Abstract
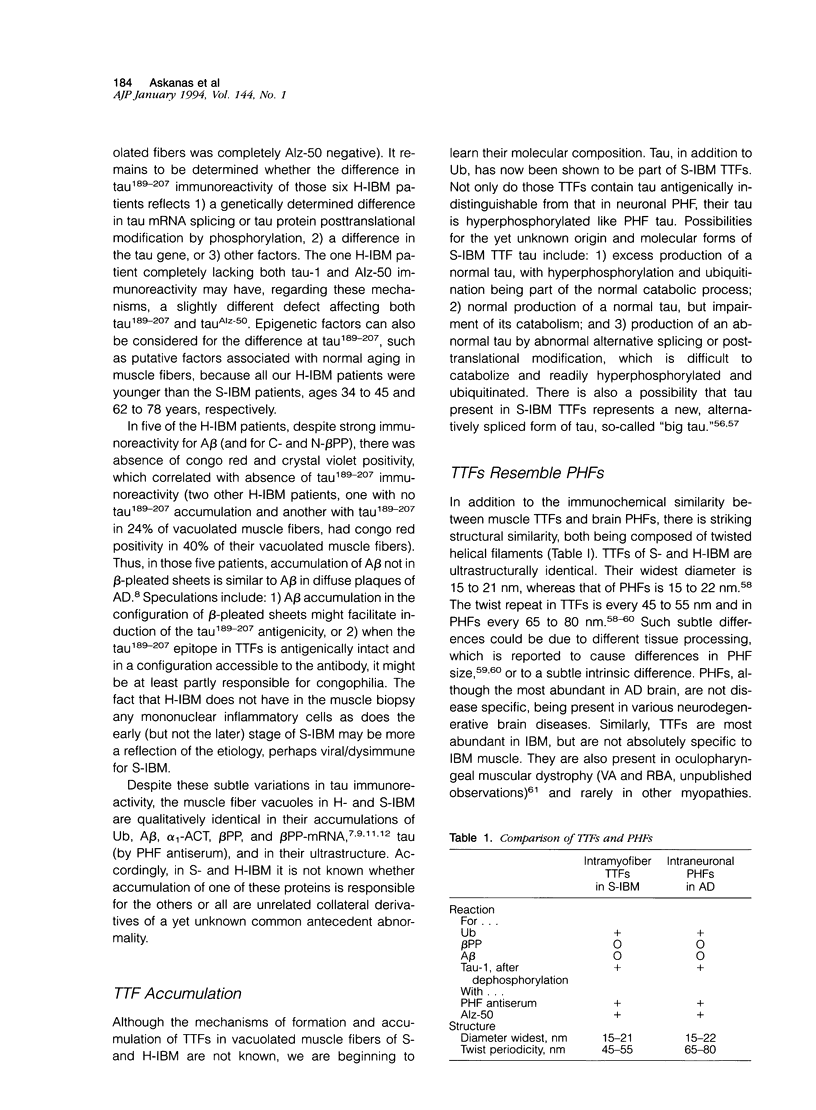
We immunostained muscle biopsies of 8 patients with sporadic inclusion body myositis (S-IBM), 7 patients with autosomal recessive hereditary inclusion body myopathy (H-IBM) (both diseases being characterized by similar muscle fiber vacuoles containing inclusions), and 11 normal and disease controls. We used the following well-characterized antibodies against tau protein: Tau-1, Alz-50, and anti-paired helical filament (PHF) antiserum. By light microscopy, in all S-IBM muscle biopsies virtually all vacuoles immunoreactive for ubiquitin and beta-amyloid protein also contained inclusions immunoreactive with Alz-50 and anti-PHF antiserum. With tau-1 antibody, strong immunoreactivity in the vacuoles was obtained only after dephosphorylation of muscle sections. By electronmicroscopy, all three antibodies immunodecorated exclusively cytoplasmic twisted tubulofilaments (TTFs). In H-IBM, virtually all ubiquitin and beta-amyloid-positive muscle fiber vacuoles contained inclusions immunoreactive with anti-PHF antiserum, but in only 40% of those fibers were the inclusions immunoreactive with Alz-50. In six H-IBM patients there were no tau-1 immunoreactive inclusions in any of their vacuolated muscle fibers; in one patient, 24% of the vacuolated fibers had tau-1 immunoreactivity. By demonstrating that hyperphosphorylated tau, which is characteristic of Alzheimer brain PHFs, is a component of S-IBM-muscle TTFs (which are also ultrastructurally similar to PHFs), our study: 1) provides the first demonstration of abnormally accumulated tau in nonneural tissue and 2) suggests that the cytopathogenesis in Alzheimer brain and S-IBM muscle may share some similar mechanisms. Whether the difference in tau immunoreactivity between S-IBM and most of the H-IBM patients reflects a difference in genetically determined transcriptional or posttranslational modifications of tau protein or other factors remains to be determined.
