 1):S19–S21. doi: 10.1007/BF01644482. [DOI] [PubMed] [Google Scholar]


