Abstract
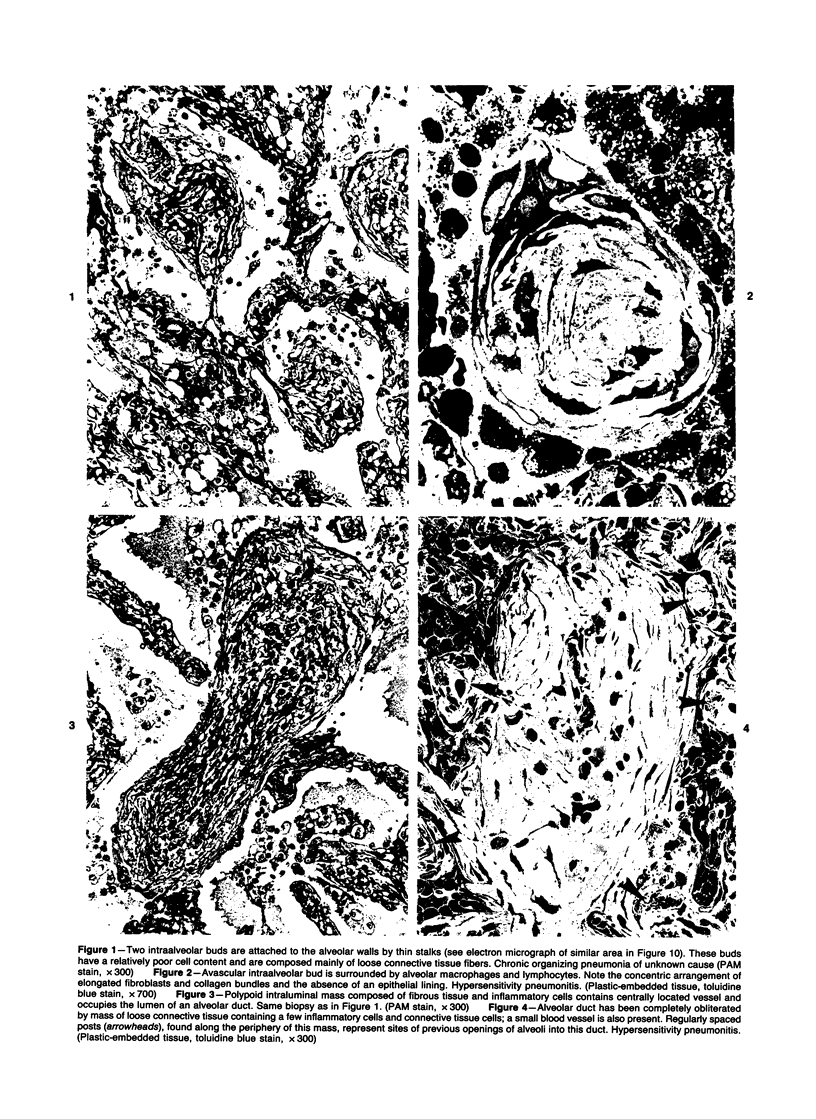
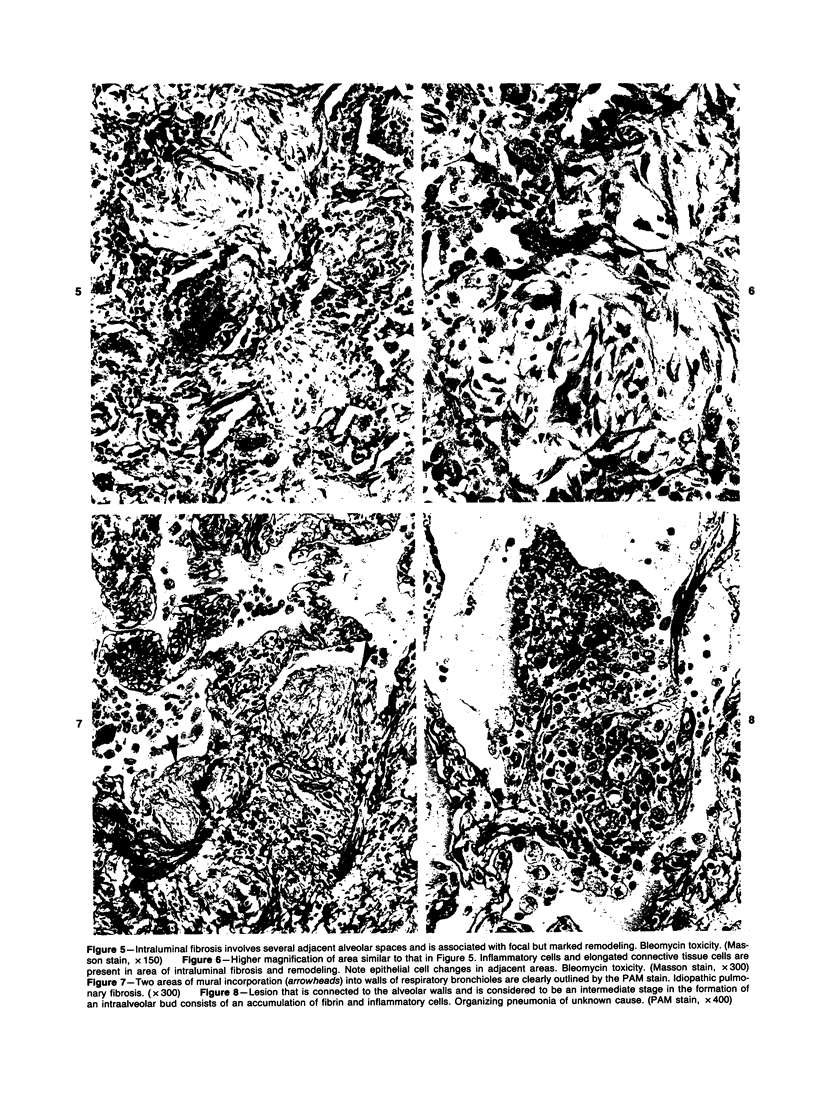
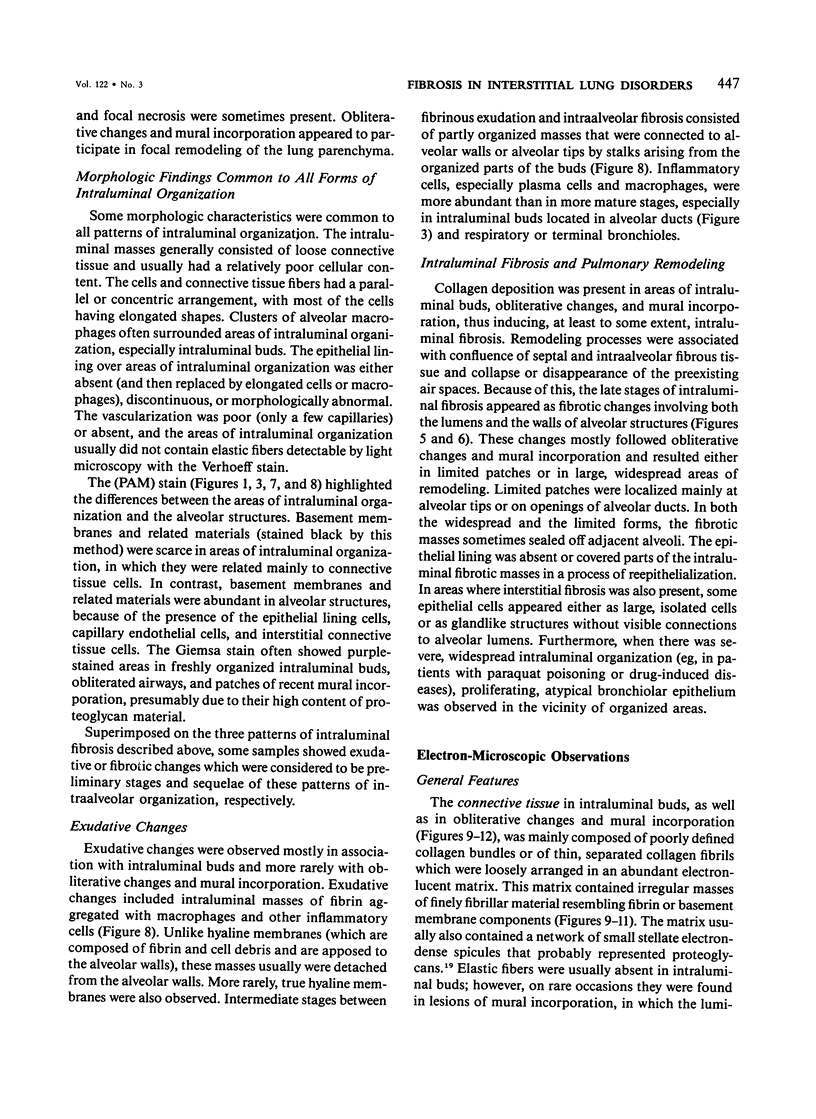
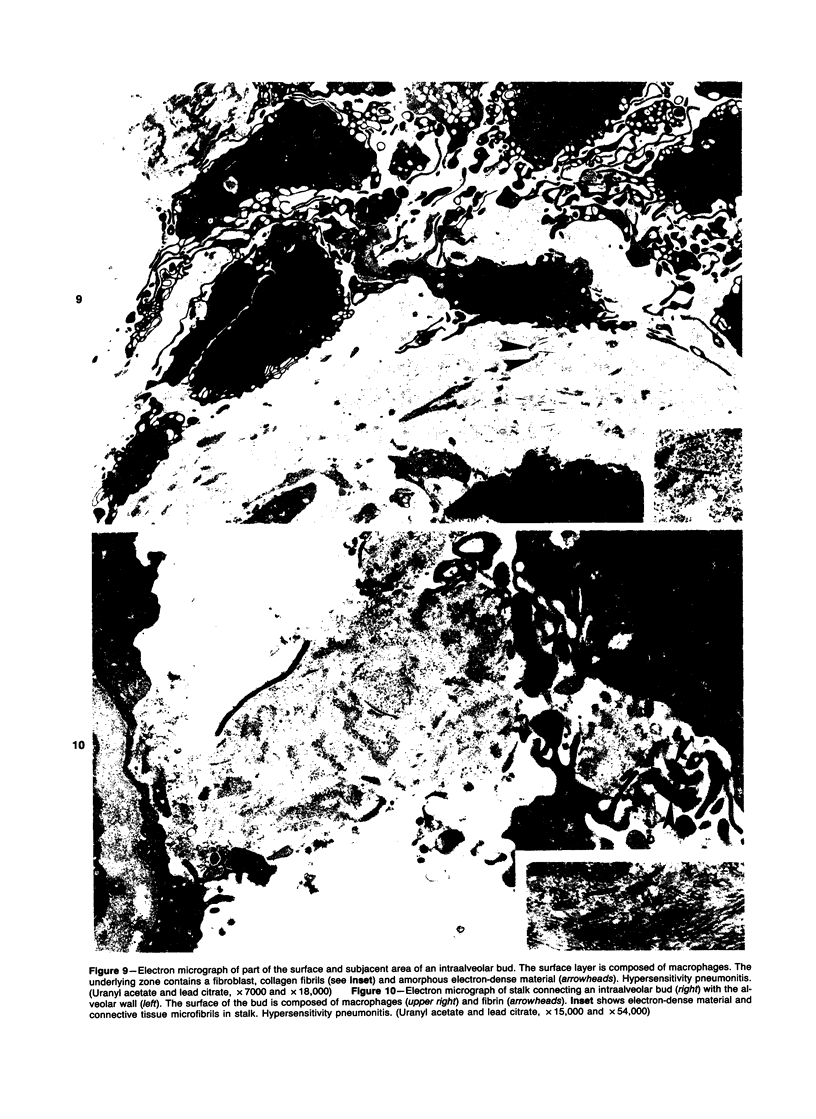
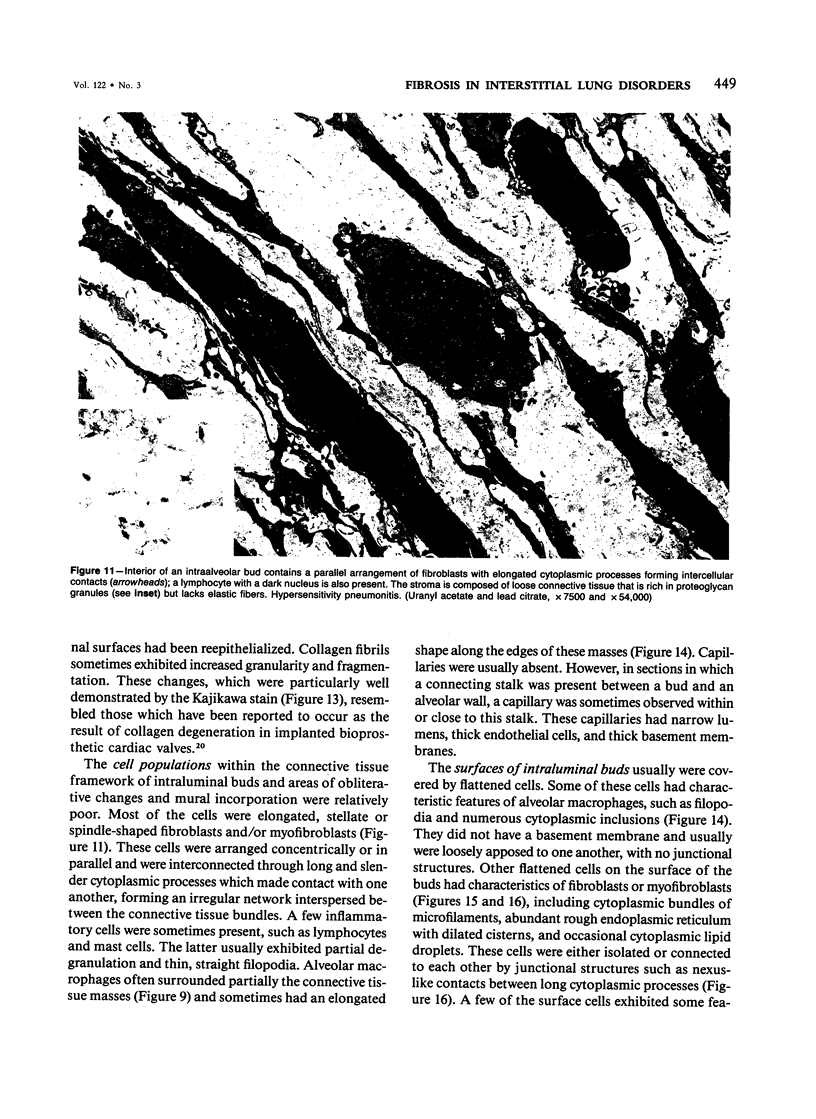
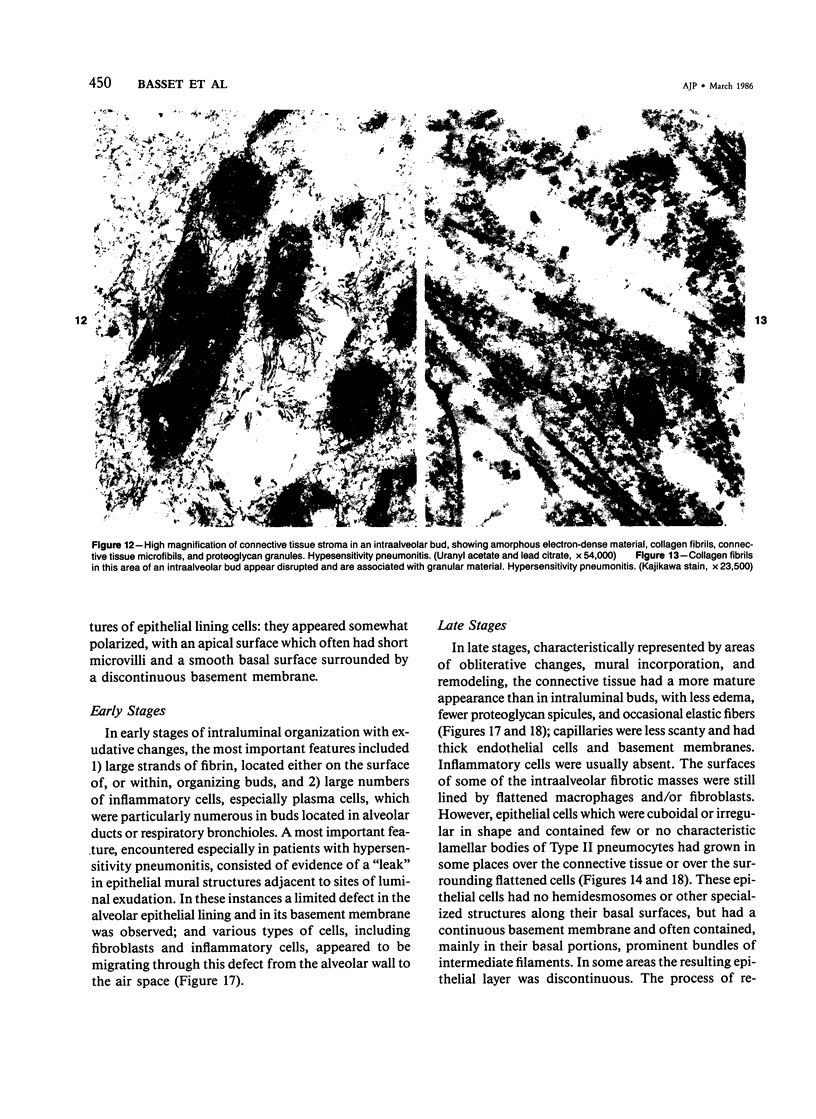
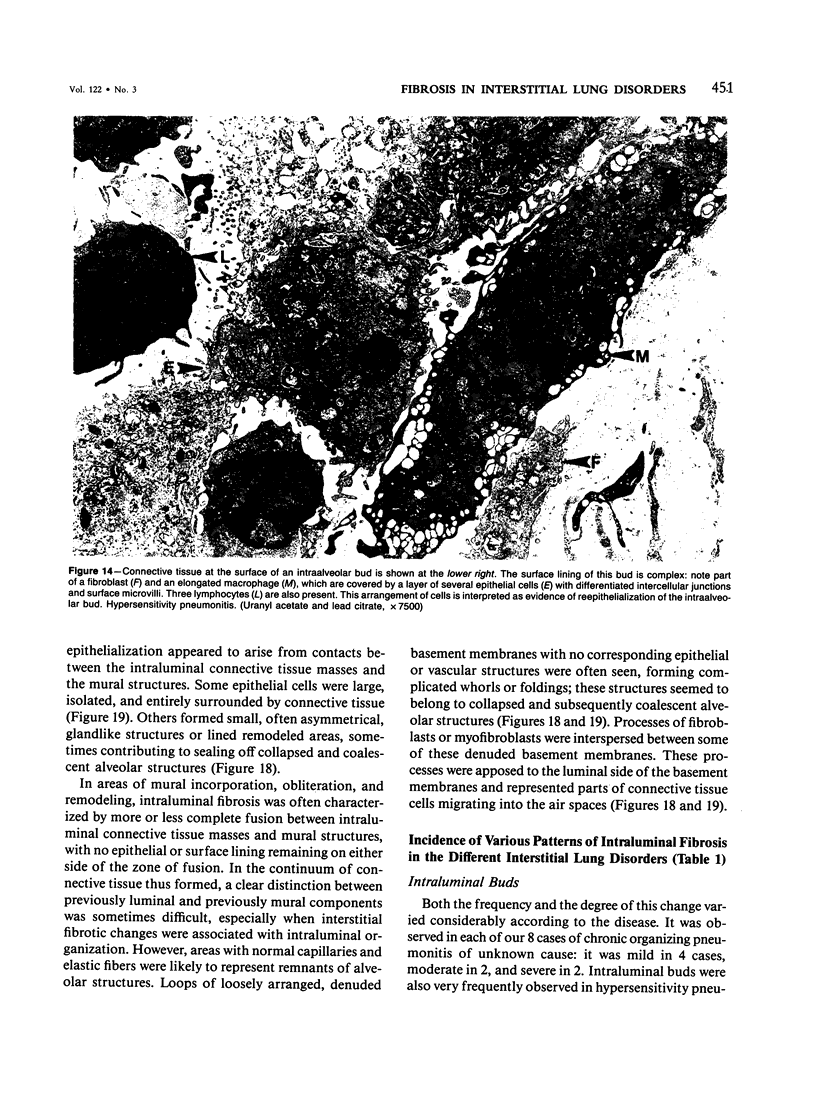
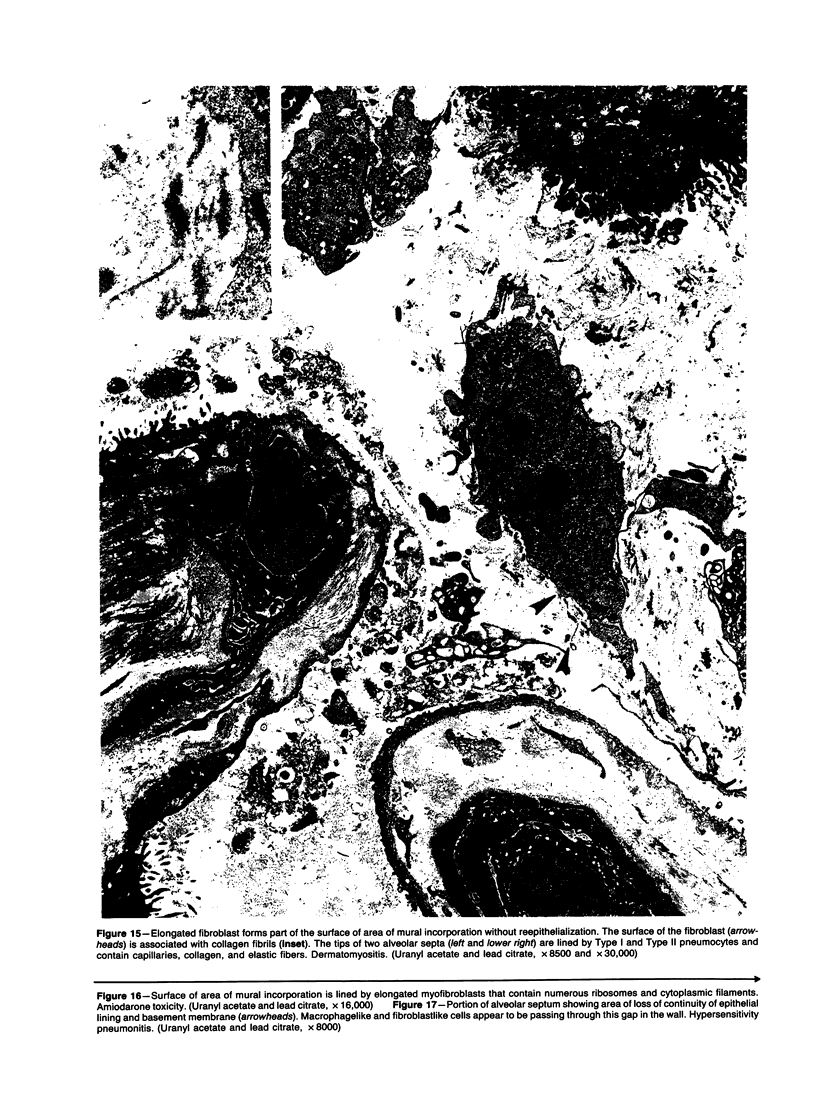
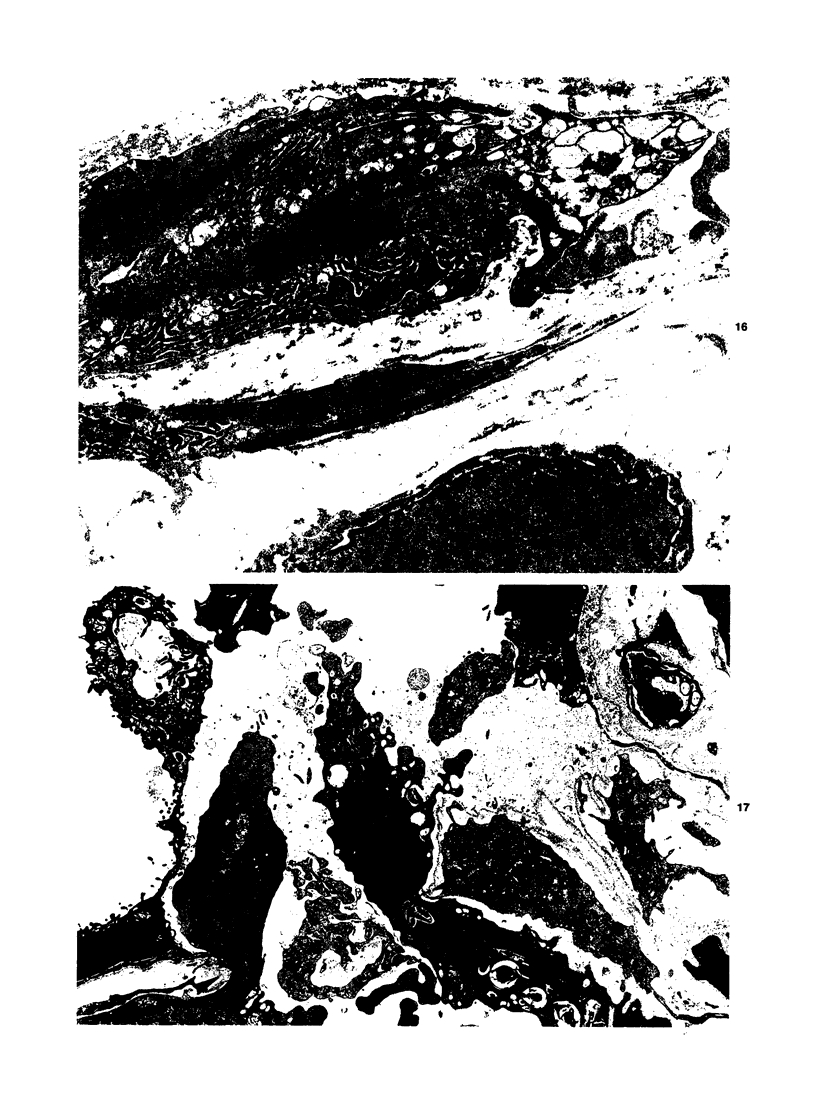
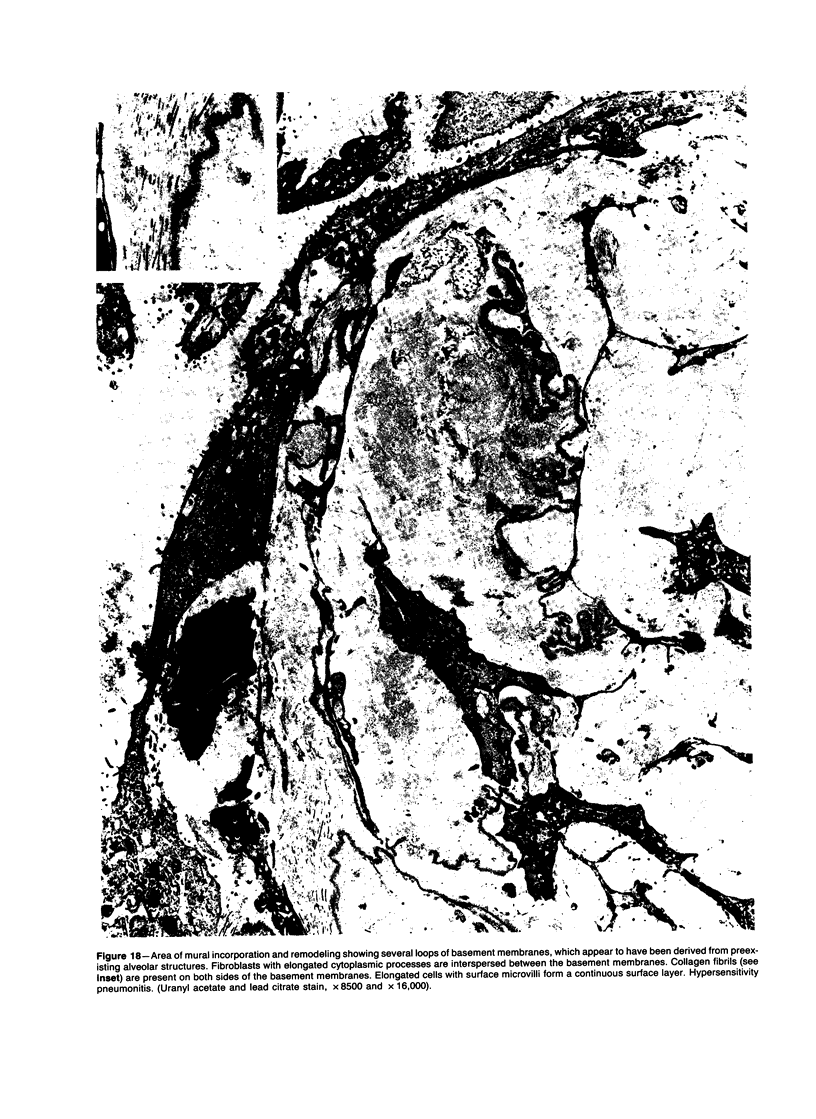
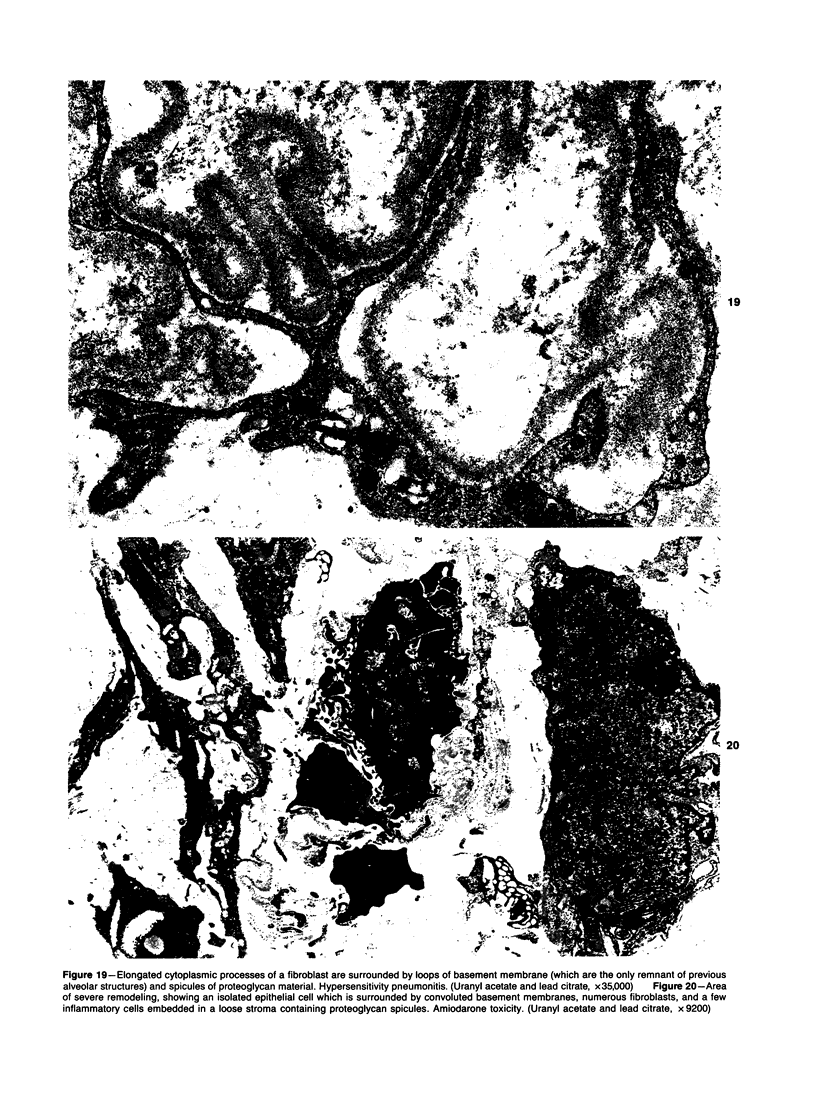
