Abstract
Background
Previous studies have shown elevated rates of health-related harms among Aboriginal people who use injection drugs such as heroin. Methadone maintenance therapy is one of the most effective interventions to address the harms of heroin injection. We assessed the rate of methadone use in a cohort of opioid injection drug users in Vancouver and investigated whether methadone use was associated with Aboriginal ethnic background.
Methods
Using data collected as part of the Vancouver Injection Drug Users Study (May 1996–November 2005), we evaluated whether Aboriginal ethnic background was associated with methadone use using generalized estimating equations and Cox regression analysis. We compared methadone use among Aboriginal and non-Aboriginal injection drug users at the time of enrolment and during the follow-up period, and we evaluated the time to first methadone use among people not using methadone at enrolment.
Results
During the study period, 1603 injection drug users (435 Aboriginal, 1168 non-Aboriginal) were recruited. At enrolment, 54 (12.4%) Aboriginal participants used methadone compared with 247 (21.2%) non-Aboriginal participants (odds ratio [OR] 0.53, 95% confidence interval [CI] 0.38–0.73, p < 0.001). Among the 1351 (84.3%) participants who used heroin, Aboriginal people were less likely to use methadone throughout the follow-up period (adjusted OR 0.60, 95% CI 0.45–0.81, p < 0.001). Among people using heroin but who were not taking methadone at enrolment, Aboriginal ethnic background was associated with increased time to first methadone use (adjusted relative hazard 0.60, 95% CI 0.49–0.74, p < 0.001).
Interpretation
Methadone use was lower among Aboriginal than among non-Aboriginal injection drug users. Culturally appropriate interventions with full participation of the affected community are required to address this disparity.
Illicit injection drug use is associated with a wide array of health and social harms.1–3 The provision of addiction treatment is one of the most effective interventions to address these harms. Several Cochrane reviews have concluded that methadone treatment is effective in treating addiction to heroin and other opioids.4–6
During the last decade, Vancouver has experienced a public health crisis related to the use of injection drugs.7 Previous studies have demonstrated that health and social harms related to this problem may be overrepresented among Aboriginal people.8–10 We conducted the present study to evaluate the rate of methadone use among a cohort of injection drug users in Vancouver and to examine whether Aboriginal ethnic background was associated with reduced methadone use.
Methods
Study participants
The Vancouver Injection Drug Users Study (VIDUS) included people who had injected illicit drugs (heroin, cocaine or methamphetamine) in the month before enrolment.11 At enrolment and semi-annually thereafter, participants provided a venous blood sample and responded to a questionnaire administered by an interviewer. This study received annual ethics approval from the University of British Columbia's Providence Health Care Research Ethics Board.
Statistical analysis
We used several approaches to examine whether Aboriginal ethnic background (defined as a person who self-reported as being Aboriginal, Metis, Inuit or First Nations8) was associated with methadone use. All multivariate models were fit by use of a protocol defined a priori to adjust for all variables that were significant (p < 0.05) in the univariate analyses. Behaviours refer to the participants' activities in the 6 months before each visit. Definitions of the variables used were identical to those used in earlier reports.8 First, we evaluated whether Aboriginal ethnic background was associated with methadone use at the time of enrolment. Second, we used generalized estimating equations to examine whether Aboriginal ethnic background was associated with methadone use during the study period (May 1996–November 2005) using data obtained at enrolment and at semi-annual follow-up visits. For this analysis, we considered the following additional variables as potential determinants of methadone use: age; sex; residence in Vancouver's Downtown Eastside; unstable residence; borrowing and lending syringes; injection of heroin, cocaine or speedball (mixture of heroin and cocaine); involvement in the sex trade; help required to inject; and binge drug use. Finally, in order to determine the factors associated with first time methadone use among people not using methadone at enrolment, we used Kaplan–Meier methods and Cox proportional hazards regression.
Results
Overall, 1603 people were recruited into the Vancouver Injection Drug Users Study during the study period. Of these, 435 were Aboriginal: 189 (43%) First Nations, 188 (43%) Aboriginal, 57 (13%) Metis and 1 (< 1%) Inuit. At enrolment, 12.4% (54/435) of Aboriginal participants used methadone versus 21.2% (247/1168) of non-Aboriginal participants (odds ratio [OR] 0.53, 95% confidence interval [CI] 0.38–0.73, p < 0.001). Among all participants, 1351 (84.3%) reported ever using heroin alone or in combination with cocaine (speedball) during the follow-up period. We focused on this population because methadone is only available to those who have used opioids.