Full text
PDF








Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Askanas V., Alvarez R. B., Engel W. K. beta-Amyloid precursor epitopes in muscle fibers of inclusion body myositis. Ann Neurol. 1993 Oct;34(4):551–560. doi: 10.1002/ana.410340408. [DOI] [PubMed] [Google Scholar]
- Askanas V., Alvarez R. B. Fast and reliable new method for electron-microscopic identification of cytoplasmic tubulo-filaments in muscle biopsies of patients with inclusion-body myositis. Acta Neuropathol. 1992;84(3):335–336. doi: 10.1007/BF00227829. [DOI] [PubMed] [Google Scholar]
- Askanas V., Engel W. K., Alvarez R. B. Enhanced detection of congo-red-positive amyloid deposits in muscle fibers of inclusion body myositis and brain of Alzheimer's disease using fluorescence technique. Neurology. 1993 Jun;43(6):1265–1267. doi: 10.1212/wnl.43.6.1265-a. [DOI] [PubMed] [Google Scholar]
- Askanas V., Engel W. K., Alvarez R. B., Glenner G. G. beta-Amyloid protein immunoreactivity in muscle of patients with inclusion-body myositis. Lancet. 1992 Feb 29;339(8792):560–561. doi: 10.1016/0140-6736(92)90388-j. [DOI] [PubMed] [Google Scholar]
- Askanas V., Engel W. K., Alvarez R. B. Light and electron microscopic localization of beta-amyloid protein in muscle biopsies of patients with inclusion-body myositis. Am J Pathol. 1992 Jul;141(1):31–36. [PMC free article] [PubMed] [Google Scholar]
- Askanas V., Engel W. K., Alvarez R. B. Strong immunoreactivity of beta-amyloid precursor protein, including the beta-amyloid protein sequence, at human neuromuscular junctions. Neurosci Lett. 1992 Aug 31;143(1-2):96–100. doi: 10.1016/0304-3940(92)90241-x. [DOI] [PubMed] [Google Scholar]
- Askanas V., Engel W. K. Letters to the editor: A technique of fiber selection from human muscle tissue cultures for histochemical-electronmicroscopic studies. J Histochem Cytochem. 1975 Feb;23(2):144–146. doi: 10.1177/23.2.46877. [DOI] [PubMed] [Google Scholar]
- Askanas V., Serdaroglu P., Engel W. K., Alvarez R. B. Immunocytochemical localization of ubiquitin in inclusion body myositis allows its light-microscopic distinction from polymyositis. Neurology. 1992 Feb;42(2):460–461. doi: 10.1212/wnl.42.2.460. [DOI] [PubMed] [Google Scholar]
- Askanas V., Serdaroglu P., Engel W. K., Alvarez R. B. Immunolocalization of ubiquitin in muscle biopsies of patients with inclusion body myositis and oculopharyngeal muscular dystrophy. Neurosci Lett. 1991 Sep 2;130(1):73–76. doi: 10.1016/0304-3940(91)90230-q. [DOI] [PubMed] [Google Scholar]
- Bancher C., Grundke-Iqbal I., Iqbal K., Fried V. A., Smith H. T., Wisniewski H. M. Abnormal phosphorylation of tau precedes ubiquitination in neurofibrillary pathology of Alzheimer disease. Brain Res. 1991 Jan 18;539(1):11–18. doi: 10.1016/0006-8993(91)90681-k. [DOI] [PubMed] [Google Scholar]
