Abstract
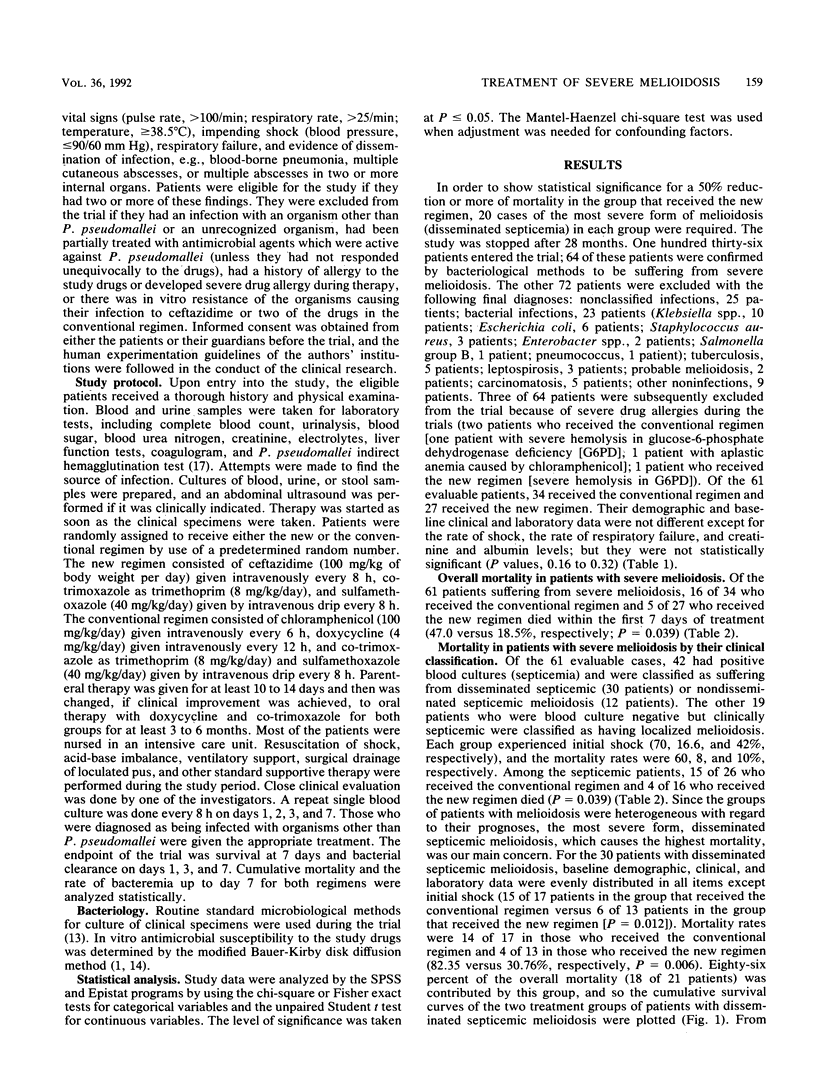
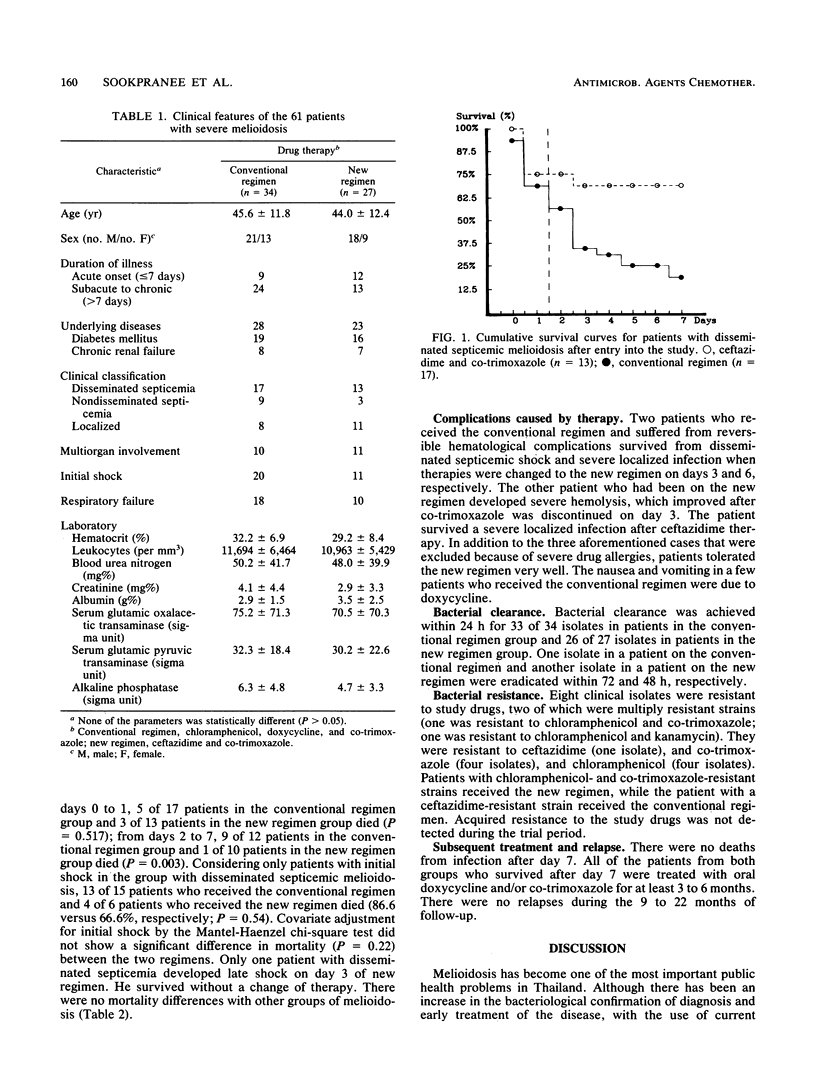
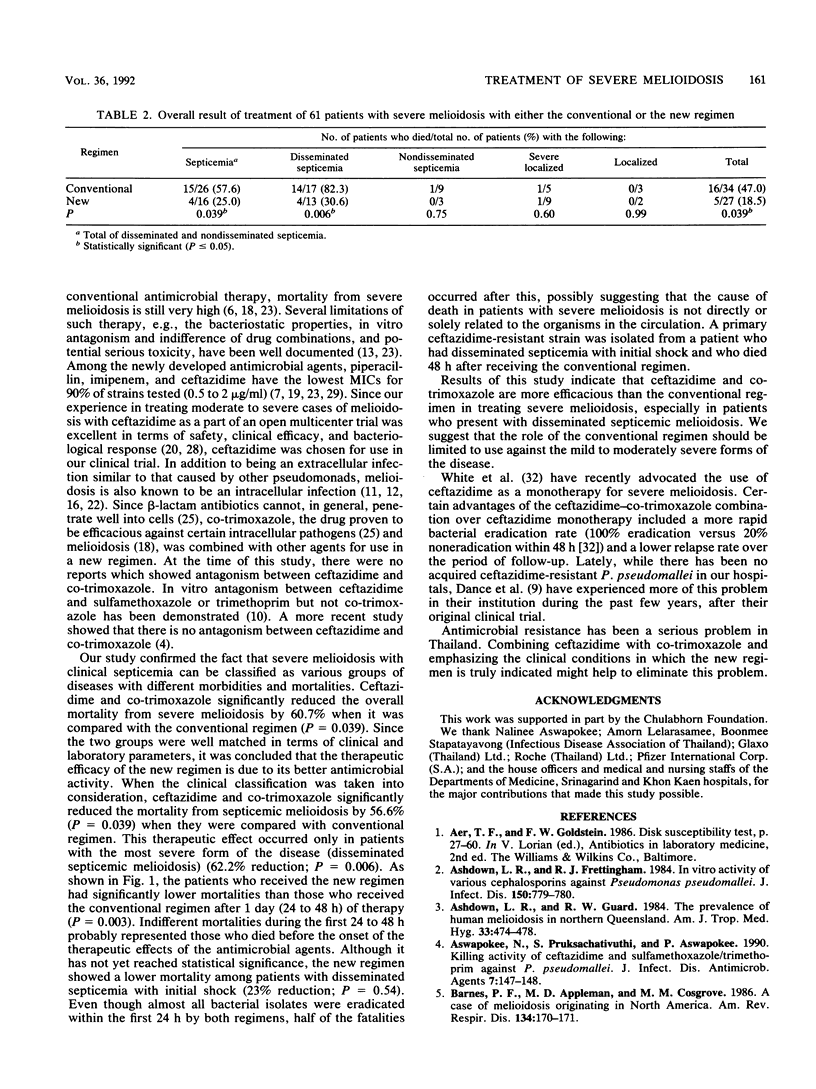
A prospective randomized trial was conducted at Srinagarind and Khon Kaen hospitals. Ceftazidime (100 mg/kg of body weight per day) and co-trimoxazole (trimethoprim, 8 mg/kg/day; sulfamethoxazole, 40 mg/kg/day) therapy was compared with conventional therapy (chloramphenicol, 100 mg/kg/day; doxycycline, 4 mg/kg/day; trimethoprim, 8 mg/kg/day; sulfamethoxazole, 40 mg/kg/day) in the treatment of 64 patients with bacteriologically confirmed cases of severe melioidosis who were admitted during September 1986 to January 1989. Of 61 evaluable patients (3 were excluded because of severe drug allergies), 42 were septicemic, and 31 of these patients had the most severe form, disseminated septicemic melioidosis. Their cumulative mortalities on day 7 were compared. There were significantly lower overall mortalities from melioidosis, septicemic melioidosis, and disseminated septicemic melioidosis in the group receiving the new treatment compared with those in the group receiving the conventional treatment (47 versus 18.5% [P = 0.039], 57.7 versus 25% [P = 0.039], and 82.3 versus 30.7% [P = 0.006], respectively); but the differences could have been influenced by the greater severity of illness, e.g., shock at initial presentation, in the patients who received the conventional