Abstract
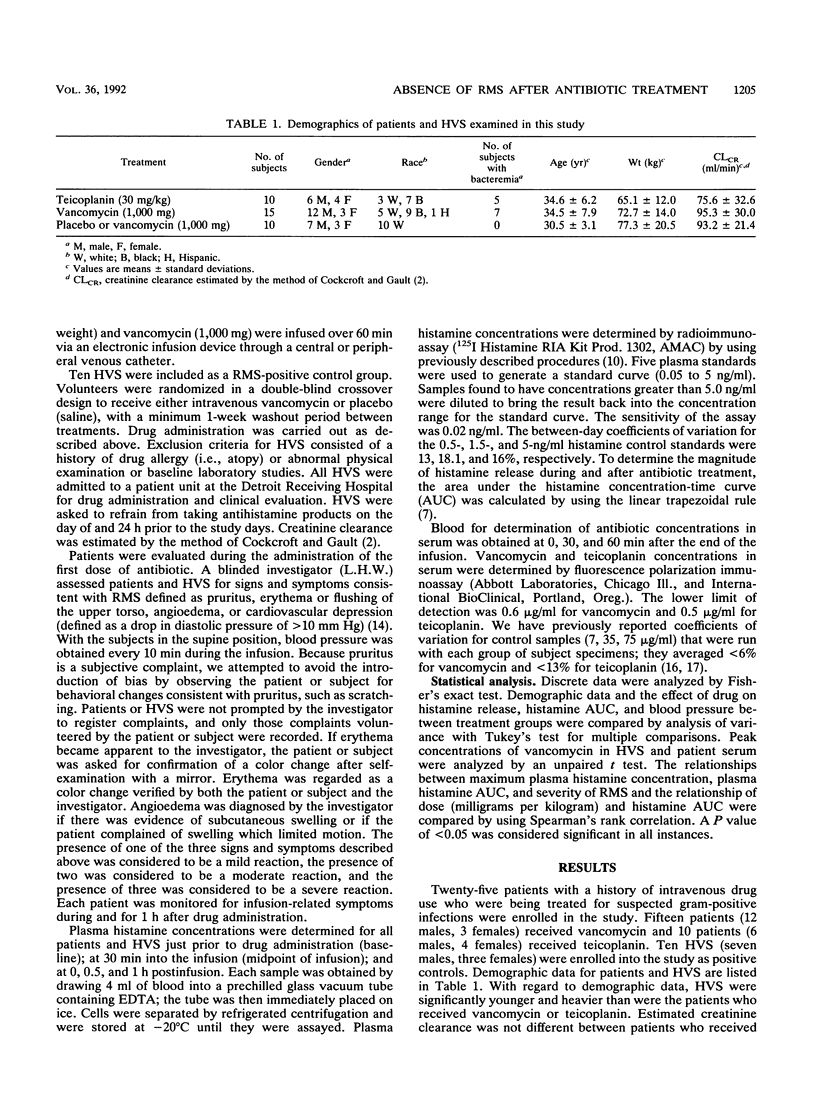
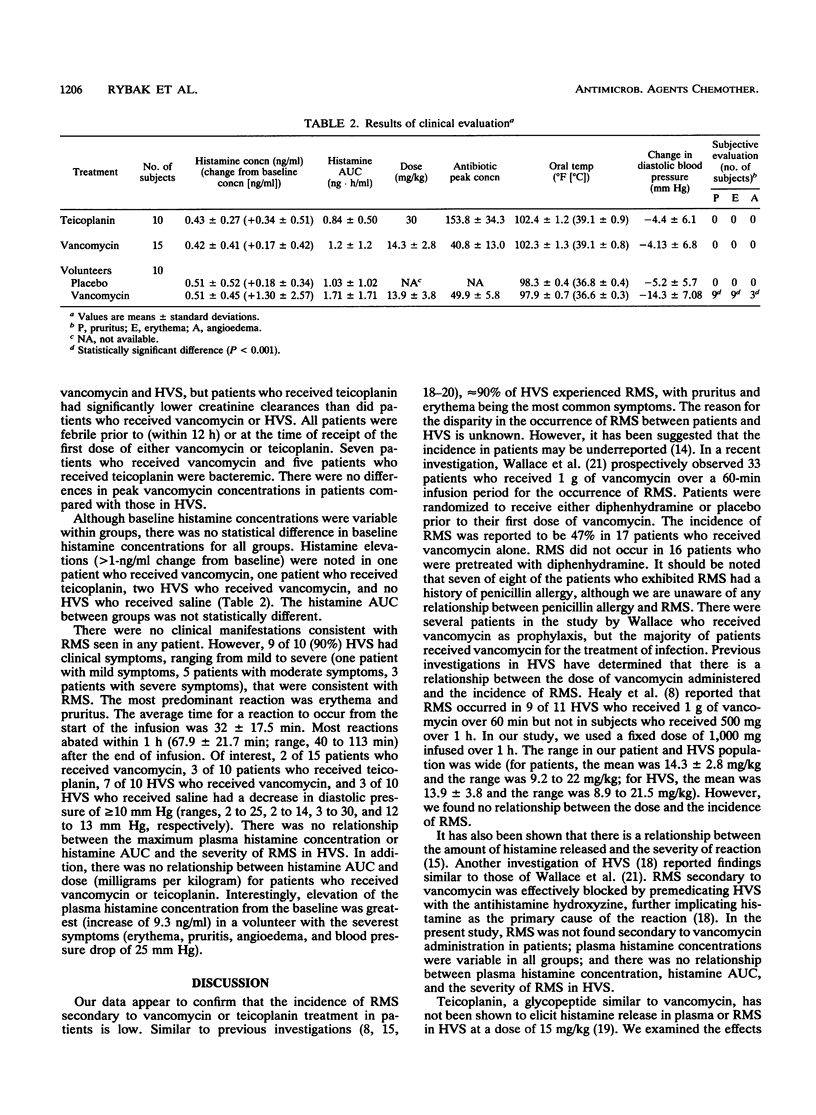
Twenty-five febrile patients with a history of intravenous drug use who were receiving either vancomycin (15 patients) or teicoplanin (10 patients) as part of a multicenter, double-blind, randomized, clinical efficacy trial were enrolled, upon receipt of their first dose of antibiotic, into a study to evaluate the effect of 1 g of vancomycin and high-dose teicoplanin (30 mg/kg of body weight) on histamine release and the occurrence of "red man syndrome" (RMS). In addition, 10 healthy volunteer subjects (HVS) were randomized to receive either 1 g of vancomycin intravenously or a saline infusion in a double-blind, crossover design study. Patients and HVS were observed for the presence of erythema, flushing, pruritus, and hypotension during and for up to 1 h postinfusion by a blinded investigator. Histamine concentrations in plasma were measured at baseline and during and after drug infusion. No significant differences were noted in baseline temperature between patients (vancomycin recipients, 102.3 degrees F [39.1 degrees C]; teicoplanin recipients, 102.4 degrees F [39.1 degrees C]) or incidence of bacteremia (7 of 15 vancomycin recipients; 5 of 10 teicoplanin recipients). There were no significant differences in peak vancomycin concentrations in the sera of patients (40.8 micrograms/ml) and HVS (49.9 micrograms/ml). There were no reactions consistent with RMS in any patient who received teicoplanin (0 of 10); there was a significant difference in the occurrence of RMS in patients in comparison with that in HVS (0 of 15 patients, 9 of 10 HVS; P less than 0.001) who received vancomycin. The predominant reaction was