Abstract
Objective—To investigate the effects of cuirass negative pressure ventilation on the cardiac output of a group of anaesthetised children after occlusion of an asymptomatic persistent arterial duct, and a group of paediatric patients in the early postoperative period following cardiopulmonary bypass. Design—Prospective study. Setting—The paediatric intensive care unit and catheter laboratory of a tertiary care centre. Patients—16 mechanically ventilated children were studied: seven had undergone surgery for congenital heart disease, and nine cardiac catheterisation for transcatheter occlusion of an isolated asymptomatic persistent arterial duct. Interventions—Cardiac output was measured using the direct Fick method during intermittent positive pressure ventilation and again after a short period of negative pressure ventilation. In five of the postoperative patients a third measurement was made following reinstitution of positive pressure ventilation. Results—Negative pressure ventilation was delivered without complication, with no significant change in systemic arterial oxygen and carbon dioxide tension. The mixed venous saturation increased from 74% to 75.8% in the healthy children, and from 58.9% to 62.3% in the postoperative group. Negative pressure ventilation increased the cardiac index from 4.0 to 4.5 l/min/m2 in the healthy children, and from 2.8 to 3.5 l/min/m2 in the surgical group. The increase was significantly higher in the postoperative patients (28.1%) than the healthy children (10.8%). Conclusions—While offering similar ventilatory efficiency to positive pressure ventilation, cuirass negative pressure ventilation led to a modest improvement in the cardiac output of healthy children, and to a greater increase in postoperative patients. There are important cardiopulmonary interactions in normal children and in children after cardiopulmonary bypass, and by having beneficial effects on these interactions, negative pressure ventilation has haemodynamic advantages over conventional positive pressure ventilation. Keywords: cardiopulmonary interactions; congenital heart disease; ventilation; children
Full Text
The Full Text of this article is available as a PDF (147.4 KB).
Figure 1 .
Cuirass negative pressure ventilation in a postoperative patient who was studied four hours after closure of a ventricular septal defect.
Figure 2 .
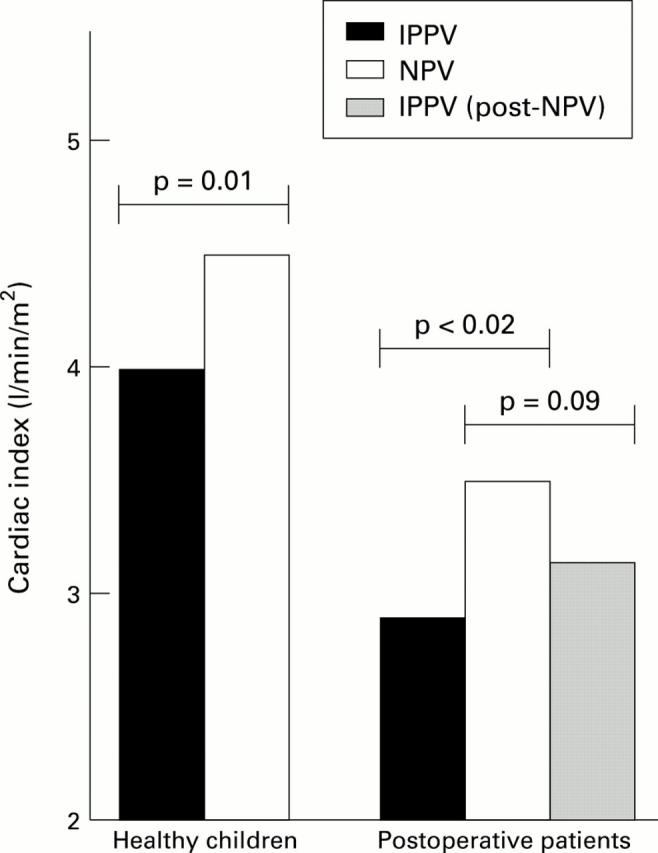
Cardiac index during intermittent positive pressure and negative pressure ventilation in the two patient groups.
