Short abstract
Medical resources are increasingly shifting from making patients better to preventing them from becoming ill. Genetic testing is likely to extend the list of conditions that can be screened for. Is it time to stop and consider whom we screen and how we approach it?
Most medical experts and health authorities consider consultations in primary health care ideal for opportunistic health promotion and disease prevention. Doctors are thus expected to discuss preventive measures even when they are not among the reasons for contact. But are such opportunistic initiatives ethically justifiable in contemporary Western medicine? We argue that doctors should maintain a clear focus on each patient's reasons for seeking help rather than be distracted by an increasing list of standardised preventive measures with unpredictable relevance to the individual.
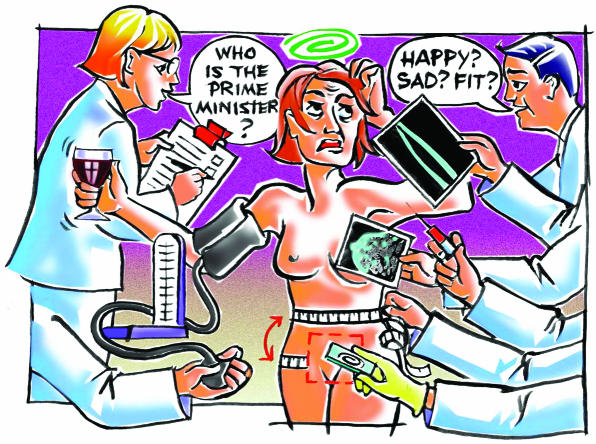
Figure 1.
Aims of a good consultation
The cornerstone of medical practice is the consultation between a patient who seeks help and a doctor whom the person trusts.1 Several theoretical models have been developed to analyse and improve the quality of the consultation. In 1979, Stott and Davis presented an influential model that elicited four potentials of the encounter between patient and doctor: management of presenting problems, modification of help seeking behaviour, management of continuing problems, and opportunistic health promotion.2 Since then, opportunistic preventive initiatives have become considered to be part of good medical practice.
From a moral point of view, preventive medicine— that is, initiatives to improve health among people who are currently free of symptoms—is fundamentally different from curative medicine, which is offered to patients who seek medical help. The two disciplines imply different promises and have different obligations to the individuals whose lives they modify.3
Expanding agenda of risk and prevention
When Stott and Davis developed their model, the number of relevant opportunistic initiatives was limited and seemed both technically feasible and ethically justifiable. However, interest in risk factors in healthy populations has expanded rapidly over the past two decades. A “risk epidemic” has occurred in medical publishing,4 and the range of tests that can be done or started in general practice has become extensive. Discussion of lifestyle and monitoring blood pressure of healthy people are well established. Other indicators of cardiovascular risk have been added more recently, including blood lipid concentrations, body mass index, blood glucose concentration, and waist-hip ratio. As authoritative researchers advocate lower thresholds for intervention,5,6 asymptomatic people are more likely to be labelled as at risk and needing medical intervention and follow up.
The box gives the most common conditions for which screening is encouraged in primary care. Genetic tests that may help predict some common diseases are likely to be included in the preventive armamentarium before long. To maintain control of the extensive preventive agenda, doctors are advised to “build into their practice a system of reminders and performance feedback to ensure necessary care.”7
The expansion of preventive biomedicine has partly resulted from medical experts and other stakeholders using aggressively assertive and presumptuous arguments.3 It is difficult to challenge the benevolent mission of a preventive programme, and public health authorities have often welcomed such initiatives with more enthusiasm than has been warranted on scientific grounds.
Clinical inertia
In practice, doctors don't always follow clinical guidelines.7–10 This phenomenon has been designated clinical inertia7 and is generally interpreted as a sign of low quality care. Explanations include doctors overestimating the quality of the care they actually provide, lack of training, and use of soft excuses to avoid intervention.7 Lack of time is also a well known explanation. The preventive measures discussed here are rarely effective enough to shift a large load of work away from treatment of manifest disease in the practice population. The total number of consultations will thus increase with the introduction of each new screening routine. A recent estimate shows that 7.4 hours of the working day of an average primary care physician in the United States would be needed to provide all services recommended by the US Preventive Services Task Force.10
Problems of opportunistic screening
Other important but more subtle factors may also contribute to doctors' limited compliance with guidelines on prevention. A clinician may hesitate to implement preventive guidelines because of the challenges of communicating risk.11 Most specialists in preventive medicine show limited interest in the downsides of preventive programmes and early intervention.3,12 The individual's decision about whether to participate should, however, not be regarded as trivial.12 The professional who offers a test carries a considerable responsibility because informed consent presupposes an understanding of the limitations of the programme.13 Every test carries a chance of misclassification of disease and false positive test results that lead to further interventions that do not benefit the patient and may cause harm.12,14 In addition, negative results can give false reassurance.