- Bilak M., Askanas V., Engel W. K. Strong immunoreactivity of alpha 1-antichymotrypsin co-localizes with beta-amyloid protein and ubiquitin in vacuolated muscle fibers of inclusion-body myositis. Acta Neuropathol. 1993;85(4):378–382. doi: 10.1007/BF00334447. [DOI] [PubMed] [Google Scholar]
- Binder L. I., Frankfurter A., Rebhun L. I. The distribution of tau in the mammalian central nervous system. J Cell Biol. 1985 Oct;101(4):1371–1378. doi: 10.1083/jcb.101.4.1371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brion J. P., Hanger D. P., Couck A. M., Anderton B. H. A68 proteins in Alzheimer's disease are composed of several tau isoforms in a phosphorylated state which affects their electrophoretic mobilities. Biochem J. 1991 Nov 1;279(Pt 3):831–836. doi: 10.1042/bj2790831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brion J. P. The pathology of the neuronal cytoskeleton in Alzheimer's disease. Biochim Biophys Acta. 1992 Nov 10;1160(1):134–142. doi: 10.1016/0167-4838(92)90047-h. [DOI] [PubMed] [Google Scholar]
- Cole A. J., Kuzniecky R., Karpati G., Carpenter S., Andermann E., Andermann F. Familial myopathy with changes resembling inclusion body myositis and periventricular leucoencephalopathy. A new syndrome. Brain. 1988 Oct;111(Pt 5):1025–1037. doi: 10.1093/brain/111.5.1025. [DOI] [PubMed] [Google Scholar]
- Couchie D., Mavilia C., Georgieff I. S., Liem R. K., Shelanski M. L., Nunez J. Primary structure of high molecular weight tau present in the peripheral nervous system. Proc Natl Acad Sci U S A. 1992 May 15;89(10):4378–4381. doi: 10.1073/pnas.89.10.4378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalakas M. C. Polymyositis, dermatomyositis and inclusion-body myositis. N Engl J Med. 1991 Nov 21;325(21):1487–1498. doi: 10.1056/NEJM199111213252107. [DOI] [PubMed] [Google Scholar]
- ENGEL W. K., CUNNINGHAM G. G. RAPID EXAMINATION OF MUSCLE TISSUE. AN IMPROVED TRICHROME METHOD FOR FRESH-FROZEN BIOPSY SECTIONS. Neurology. 1963 Nov;13:919–923. doi: 10.1212/wnl.13.11.919. [DOI] [PubMed] [Google Scholar]
- Engel W. K. Muscle biopsies in neuromuscular diseases. Pediatr Clin North Am. 1967 Nov;14(4):963–995. doi: 10.1016/s0031-3955(16)32067-3. [DOI] [PubMed] [Google Scholar]
- Goedert M., Crowther R. A., Garner C. C. Molecular characterization of microtubule-associated proteins tau and MAP2. Trends Neurosci. 1991 May;14(5):193–199. doi: 10.1016/0166-2236(91)90105-4. [DOI] [PubMed] [Google Scholar]
- Goedert M., Spillantini M. G., Cairns N. J., Crowther R. A. Tau proteins of Alzheimer paired helical filaments: abnormal phosphorylation of all six brain isoforms. Neuron. 1992 Jan;8(1):159–168. doi: 10.1016/0896-6273(92)90117-v. [DOI] [PubMed] [Google Scholar]
- Goedert M., Spillantini M. G., Crowther R. A. Cloning of a big tau microtubule-associated protein characteristic of the peripheral nervous system. Proc Natl Acad Sci U S A. 1992 Mar 1;89(5):1983–1987. doi: 10.1073/pnas.89.5.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goedert M., Spillantini M. G., Jakes R. Localization of the Alz-50 epitope in recombinant human microtubule-associated protein tau. Neurosci Lett. 1991 May 27;126(2):149–154. doi: 10.1016/0304-3940(91)90541-z. [DOI] [PubMed] [Google Scholar]