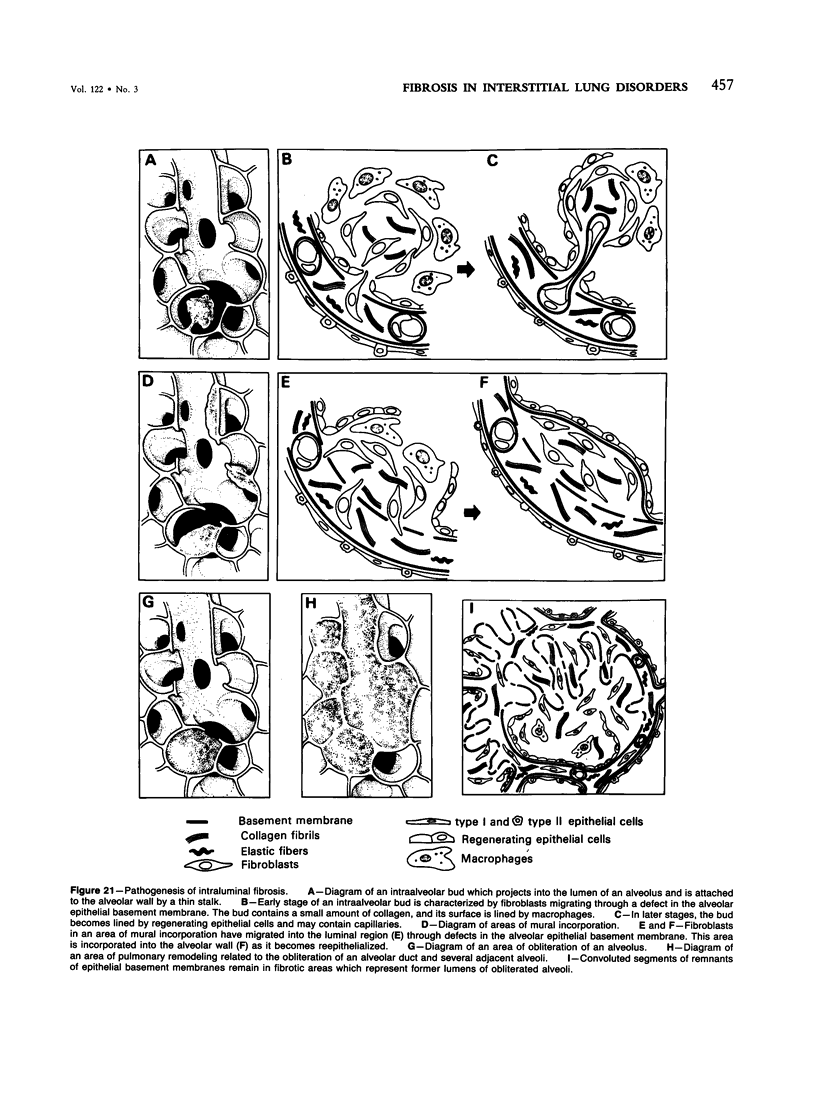
The histopathologic and ultrastructural features of intraluminal organizing and fibrotic changes were studied in open lung biopsies and autopsy specimens from 373 patients with interstitial lung disorders, including hypersensitivity pneumonitis (n = 44), idiopathic pulmonary fibrosis (n = 92), collagen-vascular diseases (n = 20), chronic eosinophilic pneumonia (n = 10), pulmonary