Furthermore, patients and doctors tend to make different choices depending on the way statistical estimates of potential medical benefit are presented.11,12,15 A 55 year old man may, for instance, be quite interested in an 18% reduction in the relative risk of dying from colorectal cancer but more reluctant if told that screening implies an absolute risk reduction of only 0.014% a year. He might alternatively consider that the likelihood of not dying from colorectal cancer is 99.34% if you are screened and 99.20% if you are not screened (numbers based on data in Kronborg et al16). Unless the doctor is willing to solve this information dilemma by using a simple paternalistic reminder such as, “take the test, it is good for you,” many preventive interventions seem too complex to suit Stott and Davis's “window of opportunity.”2
Conditions screened for in primary care
Hypertension
Coronary heart disease
Obesity
Hypercholesterolaemia
Diabetes
Breast cancer
Colorectal cancer
Cervical cancer
Chlamydia
Osteoporosis
Depression
Dementia
Alcohol misuse
Another factor affecting clinical inertia may be the applicability of research. Doctors who keep abreast of scientific publishing are likely to become nihilistic when reading that interventions which are effective in optimal settings may be of marginal benefit in everyday practice or even do more harm than good.17–19 Implementation of preventive medical measures on a large scale is thus not only becoming technically unmanageable, but a matter of increasing ethical concern in relation to individual patients.19
A final, decisive factor contributing to clinical inertia may be the professional insight that health is affected by factors other than those included in evidence based biomedicine.1,20–23 Measurable pathophysiological disturbances should not necessarily be interpreted as the ultimate cause(s) of disease and suffering. External factors, such as social inequality and destructive human relations, greatly influence health and disease.1,21,23 A focus on biotechnological interventions may divert the dialogue between patient and doctor away from important social and relational issues relevant to health.1,21 It is not necessarily good medicine to focus on the management of bodily risk factors in individuals who ask for help to take control of their lives.
Patient autonomy in preventive medicine
The fall in professional autonomy and power of individual doctors over the past few decades might be expected to have resulted in increased patient autonomy. The ongoing increase in centralised surveillance and corporate power24,25 may, however, unintentionally compromise patient autonomy and quality of preventive care. As the list of accessible preventive tests lengthens and thresholds for intervention are lowered, a doctor who adheres to all recommendations for provision of preventive services may ultimately be able to find something abnormal in everybody.
Relatively few empirical studies have examined the effect of being labelled at risk. The results are contradictory. The professional's preconception is, of course, that information about risk will increase people's sense of control over their lives and ultimately their quality of life. But there is also a potential for risk information to cast shadows of doubt and insecurity over people's lives, which means it may undermine their experience of integrity and health. 8,20
The concept of patient autonomy should be re-examined in light of the rapid expansion of preventive biomedicine.19,26 It obviously embraces a person's freedom to consider, choose, or reject preventive or therapeutic options after receiving sufficient information. Once information about medical risk has been passed on to a person, however, it cannot be retracted. Respect for autonomy should therefore also honour the person's right not to be opportunistically confronted with knowledge about biomedical risks that are unrelated to his or her reasons for seeing the doctor.20
Summary points
Opportunistic disease prevention and health promotion are regarded as part of good primary health care
The number of relevant preventive measures has increased greatly over the past two decades
Decisions about preventive measures need proper discussion about both benefits and harms, which takes time
An extensive preventive agenda may divert the dialogue between patient and doctor away from important social and relational issues relevant to the patient's health
Routine opportunistic preventive initiatives may no longer be ethically justifiable in contemporary Western medicine
Future consultations
Clinical inertia in implementation of preventive medical guidelines should not necessarily be taken as a sign of low quality care. It is time to reconsider the extent to which specific, opportunistic initiatives to prevent disease among asymptomatic individuals should remain a core element of everyday consultations in Western medicine. It is certainly good medical practice to identify, emphasise, and support health promoting resources,27 skills, and activities that have a logical link to the patient's reason for coming to see the doctor. Other opportunistic initiatives may also seem appropriate. Doctors could increase patient autonomy by inviting the patient to introduce a topic rather than using a computerised reminding system. An open ended invitation may be one way to proceed. For example, “It could be that you have been considering other things that might be good for your health? If there is something you would like to discuss, you are welcome.”
We thank the general practitioners at Solvangur Health Centre, Iceland, for encouraging us to write this paper and Anne Luise Kirkengen, Magne Nylenna, Pétur Pétursson, Peter Pritchard, Stefan Hjörleifsson and Steinar Westin for constructive comments.
Contributors and sources: The idea to write this paper arose from discussions at the 12th Nordic Congress in General Practice in Norway, September 2002. The content of general practice was the main topic of the congress, and the authors had central roles as congress president (IH), member of the Nordic reference group (JAS), and key-note speaker (LG). LG has worked for several years in academic general practice and is author of a Norwegian continuing medical education textbook. JAS works as a professor and general practitioner. His research was originally on the epidemiology of cardiovascular risk factors, but recently he has become increasingly interested in the topic of medicalisation. IH works as a GP and associate professor. After her PhD research revealed limited adherence to clinical guidelines in preventive medicine among Norwegian GPs, she went on to address the content of general practice and the role of stake-holders who influence the development of the discipline.