- Goedert M., Spillantini M. G., Jakes R., Rutherford D., Crowther R. A. Multiple isoforms of human microtubule-associated protein tau: sequences and localization in neurofibrillary tangles of Alzheimer's disease. Neuron. 1989 Oct;3(4):519–526. doi: 10.1016/0896-6273(89)90210-9. [DOI] [PubMed] [Google Scholar]
- Gorycki M. A., Askanas V. Improved technique for electron microscopy of cultured cells. Stain Technol. 1977 Sep;52(5):249–254. doi: 10.3109/10520297709116788. [DOI] [PubMed] [Google Scholar]
- Grundke-Iqbal I., Iqbal K., Tung Y. C., Quinlan M., Wisniewski H. M., Binder L. I. Abnormal phosphorylation of the microtubule-associated protein tau (tau) in Alzheimer cytoskeletal pathology. Proc Natl Acad Sci U S A. 1986 Jul;83(13):4913–4917. doi: 10.1073/pnas.83.13.4913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haass C., Schlossmacher M. G., Hung A. Y., Vigo-Pelfrey C., Mellon A., Ostaszewski B. L., Lieberburg I., Koo E. H., Schenk D., Teplow D. B. Amyloid beta-peptide is produced by cultured cells during normal metabolism. Nature. 1992 Sep 24;359(6393):322–325. doi: 10.1038/359322a0. [DOI] [PubMed] [Google Scholar]
- Ihara Y., Abraham C., Selkoe D. J. Antibodies to paired helical filaments in Alzheimer's disease do not recognize normal brain proteins. Nature. 1983 Aug 25;304(5928):727–730. doi: 10.1038/304727a0. [DOI] [PubMed] [Google Scholar]
- Kosik K. S. Alzheimer's disease: a cell biological perspective. Science. 1992 May 8;256(5058):780–783. doi: 10.1126/science.1589757. [DOI] [PubMed] [Google Scholar]
- Kosik K. S., Orecchio L. D., Binder L., Trojanowski J. Q., Lee V. M., Lee G. Epitopes that span the tau molecule are shared with paired helical filaments. Neuron. 1988 Nov;1(9):817–825. doi: 10.1016/0896-6273(88)90129-8. [DOI] [PubMed] [Google Scholar]
- Kosik K. S. Tau protein and Alzheimer's disease. Curr Opin Cell Biol. 1990 Feb;2(1):101–104. doi: 10.1016/s0955-0674(05)80038-9. [DOI] [PubMed] [Google Scholar]
- Kosik K. S. The molecular and cellular biology of tau. Brain Pathol. 1993 Jan;3(1):39–43. doi: 10.1111/j.1750-3639.1993.tb00724.x. [DOI] [PubMed] [Google Scholar]
- Kowall N. W., Kosik K. S. Axonal disruption and aberrant localization of tau protein characterize the neuropil pathology of Alzheimer's disease. Ann Neurol. 1987 Nov;22(5):639–643. doi: 10.1002/ana.410220514. [DOI] [PubMed] [Google Scholar]
- Ksiezak-Reding H., Binder L. I., Yen S. H. Alzheimer disease proteins (A68) share epitopes with tau but show distinct biochemical properties. J Neurosci Res. 1990 Mar;25(3):420–430. doi: 10.1002/jnr.490250320. [DOI] [PubMed] [Google Scholar]