treatment. Among patients with disseminated septicemia and initial shock, there was no significant difference in mortality between the regimens. Both regimens effectively eradicated bacteria from the circulation within 24 h (97 versus 96%, respectively). We recommend ceftazidime and co-trimoxazole as the drugs of choice for treatment of severe melioidosis, especially in those patients with disseminated septicemia.
Full text
PDF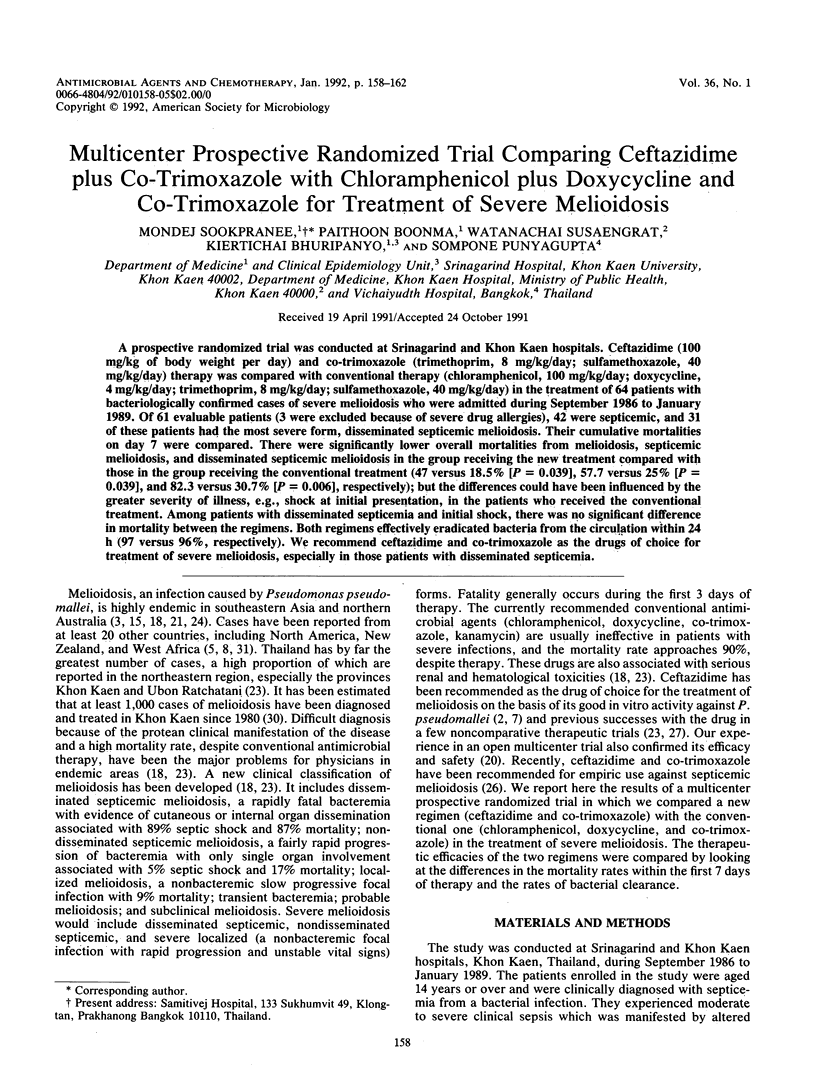
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashdown L. R., Frettingham R. J. In vitro activity of various cephalosporins against Pseudomonas pseudomallei. J Infect Dis. 1984 Nov;150(5):779–780. doi: 10.1093/infdis/150.5.779. [DOI] [PubMed] [Google Scholar]
- Ashdown L. R., Guard R. W. The prevalence of human melioidosis in Northern Queensland. Am J Trop Med Hyg. 1984 May;33(3):474–478. doi: 10.4269/ajtmh.1984.33.474. [DOI] [PubMed] [Google Scholar]
- Barnes P. F., Appleman M. D., Cosgrove M. M. A case of melioidosis originating in North America. Am Rev Respir Dis. 1986 Jul;134(1):170–171. doi: 10.1164/arrd.1986.134.1.170. [DOI] [PubMed] [Google Scholar]
- Chaowagul W., White N. J., Dance D. A., Wattanagoon Y., Naigowit P., Davis T. M., Looareesuwan S., Pitakwatchara N. Melioidosis: a major cause of community-acquired septicemia in northeastern Thailand. J Infect Dis. 1989 May;159(5):890–899. doi: 10.1093/infdis/159.5.890. [DOI] [PubMed] [Google Scholar]