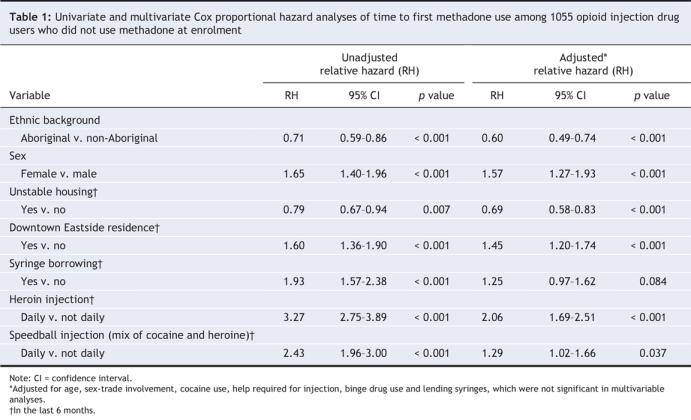
Regression analysis (by use of generalized estimating equations) showed that Aboriginal participants were less likely to use methadone compare with non-Aboriginal participants (univariate analysis, OR 0.51, 95% CI 0.41–0.63, p < 0.001; multivariate analysis, OR 0.60, 95% CI 0.45–0.81, p < 0.001). Figure 1 shows the time to first methadone use among the 1055 injection drug users who used opioids but did not use methadone at enrolment and who had at least 1 follow-up visit. Aboriginal ethnic background was associated with a lower rate of initiation of methadone therapy over the follow-up period compared with non-Aboriginal ethnic background (log-rank p < 0.001). Indeed, Aboriginal ethnic background was associated with a longer time to first methadone use in both the unadjusted (relative hazard [RH] 0.71, 95% CI 0.59–0.86, p < 0.001) and the multivariate adjusted (RH 0.60, 95% CI 0.49–0.74, p < 0.001) analyses (Table 1). Ab-original ethnic background remained independently associated with reduced methadone use even if we altered the model-fitting protocol and forced in additional sociodemographic variables, such as education and employment (full details of this analysis are available from the corresponding author).
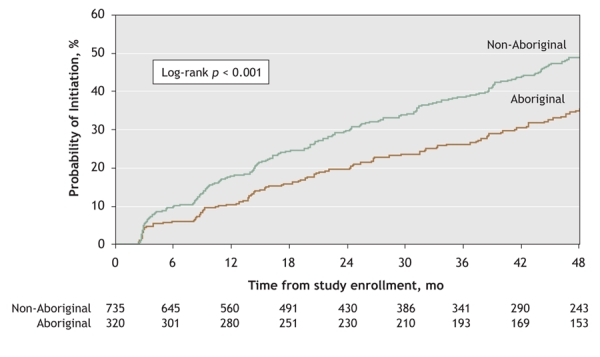
Figure 1: Cumulative rate of initiation of methadone treatment among 1055 opioid injection drug users who did not use methadone at enrolment, stratified by ethnic background.
Table 1
Interpretation
In the present study, we found that Aboriginal ethnic background was associated with reduced use of methadone at baseline. When we followed heroin users over time and examined the rate of methadone initiation, we found that Aboriginal participants had a slower time to initiation compared with non-Aboriginal participants.
In Canada, the problem of addiction deserves both great attention from policy makers and greater application of evidence-based public health strategies.2 Since a number of the health-related harms stemming from illicit drug use may be more common among Aboriginal people,8 this population will require dedicated resources and policy initiatives. However, these initiatives must be evidence-based2 and developed in full collaboration with the affected community. In addition, further study is required to understand why the rate of methadone use appears to be lower among this population.
Although the Vancouver Injection Drug Users Study is believed to be representative of injection drug users in Vancouver, this type of cohort study is limited by the fact that there are no registries of injection drug users from which to draw a random sample, and as such our findings may not be generalizable to other settings. In addition, certain behaviours, such as syringe sharing, may be underreported because they are socially undesirable. It is also possible that methadone use was under-or overreported.12 However, the end points used in our study (primarily methadone maintenance therapy and ethnic background) have not been shown to be affected by under-or overreporting or by issues of recall bias. In addition, we have used an inclusive definition for Aboriginal people based on how study participants self-identified upon recruitment to the study; however, it is likely that there are unique groups within this definition.
Previous studies have shown elevated rates of HIV infection and other health-related harms among Aboriginal people who use injection drugs.8–10 Our study indicates that, in addition to these concerns, there may be other considerable barriers to evidence-based treatment for heroin addiction and highlights issues related to HIV prevention and access to health care. Interventions that are evidence-based and culturally appropriate and that have the full participation of the affected community (designing, planning, implementation and evaluation) are required to address ongoing health-related harms and disparities in the access to addiction treatment among this population.
Acknowledgments
We thank the participants of the Vancouver Injection Drug Users Study for their ongoing contribution to the study, and the members of the Community Advisory Board for the Vancouver Injection Drug Users Study.
Footnotes
This article has been peer reviewed.