histiocytosis X (n-90), pulmonary sarcoidosis (n = 62), pneumoconioses (n = 25), Legionnaire's disease (n = 5), drug- and toxin-induced pneumonitis (n = 4), radiation-induced pneumonitis (n = 2), lymphangioleiomyomatosis (n = 11), and chronic organizing pneumonia of unknown cause (n = 8). Three patterns of intraluminal organization and fibrosis were recognized: 1) intraluminal buds, which partially filled the alveoli, alveolar ducts and/or distal bronchioles; 2) obliterative changes, in which loose connective tissue masses obliterated the lumens of alveoli, alveolar ducts or distal bronchioles, and 3) mural incorporation of previously intraluminal connective tissue masses, which fused with alveolar, alveolar ductal, or bronchiolar structures and frequently became reepithelialized. All three patterns had common morphologic features, suggesting that, regardless of their severity, they resulted from a common pathogenetic mechanism, ie, the migration of activated connective tissue cells, through defects in the epithelial lining and its basement membrane, from the interstitial into the intraluminal compartment. Intraluminal buds were observed most frequently in hypersensitivity pneumonitis, chronic eosinophilic pneumonia, and organizing pneumonia of unknown cause. Mural incorporation and, to a lesser extent, obliterative changes were observed in most interstitial disorders and were very prominent in idiopathic pulmonary fibrosis. Mural incorporation and obliterative changes play an important role in pulmonary remodeling, especially when several adjacent alveoli and/or other air spaces are involved. Under these circumstances, intraluminal organization can mediate the fusion of adjacent alveolar structures by intraluminal connective tissue.