- Ksiezak-Reding H., Yen S. H. Structural stability of paired helical filaments requires microtubule-binding domains of tau: a model for self-association. Neuron. 1991 May;6(5):717–728. doi: 10.1016/0896-6273(91)90169-z. [DOI] [PubMed] [Google Scholar]
- Lee V. M., Balin B. J., Otvos L., Jr, Trojanowski J. Q. A68: a major subunit of paired helical filaments and derivatized forms of normal Tau. Science. 1991 Feb 8;251(4994):675–678. doi: 10.1126/science.1899488. [DOI] [PubMed] [Google Scholar]
- Lee V. M., Trojanowski J. Q. The disordered neuronal cytoskeleton in Alzheimer's disease. Curr Opin Neurobiol. 1992 Oct;2(5):653–656. doi: 10.1016/0959-4388(92)90034-i. [DOI] [PubMed] [Google Scholar]
- Lotz B. P., Engel A. G., Nishino H., Stevens J. C., Litchy W. J. Inclusion body myositis. Observations in 40 patients. Brain. 1989 Jun;112(Pt 3):727–747. doi: 10.1093/brain/112.3.727. [DOI] [PubMed] [Google Scholar]
- Marx J. Boring in on beta-amyloid's role in Alzheimer's. Science. 1992 Feb 7;255(5045):688–689. doi: 10.1126/science.1738843. [DOI] [PubMed] [Google Scholar]
- Massa R., Weller B., Karpati G., Shoubridge E., Carpenter S. Familial inclusion body myositis among Kurdish-Iranian Jews. Arch Neurol. 1991 May;48(5):519–522. doi: 10.1001/archneur.1991.00530170083024. [DOI] [PubMed] [Google Scholar]
- Mendell J. R., Sahenk Z., Gales T., Paul L. Amyloid filaments in inclusion body myositis. Novel findings provide insight into nature of filaments. Arch Neurol. 1991 Dec;48(12):1229–1234. doi: 10.1001/archneur.1991.00530240033013. [DOI] [PubMed] [Google Scholar]
- Mori H., Kondo J., Ihara Y. Ubiquitin is a component of paired helical filaments in Alzheimer's disease. Science. 1987 Mar 27;235(4796):1641–1644. doi: 10.1126/science.3029875. [DOI] [PubMed] [Google Scholar]
- Neville H. E., Baumbach L. L., Ringel S. P., Russo L. S., Jr, Sujansky E., Garcia C. A. Familial inclusion body myositis: evidence for autosomal dominant inheritance. Neurology. 1992 Apr;42(4):897–902. doi: 10.1212/wnl.42.4.897. [DOI] [PubMed] [Google Scholar]
- Nukina N., Kosik K. S., Selkoe D. J. The monoclonal antibody, Alz 50, recognizes tau proteins in Alzheimer's disease brain. Neurosci Lett. 1988 May 3;87(3):240–246. doi: 10.1016/0304-3940(88)90455-7. [DOI] [PubMed] [Google Scholar]
- Perry G., Friedman R., Shaw G., Chau V. Ubiquitin is detected in neurofibrillary tangles and senile plaque neurites of Alzheimer disease brains. Proc Natl Acad Sci U S A. 1987 May;84(9):3033–3036. doi: 10.1073/pnas.84.9.3033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riley D. A., Bain J. L., Ellis S., Haas A. L. Quantitation and immunocytochemical localization of ubiquitin conjugates within rat red and white skeletal muscles. J Histochem Cytochem. 1988 Jun;36(6):621–632. doi: 10.1177/36.6.2835410. [DOI] [PubMed] [Google Scholar]
- Sarkozi E., Askanas V., Johnson S. A., Engel W. K., Alvarez R. B. beta-Amyloid precursor protein mRNA is increased in inclusion-body myositis muscle. Neuroreport. 1993 Jun;4(6):815–818. doi: 10.1097/00001756-199306000-00055. [DOI] [PubMed] [Google Scholar]
