Abstract
Promising research on three new drugs provides hope for chronically infected patients
HIV has an impressive ability to replicate, mutate, and diversify, so developing drugs or vaccines that can fully contain the virus is a challenge. The only consistently successful way to prevent replication of HIV is to administer a potent combination regimen that contains at least two and preferably three antiretroviral drugs. Fortunately, with more than 20 antiretroviral drugs currently available, it is easy to construct such regimens for patients who are treatment naive.
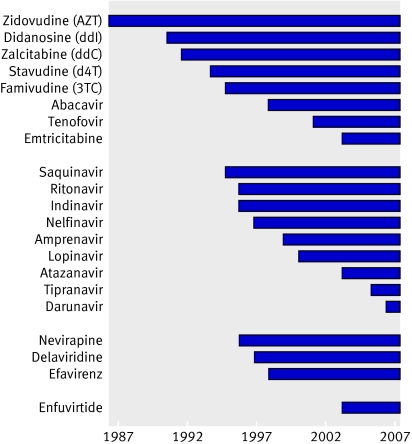
However, a considerable number of patients have not had the chance to achieve full viral suppression despite access to antiretroviral drugs. These people are not well defined, but they generally began monotherapy with zidovudine in the early 1990s, and were sequentially exposed to each new drug as it became available (figure). This sequential use of suboptimal regimens led to the emergence of multidrug resistant HIV. These patients are often referred to as being in “deep salvage” and are at risk for disease progression.
Development of antiretroviral drugs, 1987-2007
This year, we may witness a dramatic shift in how these patients are managed. For the first time in the HIV epidemic, three new agents have been developed for the management of drug resistant virus. They are the HIV integrase inhibitors, R5 inhibitors, and etravirine (TMC125)—a second generation non-nucleoside reverse transcriptase inhibitor. Hence, for patients in deep salvage, 2007 may be comparable to the landmark events of 1996, when the near miraculous effects of combination therapy were first observed. Although caution is needed given the hype that often surrounds any new treatment for HIV, it is nevertheless a time of renewed hope for such patients.
Most of the recent excitement has focused on HIV integrase inhibitors, a novel drug class that prevents integration of HIV DNA into the host genome.1 Two such drugs are actively being developed—raltegravir (MK-0518) and elvitegravir (GS-9137)—with the former now available in expanded access programmes. Interim analyses from two ongoing phase III randomised double blind placebo controlled studies of raltegravir were recently presented at the 14th conference on retroviruses and opportunistic infections.2 3 A planned interim analysis at 16 weeks found that raltegravir was superior to placebo for reducing plasma HIV RNA to fewer than 50 copies/ml (61% v 33%, P<0.001 in BENCHMRK-12; 62% v 36%, P<0.001 in BENCHMRK-23). In a combined analysis of both studies, patients who were not able to include another fully effective agent in their background regimen still benefited from raltegravir based treatment (at 16 weeks, 61% had a plasma HIV RNA below 400 copies/ml compared with 5% in the placebo group). Raltegravir was well tolerated in both studies.
Data on the second novel therapeutic drug class, the R5 inhibitors, were also presented at this conference. All strains of HIV enter CD4 positive T cells via the CCR5 or CXCR4 coreceptor.4 Most patients with early stage disease harbour viruses that enter via the CCR5 coreceptor, whereas up to half of those with advanced disease harbour at least some viruses that enter via the CXCR4 coreceptor.5 6 R5 inhibitors bind to the CCR5 molecule and prevent CCR5 utilising variants from entering cells.
Enthusiasm for this drug class had waned for several reasons. Firstly, many patients in deep salvage harbour viruses that use the CXCR4 and not the CCR5 coreceptor. Secondly, the use of an R5 inhibitor may force a virus to switch from a CCR5 utilising state to a potentially more pathogenic CXCR4 utilising state. Thirdly, unlike other antiretroviral drugs, R5 inhibitors target the host rather than the virus and might therefore be more toxic. Finally, one leading drug candidate was discontinued because of severe liver toxicity.7
All of these concerns were at least partially addressed in two large phase IIb/III studies examining the role of the R5 inhibitor maraviroc in patients in deep salvage. A planned interim analysis at week 24 of MOTIVATE 1 showed that maraviroc was superior to placebo for suppressing plasma HIV RNA to fewer than 50 copies/ml (42.2% maraviroc once daily v 48.5% maraviroc twice daily v 24.6% placebo, P<0.001)8; similar findings were reported for MOTIVATE 2.9 The drug was well tolerated and no hepatic toxicity was seen. Moreover, although maraviroc did select for CXCR4 utilising virus, this was not associated with a quicker short term decline in CD4 positive T cell numbers. Maraviroc received unanimous support from a Food and Drug Advisory (FDA) panel of outside experts on 24 April 2007.