- Chau P. Y., Ng W. S., Leung Y. K., Lolekha S. In vitro susceptibility of strains of Pseudomonas pseudomallei isolated in Thailand and Hong Kong to some newer beta-lactam antibiotics and quinolone derivatives. J Infect Dis. 1986 Jan;153(1):167–170. doi: 10.1093/infdis/153.1.167. [DOI] [PubMed] [Google Scholar]
- Corkill M. M., Cornere B. Melioidosis: a new disease to New Zealand. N Z Med J. 1987 Feb 25;100(818):106–107. [PubMed] [Google Scholar]
- DANNENBERG A. M., Jr, SCOTT E. M. Melioidosis: pathogenesis and immunity in mice and hamsters. I. Studies with virulent strains of Malleomyces pseudomallei. J Exp Med. 1958 Jan 1;107(1):153–166. doi: 10.1084/jem.107.1.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DANNENBERG A. M., Jr, SCOTT E. M. Melioidosis: pathogenesis and immunity in mice and hamsters. II. Studies with avirulent strains of Malleomyces pseudomallei. Am J Pathol. 1958 Nov-Dec;34(6):1099–1121. [PMC free article] [PubMed] [Google Scholar]
- Dance D. A., Wuthiekanun V., Chaowagul W., White N. J. Interactions in vitro between agents used to treat melioidosis. J Antimicrob Chemother. 1989 Sep;24(3):311–316. doi: 10.1093/jac/24.3.311. [DOI] [PubMed] [Google Scholar]
- Eickhoff T. C., Bennett J. V., Hayes P. S., Feeley J. Pseudomonas pseudomallei: susceptibility to chemotherapeutic agents. J Infect Dis. 1970 Feb;121(2):95–102. doi: 10.1093/infdis/121.2.95. [DOI] [PubMed] [Google Scholar]
