Abstract
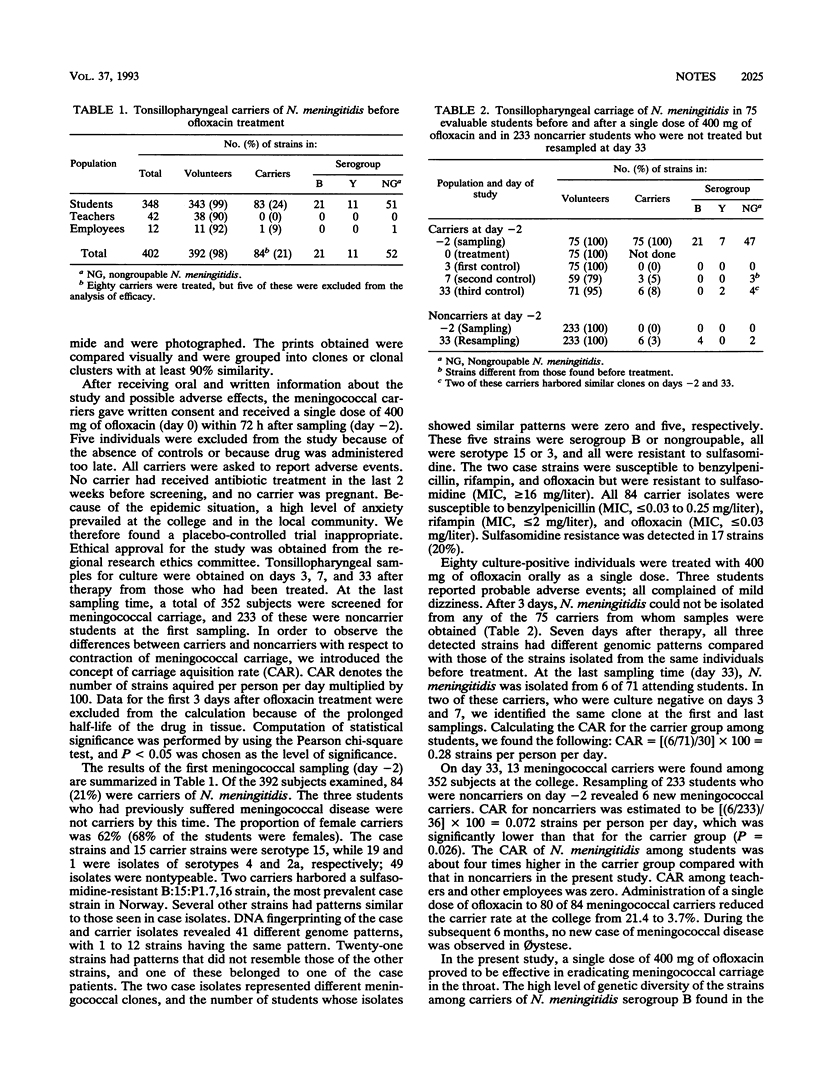
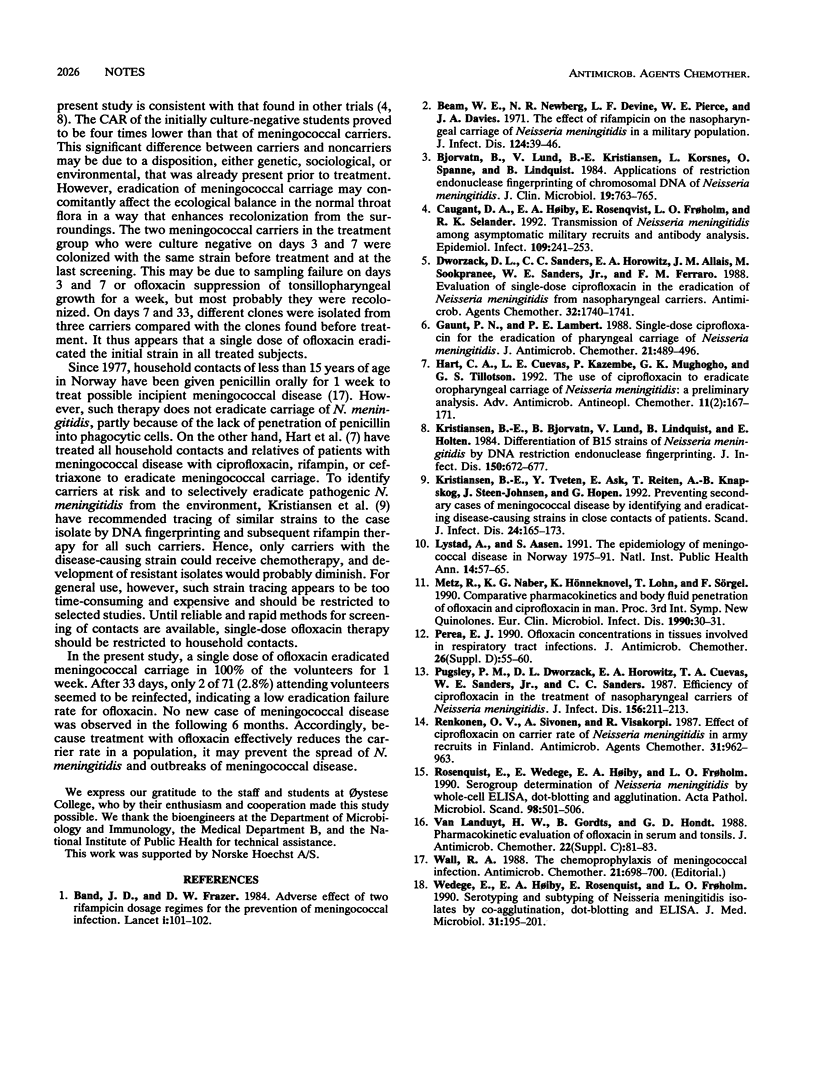
After an outbreak of three cases of serogroup B meningococcal disease at a Norwegian college, 84 of 392 (21%) subjects were tonsillopharyngeal carriers of Neisseria meningitidis. To eradicate meningococcal carriage, 80 volunteers received a single dose of 400 mg of ofloxacin. Three days after treatment, all 75 evaluable volunteers were culture negative for N. meningitidis, and after 7 days none carried the strain that they carried initially, as judged by DNA fingerprinting. A single dose of ofloxacin was found to be 97.2% effective in eradicating carriage of N. meningitidis for a period of 33 days. The carriage acquisition rate among treated students was four times higher than that among nontreated noncarriers (P = 0.02). After ofloxacin treatment, no case of meningococcal disease occurred for 6 months. Ofloxacin may thus prevent the outbreak and spread of meningococcal disease.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Band J. D., Fraser D. W. Adverse effects of two rifampicin dosage regimens for the prevention of meningococcal infection. Lancet. 1984 Jan 14;1(8368):101–102. doi: 10.1016/s0140-6736(84)90025-4. [DOI] [PubMed] [Google Scholar]
- Beam W. E., Jr, Newberg N. R., Devine L. F., Pierce W. E., Davies J. A. The effect of rifampin on the nasopharyngeal carriage of Neisseria meningitidis in a military population. J Infect Dis. 1971 Jul;124(1):39–46. doi: 10.1093/infdis/124.1.39. [DOI] [PubMed] [Google Scholar]
