Abstract
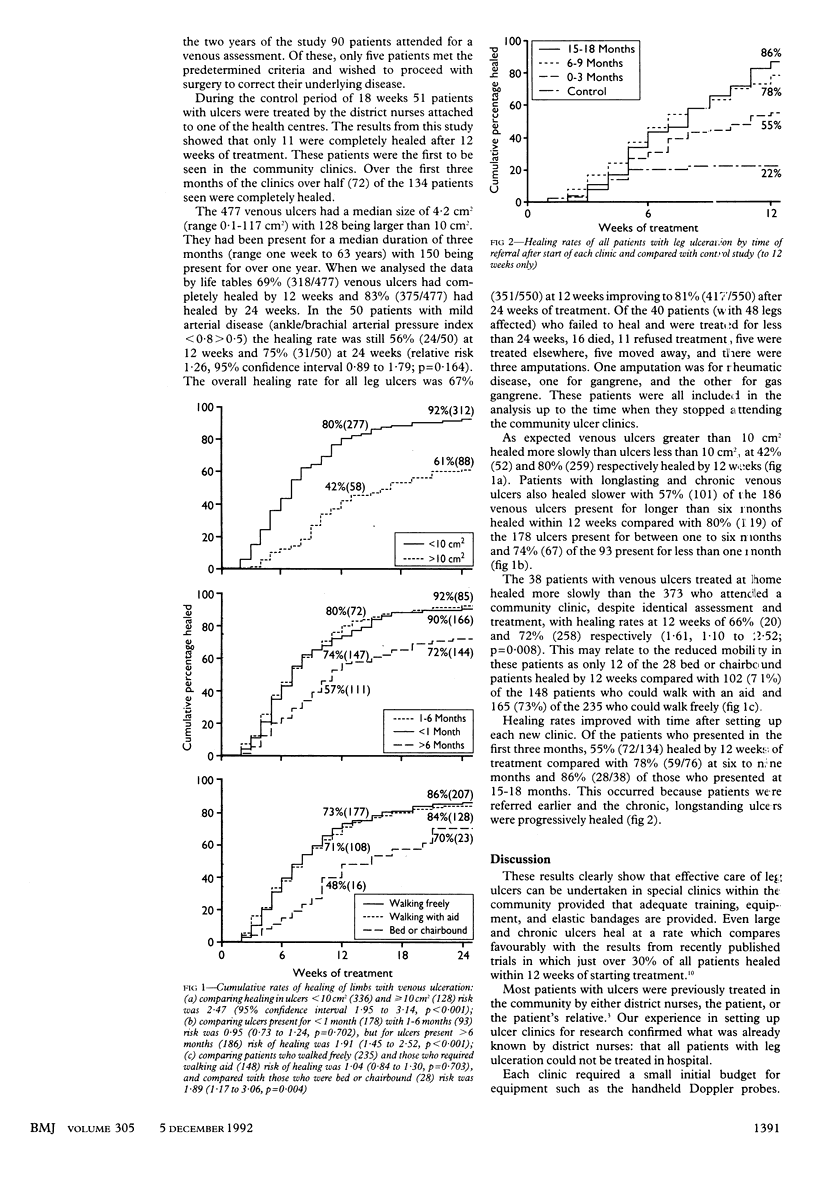
OBJECTIVE--To evaluate the effectiveness of community clinics for leg ulcers. DESIGN--All patients with leg ulceration were invited to community clinics that offered treatment developed in a hospital research clinic. Patients without serious arterial disease (Doppler ankle/brachial index > 0.8) were treated with a high compression bandage of four layers. SETTING--Six community clinics held in health centres in Riverside District Health Authority supported by the Charing Cross vascular surgical service. PATIENTS--All patients referred to the community services with leg ulceration, irrespective of cause and duration of ulceration. MAIN OUTCOME MEASURES--Time to complete healing by the life table method. RESULTS--550 ulcerated legs were seen in 475 patients of mean (SD) age 73.8 (11.9) years. There were 477 venous ulcers of median size 4.2 cm2 (range 0.1-117 cm2), 128 being larger than 10 cm2. These ulcers had been present for a median of three months (range one week to 63 years) with 150 present for over one year. Four layer bandaging in the community clinics achieved complete healing in 318 (69%) venous ulcers by 12 weeks and 375 (83%) by 24 weeks. There were 56 patients with an ankle/brachial arterial pressure index < 0.8, indicating arterial disease. The 50 patients with pressure index < 0.8 > 0.5 were treated with reduced compression, and 24 (56%) healed by 12 weeks and 31 (75%) by 24 weeks. The figures for overall healing for all leg ulcers were 351/550 (67%) at 12 weeks and 417/550 (81%) at 24 weeks, compared with only 11/51 (22%) at 12 weeks before the community clinics were set up. CONCLUSIONS--Community clinics for venous ulcers offer an effective means of achieving healing in most patients with leg ulcers.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Callam M. J., Ruckley C. V., Dale J. J., Harper D. R. Hazards of compression treatment of the leg: an estimate from Scottish surgeons. Br Med J (Clin Res Ed) 1987 Nov 28;295(6610):1382–1382. doi: 10.1136/bmj.295.6610.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callam M. J., Ruckley C. V., Harper D. R., Dale J. J. Chronic ulceration of the leg: extent of the problem and provision of care. Br Med J (Clin Res Ed) 1985 Jun 22;290(6485):1855–1856. doi: 10.1136/bmj.290.6485.1855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colgan M. P., Dormandy J. A., Jones P. W., Schraibman I. G., Shanik D. G., Young R. A. Oxpentifylline treatment of venous ulcers of the leg. BMJ. 1990 Apr 14;300(6730):972–975. doi: 10.1136/bmj.300.6730.972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwall J. V., Doré C. J., Lewis J. D. Leg ulcers: epidemiology and aetiology. Br J Surg. 1986 Sep;73(9):693–696. doi: 10.1002/bjs.1800730905. [DOI] [PubMed] [Google Scholar]
- Lock S. NHS 1948-88: less ideology, more humanity. BMJ. 1988 Jul 2;297(6640):1–3. doi: 10.1136/bmj.297.6640.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poskitt K. R., James A. H., Lloyd-Davies E. R., Walton J., McCollum C. Pinch skin grafting or porcine dermis in venous ulcers: a randomised clinical trial. Br Med J (Clin Res Ed) 1987 Mar 14;294(6573):674–676. doi: 10.1136/bmj.294.6573.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yao S. T., Hobbs J. T., Irvine W. T. Ankle systolic pressure measurements in arterial disease affecting the lower extremities. Br J Surg. 1969 Sep;56(9):676–679. doi: 10.1002/bjs.1800560910. [DOI] [PubMed] [Google Scholar]