- Guard R. W., Khafagi F. A., Brigden M. C., Ashdown L. R. Melioidosis in Far North Queensland. A clinical and epidemiological review of twenty cases. Am J Trop Med Hyg. 1984 May;33(3):467–473. doi: 10.4269/ajtmh.1984.33.467. [DOI] [PubMed] [Google Scholar]
- Kanai K., Dejsirilert S. Pseudomonas pseudomallei and melioidosis, with special reference to the status in Thailand. Jpn J Med Sci Biol. 1988 Aug;41(4):123–157. doi: 10.7883/yoken1952.41.123. [DOI] [PubMed] [Google Scholar]
- Khupulsup K., Petchclai B. Application of indirect hemagglutination test and indirect fluorescent antibody test for IgM antibody for diagnosis of melioidosis in Thailand. Am J Trop Med Hyg. 1986 Mar;35(2):366–369. doi: 10.4269/ajtmh.1986.35.366. [DOI] [PubMed] [Google Scholar]
- Leelarasamee A., Bovornkitti S. Melioidosis: review and update. Rev Infect Dis. 1989 May-Jun;11(3):413–425. doi: 10.1093/clinids/11.3.413. [DOI] [PubMed] [Google Scholar]
- PREVATT A. L., HUNT J. S. Chronic systemic melioidosis; review of literature and report of a case, with a note on visual disturbance due to chloramphenicol. Am J Med. 1957 Nov;23(5):810–823. doi: 10.1016/0002-9343(57)90382-0. [DOI] [PubMed] [Google Scholar]
- Pruksachartvuthi S., Aswapokee N., Thankerngpol K. Survival of Pseudomonas pseudomallei in human phagocytes. J Med Microbiol. 1990 Feb;31(2):109–114. doi: 10.1099/00222615-31-2-109. [DOI] [PubMed] [Google Scholar]