Full text
PDF

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- AUERBACH S. H., MIMS O. M., GOODPASTURE E. W. Pulmonary fibrosis secondary to pneumonia. Am J Pathol. 1952 Jan-Feb;28(1):69–87. [PMC free article] [PubMed] [Google Scholar]
- Azizirad H., Polgar G., Borns P. F., Chatten J. Bronchiolitis obliterans. Clin Pediatr (Phila) 1975 Jun;14(6):572-7, 582-4. doi: 10.1177/000992287501400610. [DOI] [PubMed] [Google Scholar]
- Basset F., Corrin B., Spencer H., Lacronique J., Roth C., Soler P., Battesti J. P., Georges R., Chrétien J. Pulmonary histiocytosis X. Am Rev Respir Dis. 1978 Nov;118(5):811–820. doi: 10.1164/arrd.1978.118.5.811. [DOI] [PubMed] [Google Scholar]
- Bitterman P. B., Rennard S. I., Adelberg S., Crystal R. G. Role of fibronectin as a growth factor for fibroblasts. J Cell Biol. 1983 Dec;97(6):1925–1932. doi: 10.1083/jcb.97.6.1925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackmon J. A., Harley R. A., Hicklin M. D., Chandler F. W. Pulmonary sequelae of acute Legionnaires' disease pneumonia. Ann Intern Med. 1979 Apr;90(4):552–554. doi: 10.7326/0003-4819-90-4-552. [DOI] [PubMed] [Google Scholar]
- Bowden D. H. Alveolar response to injury. Thorax. 1981 Nov;36(11):801–804. doi: 10.1136/thx.36.11.801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brooks R. E. Ultrastructure of lung lesions produced by ingested chemicals. I. Effect of the herbicide paraquat on mouse lung. Lab Invest. 1971 Dec;25(6):536–545. [PubMed] [Google Scholar]
- Carrington C. B. Organizing interstitial pneumonia. Definition of the lesion and attempts to devise an experimental model. Yale J Biol Med. 1968 Apr-Jun;40(5-6):352–363. [PMC free article] [PubMed] [Google Scholar]
- Charan N. B., Myers C. G., Lakshminarayan S., Spencer T. M. Pulmonary injuries associated with acute sulfur dioxide inhalation. Am Rev Respir Dis. 1979 Apr;119(4):555–560. doi: 10.1164/arrd.1979.119.4.555. [DOI] [PubMed] [Google Scholar]
- Coalson J. J. The ultrastructure of human fibrosing alveolitis. Virchows Arch A Pathol Anat Histol. 1982;395(2):181–199. doi: 10.1007/BF00429611. [DOI] [PubMed] [Google Scholar]
- Cooney T. P. Interrelationship of chronic eosinophilic pneumonia, bronchiolitis obliterans, and rheumatoid disease: a hypothesis. J Clin Pathol. 1981 Feb;34(2):129–137. doi: 10.1136/jcp.34.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crystal R. G., Bitterman P. B., Rennard S. I., Hance A. J., Keogh B. A. Interstitial lung diseases of unknown cause. Disorders characterized by chronic inflammation of the lower respiratory tract (first of two parts). N Engl J Med. 1984 Jan 19;310(3):154–166. doi: 10.1056/NEJM198401193100304. [DOI] [PubMed] [Google Scholar]
- Crystal R. G., Bitterman P. B., Rennard S. I., Hance A. J., Keogh B. A. Interstitial lung diseases of unknown cause. Disorders characterized by chronic inflammation of the lower respiratory tract. N Engl J Med. 1984 Jan 26;310(4):235–244. doi: 10.1056/NEJM198401263100406. [DOI] [PubMed] [Google Scholar]
- Davison A. G., Heard B. E., McAllister W. A., Turner-Warwick M. E. Cryptogenic organizing pneumonitis. Q J Med. 1983 Summer;52(207):382–394. [PubMed] [Google Scholar]
- Dearden L. C., Fairshter R. D., McRae D. M., Smith W. R., Glauser F. L., Wilson A. F. Pulmonary ultrastructure of the late aspects of human paraquat poisoning. Am J Pathol. 1978 Dec;93(3):667–680. [PMC free article] [PubMed] [Google Scholar]
- Epler G. R., Colby T. V., McLoud T. C., Carrington C. B., Gaensler E. A. Bronchiolitis obliterans organizing pneumonia. N Engl J Med. 1985 Jan 17;312(3):152–158. doi: 10.1056/NEJM198501173120304. [DOI] [PubMed] [Google Scholar]
- Epler G. R., Colby T. V. The spectrum of bronchiolitis obliterans. Chest. 1983 Feb;83(2):161–162. doi: 10.1378/chest.83.2.161. [DOI] [PubMed] [Google Scholar]
- Epler G. R., Snider G. L., Gaensler E. A., Cathcart E. S., FitzGerald M. X., Carrington C. B. Bronchiolitis and bronchitis in connective tissue disease. A possible relationship to the use of penicillamine. JAMA. 1979 Aug 10;242(6):528–532. [PubMed] [Google Scholar]
- Ferrans V. J., Spray T. L., Billingham M. E., Roberts W. C. Structural changes in glutaraldehyde-treated porcine heterografts used as substitute cardiac valves. Transmission and scanning electron microscopic observations in 12 patients. Am J Cardiol. 1978 Jun;41(7):1159–1184. doi: 10.1016/0002-9149(78)90873-1. [DOI] [PubMed] [Google Scholar]
- Fox B., Seed W. A. Chronic eosinophilic pneumonia. Thorax. 1980 Aug;35(8):570–580. doi: 10.1136/thx.35.8.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fukuda Y., Ferrans V. J., Schoenberger C. I., Rennard S. I., Crystal R. G. Patterns of pulmonary structural remodeling after experimental paraquat toxicity. The morphogenesis of intraalveolar fibrosis. Am J Pathol. 1985 Mar;118(3):452–475. [PMC free article] [PubMed] [Google Scholar]
- Geddes D. M., Corrin B., Brewerton D. A., Davies R. J., Turner-Warwick M. Progressive airway obliteration in adults and its association with rheumatoid disease. Q J Med. 1977 Oct;46(184):427–444. [PubMed] [Google Scholar]
- Geraads A., Brambilla E., Hohn B., Piton J. L., Blanc-Jouvan F., Kamel A. Polyarthrite rhumatoïde, bronchiolite oblitérante et D-penicillamine. A propos d'un nouveau cas avec examen ultrastructural et revue de la littérature. Poumon Coeur. 1983;39(5):257–262. [PubMed] [Google Scholar]