The third agent that is also now available through expanded access programmes is etravirine (TMC125), a second generation non-nucleoside reverse transcriptase inhibitor (NNRTI) that appears to be active against virus that is resistant to the currently available NNRTIs (such as nevirapine and efavirenz). Results of a study of etravirine were reported last year.10 A randomised controlled trial in subjects with documented NNRTI resistance compared etravirine (400 mg or 800 mg twice daily) with an investigator selected background versus a standard of care control regimen. At 48 weeks, the average reduction in HIV RNA was −0.88, −1.01, and −0.14 log10 copies/ml for the etravirine 400 mg, etravirine 800 mg, and control groups, respectively (P<0.05).
So will we see the end of deep salvage in 2007? Certainly not, because not all patients can achieve lifelong viral suppression for several reasons. Each of these drugs has the potential for significant drug-drug interactions, and it is not clear if they can be easily combined. Many patients harbour viruses that use the CXCR4 coreceptor and will not respond to maraviroc or other R5 inhibitors. Many patients treated with first generation NNRTIs have developed viruses that are cross resistant to etravirine (this is particularly true if the Y181C mutation is present).
Finally, it has always been challenging to translate data generated from a highly motivated study population into real world situations. This may be especially true for the integrase inhibitors, as recent data suggest that high level resistance to these drugs emerges rapidly. Despite these concerns, however, we will probably witness in the next year a remarkable transformation in the prognosis of a generation of chronically ill, HIV infected adults, just as we saw in 1996 with patients who were less treatment experienced.
Competing interests: SGD has provided ad hoc consulting for Merck, Tibotec, and Pfizer, who manufacture three of the drugs discussed in this editorial, and has served on a DSMB for Pfizer. HH has none to declare.
Provenance and peer review: Commissioned; not externally peer reviewed.
References
- 1.Hazuda DJ, Felock P, Witmer M, Wolfe A, Stillmock K, Grobler JA, et al. Inhibitors of strand transfer that prevent integration and inhibit HIV-1 replication in cells. Science 2000;287:646-50. [DOI] [PubMed] [Google Scholar]
- 2.Cooper D, Gatell J, Rockstroh J, Katlama C, Yeni P, Lazzarin A, et al. Results from BENCHMRK-1, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: Program and abstracts of the 14th conference on retroviruses and opportunistic infections. Los Angeles, CA, 2007. www.retroconference.org/2007/
- 3.Steigbigel R, Kumar P, Eron J, Schechter M, Markowitz M, Loufty M, et al. Results from BENCHMRK-2, a phase III study evaluating the efficacy and safety of MK-0518, a novel HIV-1 integrase inhibitor, in patients with triple-class resistant virus. In: Program and abstracts of the 14th conference on retroviruses and opportunistic infections. Los Angeles, CA, 2007. www.retroconference.org/2007/
- 4.Moore JP, Kitchen SG, Pugach P, Zack JA. The CCR5 and CXCR4 coreceptors—central to understanding the transmission and pathogenesis of human immunodeficiency virus type 1 infection. AIDS Res Hum Retroviruses 2004;20:111-26. [DOI] [PubMed] [Google Scholar]
- 5.Hunt PW, Harrigan PR, Huang W, Bates M, Williamson DW, McCune JM, et al. Prevalence of CXCR4 tropism among antiretroviral-treated HIV-1-infected patients with detectable viremia. J Infect Dis 2006;194:926-30. [DOI] [PubMed] [Google Scholar]
- 6.Wilkin TJ, Su Z, Kuritzkes DR, Hughes M, Flexner C, Gross R, et al. HIV type 1 chemokine coreceptor use among antiretroviral-experienced patients screened for a clinical trial of a CCR5 inhibitor: AIDS Clinical Trial Group A5211. Clin Infect Dis 2007;44:591-5. [DOI] [PubMed] [Google Scholar]
- 7.GlaxoSmithKline. Statement to HIV patient community: information from GlaxoSmithKline on changes to studies of investigational CCR5 entry inhibitor aplaviroc (GW873140) 15 September 2005. www.hivandhepatitis.com/recent/ad/091405a.html
- 8.Lalezari J, Goodrich J, DeJesus E, Lampiris H, Gulick R, Saag M, et al. Efficacy and safety of maraviroc plus optimized background therapy in viremic ARV-experienced patients infected with CCR5-tropic HIV-1: 24-week results of a phase 2b/3 study in the US and Canada. In: Program and abstracts of the 14th conference on retroviruses and opportunistic infections Los Angeles, CA, 2007. www.retroconference.org/2007/
- 9.Nelson M, Fatkenheuer G, Konourina I, Lazzarin A, Clumeck N, Horban A, et al. Efficacy and safety of maraviroc plus optimized background therapy in viremic ARV-experienced patients infected with CCR5-tropic HIV-1 in Europe, Australia, and North America: 24-week results. In: Program and abstracts of the 14th conference on retroviruses and opportunistic infections Los Angeles, CA, 2007. www.retroconference.org/2007/
- 10.Cohen C, Steinhart CR, Ward DJ, Ruane P, Vingerhoets J, Peeters M, et al. Efficacy and safety results at 48 weeks with the novel NNRTI, TMC125, and impact of baseline resistance on the virologic response in study TMC125-C223. In: Program and abstracts of the XVI international AIDS conference Toronto, Canada, 2006