- RUBIN H. L., ALEXANDER A. D., YAGER R. H. Melioidosis--a military medical problem? Mil Med. 1963 Jun;128:538–542. [PubMed] [Google Scholar]
- Schwab J. C., Mandell G. L. The importance of penetration of antimicrobial agents into cells. Infect Dis Clin North Am. 1989 Sep;3(3):461–467. [PubMed] [Google Scholar]
- So S. Y., Chau P. Y., Leung Y. K., Lam W. K., Yu D. Y. Successful treatment of melioidosis caused by a multiresistant strain in an immunocompromised host with third generation cephalosporins. Am Rev Respir Dis. 1983 May;127(5):650–654. doi: 10.1164/arrd.1983.127.5.650. [DOI] [PubMed] [Google Scholar]
- Sookpranee T., Sookpranee M., Mellencamp M. A., Preheim L. C. Pseudomonas pseudomallei, a common pathogen in Thailand that is resistant to the bactericidal effects of many antibiotics. Antimicrob Agents Chemother. 1991 Mar;35(3):484–489. doi: 10.1128/aac.35.3.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall R. A., Mabey D. C., Corrah P. T., Peters L. A case of melioidosis in West Africa. J Infect Dis. 1985 Aug;152(2):424–425. doi: 10.1093/infdis/152.2.424a. [DOI] [PubMed] [Google Scholar]
- White N. J., Dance D. A., Chaowagul W., Wattanagoon Y., Wuthiekanun V., Pitakwatchara N. Halving of mortality of severe melioidosis by ceftazidime. Lancet. 1989 Sep 23;2(8665):697–701. doi: 10.1016/s0140-6736(89)90768-x. [DOI] [PubMed] [Google Scholar]