- Goldstein J. D., Godleski J. J., Balikian J. P., Herman P. G. Pathologic patterns of Serratia marcescens pneumonia. Hum Pathol. 1982 May;13(5):479–484. doi: 10.1016/s0046-8177(82)80031-2. [DOI] [PubMed] [Google Scholar]
- Grinblat J., Mechlis S., Lewitus Z. Organizing pneumonia-like process: an unusual observation in steroid responsive cases with features of chronic interstitial pneumonia. Chest. 1981 Sep;80(3):259–263. doi: 10.1378/chest.80.3.259. [DOI] [PubMed] [Google Scholar]
- Hawley P. C., Whitcomb M. E. Bronchiolitis fibrosa obliterans in adults. Arch Intern Med. 1981 Sep;141(10):1324–1327. [PubMed] [Google Scholar]
- Herbut P. A., Manges W. E. The "Masson Body" in Rheumatic Pneumonia. Am J Pathol. 1945 Jul;21(4):741–751. [PMC free article] [PubMed] [Google Scholar]
- Herzog C. A., Miller R. R., Hoidal J. R. Bronchiolitis and rheumatoid arthritis. Am Rev Respir Dis. 1981 Nov;124(5):636–639. doi: 10.1164/arrd.1981.124.5.636. [DOI] [PubMed] [Google Scholar]
- Kajikawa K., Yamaguchi T., Katsuda S., Miwa A. An improved electron stain for elastic fibers using tannic acid. J Electron Microsc (Tokyo) 1975;24(4):287–289. [PubMed] [Google Scholar]
- Kawanami O., Basset F., Barrios R., Lacronique J. G., Ferrans V. J., Crystal R. G. Hypersensitivity pneumonitis in man. Light- and electron-microscopic studies of 18 lung biopsies. Am J Pathol. 1983 Mar;110(3):275–289. [PMC free article] [PubMed] [Google Scholar]
- Kawanami O., Ferrans V. J., Crystal R. G. Structure of alveolar epithelial cells in patients with fibrotic lung disorders. Lab Invest. 1982 Jan;46(1):39–53. [PubMed] [Google Scholar]
- Kelly D. F., Morgan D. G., Darke P. G., Gibbs C., Pearson H., Weaver B. M. Pathology of acute respiratory distress in the dog associated with paraquat poisoning. J Comp Pathol. 1978 Apr;88(2):275–294. [PubMed] [Google Scholar]
- Kinney W. W., Angelillo V. A. Bronchiolitis in systemic lupus erythematosus. Chest. 1982 Nov;82(5):646–649. doi: 10.1378/chest.82.5.646. [DOI] [PubMed] [Google Scholar]
- Massumi R. A., Legier J. F. Rheumatic pneumonitis. Circulation. 1966 Mar;33(3):417–425. doi: 10.1161/01.cir.33.3.417. [DOI] [PubMed] [Google Scholar]
- Matthay R. A., Schwarz M. I., Petty T. L., Stanford R. E., Gupta R. C., Sahn S. A., Steigerwald J. C. Pulmonary manifestations of systemic lupus erythematosus: review of twelve cases of acute lupus pneumonitis. Medicine (Baltimore) 1975 Sep;54(5):397–409. doi: 10.1097/00005792-197509000-00003. [DOI] [PubMed] [Google Scholar]
- Matthew H., Logan A., Woodruff M. F., Heard B. Paraquat poisoning--lung transplantation. Br Med J. 1968 Sep 28;3(5621):759–763. doi: 10.1136/bmj.3.5621.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy K. C., Atkins C. J., Offer R. C., Hogg J. C., Stein H. B. Obliterative bronchiolitis in two rheumatoid arthritis patients treated with penicillamine. Arthritis Rheum. 1981 Mar;24(3):557–560. doi: 10.1002/art.1780240318. [DOI] [PubMed] [Google Scholar]
- Murray R. E., Gibson J. E. A comparative study of paraquat intoxication in rats, guinea pigs and monkeys. Exp Mol Pathol. 1972 Dec;17(3):317–325. doi: 10.1016/0014-4800(72)90044-5. [DOI] [PubMed] [Google Scholar]
- Rebello G., Mason J. K. Pulmonary histological appearances in fatal paraquat poisoning. Histopathology. 1978 Jan;2(1):53–66. doi: 10.1111/j.1365-2559.1978.tb01693.x. [DOI] [PubMed] [Google Scholar]
- Rinaldo J. E., Rogers R. M. Adult respiratory-distress syndrome: changing concepts of lung injury and repair. N Engl J Med. 1982 Apr 15;306(15):900–909. doi: 10.1056/NEJM198204153061504. [DOI] [PubMed] [Google Scholar]
- Schwarz M. I., Matthay R. A., Sahn S. A., Stanford R. E., Marmorstein B. L., Scheinhorn D. J. Interstitial lung disease in polymyositis and dermatomyositis: analysis of six cases and review of the literature. Medicine (Baltimore) 1976 Jan;55(1):89–104. doi: 10.1097/00005792-197601000-00005. [DOI] [PubMed] [Google Scholar]
- Seggev J. S., Mason U. G., 3rd, Worthen S., Stanford R. E., Fernandez E. Bronchiolitis obliterans. Report of three cases with detailed physiologic studies. Chest. 1983 Feb;83(2):169–174. doi: 10.1378/chest.83.2.169. [DOI] [PubMed] [Google Scholar]
- Seidenfeld J. J., Wycoff D., Zavala D. C., Richerson H. B. Paraquat lung injury in rabbits. Br J Ind Med. 1978 Aug;35(3):245–257. doi: 10.1136/oem.35.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P., Heath D. Paraquat lung: a reappraisal. Thorax. 1974 Nov;29(6):643–653. doi: 10.1136/thx.29.6.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith P., Heath D. The pathology of the lung in paraquat poisoning. J Clin Pathol Suppl (R Coll Pathol) 1975;9:81–93. [PMC free article] [PubMed] [Google Scholar]
- Toner P. G., Vetters J. M., Spilg W. G., Harland W. A. Fine structure of the lung lesion in a case of paraquat poisoning. J Pathol. 1970 Nov;102(3):182–185. doi: 10.1002/path.1711020311. [DOI] [PubMed] [Google Scholar]
- Tukiainen P., Poppius H., Taskinen E. Slowly progressive bronchiolitis obliterans. A case report with detailed pulmonary function studies. Eur J Respir Dis. 1980 Apr;61(2):77–83. [PubMed] [Google Scholar]
- Vijeyaratnam G. S., Corrin B. Experimental paraquat poisoning: a histological and electron-optical study of the changes in the lung. J Pathol. 1971 Feb;103(2):123–129. doi: 10.1002/path.1711030207. [DOI] [PubMed] [Google Scholar]