Contributors: Evan Wood designed the study and wrote the first draft of the manuscript. Kathy Li conducted the statistical analyses. All of the authors contributed to the conception and design of the study and to writing the article. All of the authors approved the final version for publication.
We also thank Caitlin Johnston, Deborah Graham, Steve Kain, Peter Vann, John Charette, Cody Callon, Sidney Crosby, Vanessa Volkommer, Sandra Wheller, Trevor Logan, Cristy Power, Daniel Kane, Calvin Lai and Will Small for their administrative assistance. The study was supported by the US National Institutes of Health and the Canadian Institutes of Health Research.
Competing interests: None declared for Evan Wood, Kathy Li, Lucy Barney, Mark Tyndall, and Thomas Kerr. Julio Montaner has received grants from, has served as an ad hoc advisor to, or has spoken at events sponsored by Abbott, Argos Therapeutics, Bioject, Boehringer Ingelheim, Bristol-Myers Squibb, Gilead Sciences, GlaxoSmithKline, Hoffmann-La Roche, Janssen-Ortho, Merck Frosst, Pfizer, Schering-Plough, Serono, TheraTechnologies, Tibotec and Trimeris.
Correspondence to: Dr. Evan Wood, British Columbia Centre for Excellence in HIV/AIDS, Rm. 608, 1081 Burrard St., Vancouver BC V6Z 1Y6; fax 604 806-9044; ewood@cfenet.ubc.ca
REFERENCES
- 1.Strathdee SA, Galai N, Safaeian M, et al. Sex differences in risk factors for HIV seroconversion among injection drug users: a 10-year perspective. Arch Intern Med 2001;161:1281-8. [DOI] [PubMed]
- 2.Wood E, Li K, Small W, et al. Recent incarceration independently associated with syringe sharing by injection drug users. Public Health Rep 2005;120:150-6. [DOI] [PMC free article] [PubMed]
- 3.Romero-Daza N, Weeks M, Singer M. “Nobody gives a damn if I live or die”: violence, drugs, and street-level prostitution in inner-city Hartford, Connecticut. Med Anthropol 2003;22:233-59. [DOI] [PubMed]
- 4.Faggiano F, Vigna-Taglianti F, Versino E, et al. Methadone maintenance at different dosages for opioid dependence. Cochrane Database Syst Rev 2003;3:CD002208. [DOI] [PubMed]
- 5.Mattick RP, Breen C, Kimber J, et al. Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence. Cochrane Database Syst Rev 2003;2:CD002209. [DOI] [PubMed]
- 6.Amato L, Minozzi S, Davoli M, et al. Psychosocial combined with agonist maintenance treatments versus agonist maintenance treatments alone for treatment of opioid dependence. Cochrane Database Syst Rev 2004;4:CD004147. [DOI] [PubMed]
- 7.Wood E, Tyndall MW, Montaner JS, et al. Summary of findings from the evaluation of a pilot medically supervised safer injecting facility. CMAJ 2006;175:1399-404. [DOI] [PMC free article] [PubMed]
- 8.Craib KJ, Spittal PM, Wood E, et al. Risk factors for elevated HIV incidence among Aboriginal injection drug users in Vancouver. CMAJ 2003;168:19-24. [PMC free article] [PubMed]
- 9.Wood E, Kerr T, Palepu A, et al. Slower uptake of HIV antiretroviral therapy among Aboriginal injection drug users. J Infect 2006;52:233-6. [DOI] [PubMed]
- 10.Benoit C, Carroll D, Chaudhry M. In search of a healing place: Aboriginal women in Vancouver's Downtown Eastside. Soc Sci Med 2003;56:821-33. [DOI] [PubMed]
- 11.Strathdee SA, Patrick DM, Currie SL, et al. Needle exchange is not enough: lessons from the Vancouver injecting drug use study. AIDS 1997;11:F59-65. [DOI] [PubMed]
- 12.Des Jarlais DC, Paone D, Milliken J, et al. Audio-computer interviewing to measure risk behaviour for HIV among injecting drug users: a quasi-randomised trial. Lancet 1999;353:1657-61. [DOI] [PubMed]
- 13.Wardman D, Clement K, Quantz D. Access and utilization of health services by British Columbia's rural Aboriginal population. Int J Health Care Qual Assur Inc Leadersh Health Serv 2005;18:xxvi-xxxi. [DOI] [PubMed]
- 14.Shah BR, Gunraj N, Hux JE. Markers of access to and quality of primary care for aboriginal people in Ontario, Canada. Am J Public Health 2003;93:798-802. [DOI] [PMC free article] [PubMed]
- 15.Reading J. The quest to improve Aboriginal health [editorial]. CMAJ 2006;174:1233. [DOI] [PMC free article] [PubMed]