- Bjorvatn B., Lund V., Kristiansen B. E., Korsnes L., Spanne O., Lindqvist B. Applications of restriction endonuclease fingerprinting of chromosomal DNA of Neisseria meningitidis. J Clin Microbiol. 1984 Jun;19(6):763–765. doi: 10.1128/jcm.19.6.763-765.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caugant D. A., Høiby E. A., Rosenqvist E., Frøholm L. O., Selander R. K. Transmission of Neisseria meningitidis among asymptomatic military recruits and antibody analysis. Epidemiol Infect. 1992 Oct;109(2):241–253. doi: 10.1017/s0950268800050196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworzack D. L., Sanders C. C., Horowitz E. A., Allais J. M., Sookpranee M., Sanders W. E., Jr, Ferraro F. M. Evaluation of single-dose ciprofloxacin in the eradication of Neisseria meningitidis from nasopharyngeal carriers. Antimicrob Agents Chemother. 1988 Nov;32(11):1740–1741. doi: 10.1128/aac.32.11.1740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gaunt P. N., Lambert B. E. Single dose ciprofloxacin for the eradication of pharyngeal carriage of Neisseria meningitidis. J Antimicrob Chemother. 1988 Apr;21(4):489–496. doi: 10.1093/jac/21.4.489. [DOI] [PubMed] [Google Scholar]
- Kristiansen B. E., Bjorvatn B., Lund V., Lindqvist B., Holten E. Differentiation of B15 strains of Neisseria meningitidis by DNA restriction endonuclease fingerprinting. J Infect Dis. 1984 Nov;150(5):672–677. doi: 10.1093/infdis/150.5.672. [DOI] [PubMed] [Google Scholar]
- Kristiansen B. E., Tveten Y., Ask E., Reiten T., Knapskog A. B., Steen-Johnsen J., Hopen G. Preventing secondary cases of meningococcal disease by identifying and eradicating disease-causing strains in close contacts of patients. Scand J Infect Dis. 1992;24(2):165–173. doi: 10.3109/00365549209052608. [DOI] [PubMed] [Google Scholar]
- Lystad A., Aasen S. The epidemiology of meningococcal disease in Norway 1975-91. NIPH Ann. 1991 Dec;14(2):57–66. [PubMed] [Google Scholar]