Competing interests: None declared.
References
- 1.Metcalfe D. The crucible. J R Coll Gen Pract 1986;36: 349-54. [PMC free article] [PubMed] [Google Scholar]
- 2.Stott NCH, Davis RH. The exceptional potential in each primary care consultation. J R Coll Gen Pract 1979;29: 201-5. [PMC free article] [PubMed] [Google Scholar]
- 3.Sackett DL. The arrogance of preventive medicine. CMAJ 2002;167: 363-4. [PMC free article] [PubMed] [Google Scholar]
- 4.Skolbekken JA. The risk epidemic in medical journals. Soc Sci Med 1995;40: 291-305. [DOI] [PubMed] [Google Scholar]
- 5.Law MR, Wald NJ. Risk factor thresholds: their existence under scrutiny. BMJ 2002;324: 1570-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ault A. Latest US hypertension guidelines create new “pre-hypertensive” category. Lancet 2003;361: 1798.12781547 [Google Scholar]
- 7.Philips LS, Branch WT, Cook CB, Doyle JP, El-Kebbi IM, Gallina DL, et al. Clinical inertia. Ann Intern Med 2001;135: 825-34. [DOI] [PubMed] [Google Scholar]
- 8.Freeman AC, Sweeney K. Why general practitioners do not implement evidence: a qualitative study. BMJ 2001;323: 1100-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hetlevik I. The role of clinical guidelines in cardiovascular risk intervention in general practice. Dissertation. Trondheim: Bjaerum, 1999.
- 10.Yarnall KSH, Pollack KI, Östbye T, Krause KM, Michener JL. Primary care: is there enough time for prevention? Am J Pub Health 2003;93: 635-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Edwards A, Elwyn G, Mulley A. Explaining risks: turning numerical data into meaningful pictures. BMJ 2002;324: 827-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Welsh HG. Informed choice in cancer screening. JAMA 2001;285: 2776-8. [DOI] [PubMed] [Google Scholar]
- 13.Marteau TM, Kinmonth AL. Screening for cardiovascular risk: public health imperative or a matter of individual informed choice? BMJ 2002;325: 78-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Swensen SJ. Screening for cancer with computed tomography. BMJ 2003;326: 894-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Misselbrook D, Armstrong D. Patient's responses to risk information about benefits of treating hypertension. Br J Gen Pract 2001;51: 276-9. [PMC free article] [PubMed] [Google Scholar]
- 16.Kronborg O, Fenger C, Olsen J, Jörgensen OD, Söndergaard O. Randomised study of screening for colorectal cancer with faecal-occult-blood test. Lancet 1996;348: 1467-71 [DOI] [PubMed] [Google Scholar]
- 17.Raffle AE, Alden B, Quinn M, Babb PJ, Brett MT. Outcomes of screening to prevent cancer: analysis of cumulative incidence of cervical abnormality and modelling of cases and deaths prevented. BMJ 2003;326: 901-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Writing Group for the Women's Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women's Health Initiative randomized controlled trial. JAMA 2002;288: 321-33. [DOI] [PubMed] [Google Scholar]
- 19.Getz L, Kirkengen AL. Ultrasound screening in pregnancy: advancing technology, soft markers for fetal chromosomal aberrations, and unacknowledged ethical dilemmas. Soc Sci Med 2003;56: 2045-57. [DOI] [PubMed] [Google Scholar]
- 20.Getz L, Nilsson PM, Hetlevik I. A matter of heart: the general practitioner consultation in an evidence-based world. Scand J Prim Health Care 2003;21: 3-9. [DOI] [PubMed] [Google Scholar]
- 21.Kirkengen AL. Inscribed bodies: health impact of childhood sexual abuse. Dordrecht: Kluwer Academic Press, 2001.
- 22.Haynes RB, Devereaux PJ, Guyatt GH. Physicians' and patients' choices in evidence based practice. BMJ 2002;324: 1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bracken P. Trauma: culture, meaning and philosophy. London: Whurr, 2002.
- 24.Moynihan R, Heath I, Henry D. Selling sickness: the pharmaceutical industry and disease mongering. BMJ 2002;324: 886-91 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith R. Editor's choice: the screening industry. BMJ 2003;326 (26 April).
- 26.Tauber AI. Historical and philosophical reflections on patient autonomy. Health Care Anal 2001;9: 299-319. [DOI] [PubMed] [Google Scholar]
- 27.Hollnagel H, Malterud K. From risk factors to health resources in medical practice. Med Health Care Philos 2000;3: 257-64. [DOI] [PubMed] [Google Scholar]