- Selkoe D. J. The molecular pathology of Alzheimer's disease. Neuron. 1991 Apr;6(4):487–498. doi: 10.1016/0896-6273(91)90052-2. [DOI] [PubMed] [Google Scholar]
- Serdaroglu P., Askanas V., Engel W. K. Immunocytochemical localization of ubiquitin at human neuromuscular junctions. Neuropathol Appl Neurobiol. 1992 Jun;18(3):232–236. doi: 10.1111/j.1365-2990.1992.tb00785.x. [DOI] [PubMed] [Google Scholar]
- Tabaton M., Cammarata S., Mancardi G., Manetto V., Autilio-Gambetti L., Perry G., Gambetti P. Ultrastructural localization of beta-amyloid, tau, and ubiquitin epitopes in extracellular neurofibrillary tangles. Proc Natl Acad Sci U S A. 1991 Mar 15;88(6):2098–2102. doi: 10.1073/pnas.88.6.2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabaton M., Mandybur T. I., Perry G., Onorato M., Autilio-Gambetti L., Gambetti P. The widespread alteration of neurites in Alzheimer's disease may be unrelated to amyloid deposition. Ann Neurol. 1989 Dec;26(6):771–778. doi: 10.1002/ana.410260614. [DOI] [PubMed] [Google Scholar]
- Trojanowski J. Q., Schmidt M. L., Shin R. W., Bramblett G. T., Rao D., Lee V. M. Altered tau and neurofilament proteins in neuro-degenerative diseases: diagnostic implications for Alzheimer's disease and Lewy body dementias. Brain Pathol. 1993 Jan;3(1):45–54. doi: 10.1111/j.1750-3639.1993.tb00725.x. [DOI] [PubMed] [Google Scholar]
- Villanova M., Kawai M., Lübke U., Oh S. J., Perry G., Six J., Ceuterick C., Martin J. J., Cras P. Rimmed vacuoles of inclusion body myositis and oculopharyngeal muscular dystrophy contain amyloid precursor protein and lysosomal markers. Brain Res. 1993 Feb 19;603(2):343–347. doi: 10.1016/0006-8993(93)91260-y. [DOI] [PubMed] [Google Scholar]
- Vincent I. J., Davies P. Phosphorylation characteristics of the A68 protein in Alzheimer's disease. Brain Res. 1990 Oct 29;531(1-2):127–135. doi: 10.1016/0006-8993(90)90765-4. [DOI] [PubMed] [Google Scholar]
- Wischik C. M., Crowther R. A., Stewart M., Roth M. Subunit structure of paired helical filaments in Alzheimer's disease. J Cell Biol. 1985 Jun;100(6):1905–1912. doi: 10.1083/jcb.100.6.1905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wisniewski H. M., Merz P. A., Iqbal K. Ultrastructure of paired helical filaments of Alzheimer's neurofibrillary tangle. J Neuropathol Exp Neurol. 1984 Nov;43(6):643–656. doi: 10.1097/00005072-198411000-00008. [DOI] [PubMed] [Google Scholar]
- Wolozin B. L., Pruchnicki A., Dickson D. W., Davies P. A neuronal antigen in the brains of Alzheimer patients. Science. 1986 May 2;232(4750):648–650. doi: 10.1126/science.3083509. [DOI] [PubMed] [Google Scholar]
- Wong C. W., Quaranta V., Glenner G. G. Neuritic plaques and cerebrovascular amyloid in Alzheimer disease are antigenically related. Proc Natl Acad Sci U S A. 1985 Dec;82(24):8729–8732. doi: 10.1073/pnas.82.24.8729. [DOI] [PMC free article] [PubMed] [Google Scholar]