- Perea E. J. Ofloxacin concentrations in tissues involved in respiratory tract infections. J Antimicrob Chemother. 1990 Nov;26 (Suppl 500):55–60. doi: 10.1093/jac/26.suppl_d.55. [DOI] [PubMed] [Google Scholar]
- Pugsley M. P., Dworzack D. L., Horowitz E. A., Cuevas T. A., Sanders W. E., Jr, Sanders C. C. Efficacy of ciprofloxacin in the treatment of nasopharyngeal carriers of Neisseria meningitidis. J Infect Dis. 1987 Jul;156(1):211–213. doi: 10.1093/infdis/156.1.211. [DOI] [PubMed] [Google Scholar]
- Renkonen O. V., Sivonen A., Visakorpi R. Effect of ciprofloxacin on carrier rate of Neisseria meningitidis in army recruits in Finland. Antimicrob Agents Chemother. 1987 Jun;31(6):962–963. doi: 10.1128/aac.31.6.962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenqvist E., Wedege E., Høiby E. A., Frøholm L. O. Serogroup determination of Neisseria meningitidis by whole-cell ELISA, dot-blotting and agglutination. APMIS. 1990 Jun;98(6):501–506. [PubMed] [Google Scholar]
- Van Landuyt H. W., Gordts B., D'Hondt G. Pharmacokinetic evaluation of ofloxacin in serum and tonsils. J Antimicrob Chemother. 1988 Sep;22 (Suppl 100):81–83. doi: 10.1093/jac/22.supplement_c.81. [DOI] [PubMed] [Google Scholar]
- Wall R. A. The chemoprophylaxis of meningococcal infection. J Antimicrob Chemother. 1988 Jun;21(6):698–700. doi: 10.1093/jac/21.6.698. [DOI] [PubMed] [Google Scholar]
- Wedege E., Høiby E. A., Rosenqvist E., Frøholm L. O. Serotyping and subtyping of Neisseria meningitidis isolates by co-agglutination, dot-blotting and ELISA. J Med Microbiol. 1990 Mar;31(3):195–201. doi: 10.1099/00222615-31-3-195. [DOI] [PubMed] [Google Scholar]