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Cassidy S. S., Robertson C. H., Jr, Pierce A. K., Johnson R. L., Jr Cardiovascular effects of positive end-expiratory pressure in dogs. J Appl Physiol Respir Environ Exerc Physiol. 1978 May;44(5):743–750. doi: 10.1152/jappl.1978.44.5.743. [DOI] [PubMed] [Google Scholar]
- Cullen S., Shore D., Redington A. Characterization of right ventricular diastolic performance after complete repair of tetralogy of Fallot. Restrictive physiology predicts slow postoperative recovery. Circulation. 1995 Mar 15;91(6):1782–1789. doi: 10.1161/01.cir.91.6.1782. [DOI] [PubMed] [Google Scholar]
- Davies N. J., Denison D. M. The measurement of metabolic gas exchange and minute volume by mass spectrometry alone. Respir Physiol. 1979 Feb;36(2):261–267. doi: 10.1016/0034-5687(79)90029-x. [DOI] [PubMed] [Google Scholar]
- Dorinsky P. M., Whitcomb M. E. The effect of PEEP on cardiac output. Chest. 1983 Aug;84(2):210–216. doi: 10.1378/chest.84.2.210. [DOI] [PubMed] [Google Scholar]
- Easa D., Mundie T. G., Finn K. C., Hashiro G., Balaraman V. Continuous negative extrathoracic pressure versus positive end-expiratory pressure in piglets after saline lung lavage. Pediatr Pulmonol. 1994 Mar;17(3):161–168. doi: 10.1002/ppul.1950170305. [DOI] [PubMed] [Google Scholar]
- Gothard J. W., Busst C. M., Branthwaite M. A., Davies N. J., Denison D. M. Applications of respiratory mass spectrometry to intensive care. Anaesthesia. 1980 Sep;35(9):890–895. doi: 10.1111/j.1365-2044.1980.tb03950.x. [DOI] [PubMed] [Google Scholar]
- Henning R. J. Effects of positive end-expiratory pressure on the right ventricle. J Appl Physiol (1985) 1986 Sep;61(3):819–826. doi: 10.1152/jappl.1986.61.3.819. [DOI] [PubMed] [Google Scholar]
- Jardin F., Farcot J. C., Boisante L., Curien N., Margairaz A., Bourdarias J. P. Influence of positive end-expiratory pressure on left ventricular performance. N Engl J Med. 1981 Feb 12;304(7):387–392. doi: 10.1056/NEJM198102123040703. [DOI] [PubMed] [Google Scholar]
- Krumpe P. E., Zidulka A., Urbanetti J., Anthonisen N. R. Comparison of the effects of continuous negative external chest pressure and positive end-expiratory pressure on cardiac index in dogs. Am Rev Respir Dis. 1977 Jan;115(1):39–45. doi: 10.1164/arrd.1977.115.1.39. [DOI] [PubMed] [Google Scholar]
- Lloyd T. C., Jr Mechanical cardiopulmonary interdependence. J Appl Physiol Respir Environ Exerc Physiol. 1982 Feb;52(2):333–339. doi: 10.1152/jappl.1982.52.2.333. [DOI] [PubMed] [Google Scholar]
- Lockhat D., Langleben D., Zidulka A. Hemodynamic differences between continual positive and two types of negative pressure ventilation. Am Rev Respir Dis. 1992 Sep;146(3):677–680. doi: 10.1164/ajrccm/146.3.677. [DOI] [PubMed] [Google Scholar]
- Penny D. J., Redington A. N. Doppler echocardiographic evaluation of pulmonary blood flow after the Fontan operation: the role of the lungs. Br Heart J. 1991 Nov;66(5):372–374. doi: 10.1136/hrt.66.5.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pick R. A., Handler J. B., Murata G. H., Friedman A. S. The cardiovascular effect of positive end-expiratory pressure. Chest. 1982 Sep;82(3):345–350. doi: 10.1378/chest.82.3.345. [DOI] [PubMed] [Google Scholar]
- Pinsky M. R., Desmet J. M., Vincent J. L. Effect of positive end-expiratory pressure on right ventricular function in humans. Am Rev Respir Dis. 1992 Sep;146(3):681–687. doi: 10.1164/ajrccm/146.3.681. [DOI] [PubMed] [Google Scholar]
- Pinsky M. R. Determinants of pulmonary arterial flow variation during respiration. J Appl Physiol Respir Environ Exerc Physiol. 1984 May;56(5):1237–1245. doi: 10.1152/jappl.1984.56.5.1237. [DOI] [PubMed] [Google Scholar]
- Pinsky M. R. Heart-lung interactions during positive-pressure ventilation. New Horiz. 1994 Nov;2(4):443–456. [PubMed] [Google Scholar]
- Raine J., Redington A. N., Benatar A., Samuels M. P., Southall D. P. Continuous negative extrathoracic pressure and cardiac output--a pilot study. Eur J Pediatr. 1993 Jul;152(7):595–598. doi: 10.1007/BF01954088. [DOI] [PubMed] [Google Scholar]
- Rankin J. S., Olsen C. O., Arentzen C. E., Tyson G. S., Maier G., Smith P. K., Hammon J. W., Jr, Davis J. W., McHale P. A., Anderson R. W. The effects of airway pressure on cardiac function in intact dogs and man. Circulation. 1982 Jul;66(1):108–120. doi: 10.1161/01.cir.66.1.108. [DOI] [PubMed] [Google Scholar]
- Redmond J. M., Gillinov A. M., Stuart R. S., Zehr K. J., Winkelstein J. A., Herskowitz A., Cameron D. E., Baumgartner W. A. Heparin-coated bypass circuits reduce pulmonary injury. Ann Thorac Surg. 1993 Sep;56(3):474–479. doi: 10.1016/0003-4975(93)90882-i. [DOI] [PubMed] [Google Scholar]
- Skaburskis M., Helal R., Zidulka A. Hemodynamic effects of external continuous negative pressure ventilation compared with those of continuous positive pressure ventilation in dogs with acute lung injury. Am Rev Respir Dis. 1987 Oct;136(4):886–891. doi: 10.1164/ajrccm/136.4.886. [DOI] [PubMed] [Google Scholar]
- Skaburskis M., Rivero A., Fitchett D., Zidulka A. Hemodynamic effects of continuous negative chest pressure ventilation in heart failure. Am Rev Respir Dis. 1990 Apr;141(4 Pt 1):938–943. doi: 10.1164/ajrccm/141.4_Pt_1.938. [DOI] [PubMed] [Google Scholar]
- WHITTENBERGER J. L., McGREGOR M., BERGLUND E., BORST H. G. Influence of state of inflation of the lung on pulmonary vascular resistance. J Appl Physiol. 1960 Sep;15:878–882. doi: 10.1152/jappl.1960.15.5.878. [DOI] [PubMed] [Google Scholar]
- Westaby S. Organ dysfunction after cardiopulmonary bypass. A systemic inflammatory reaction initiated by the extracorporeal circuit. Intensive Care Med. 1987;13(2):89–95. doi: 10.1007/BF00254791. [DOI] [PubMed] [Google Scholar]