erythema and pruritus. Histamine concentrations in plasma and the area under the histamine plasma concentration-time curve were highly variable within groups and were not statistically different between patients and HVS. The incidence of RMS secondary to vancomycin or teicoplanin in our patient population appears to be low and consistent with clinical observations. Similar to previous investigations, RMS secondary to vancomycin in HVS was high (90%). However, we found no relationship between the histamine concentration in plasma or the area under the plasma histamine concentration-time curve and the severity of RMS in HVS. The reason for the discrepancy of RMS in patients versus that in HVS in unknown, but it may be related to a blunted effect of glycopeptides to produce the reaction in the presence of infection or it may be specific to our patient population.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bailie G. R., Yu R., Morton R., Waldek S. Vancomycin, red neck syndrome, and fits. Lancet. 1985 Aug 3;2(8449):279–280. doi: 10.1016/s0140-6736(85)90332-0. [DOI] [PubMed] [Google Scholar]
- Cockcroft D. W., Gault M. H. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16(1):31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- Cole D. R., Oliver M., Coward R. A., Brown C. B. Allergy, red man syndrome, and vancomycin. Lancet. 1985 Aug 3;2(8449):280–280. doi: 10.1016/s0140-6736(85)90333-2. [DOI] [PubMed] [Google Scholar]
- Davis R. L., Smith A. L., Koup J. R. The "red man's syndrome" and slow infusion of vancomycin. Ann Intern Med. 1986 Feb;104(2):285–286. doi: 10.7326/0003-4819-104-2-285_2. [DOI] [PubMed] [Google Scholar]
- Dubettier S., Boibieux A., Lagable M., Crevon L., Peyramond D., Milon H. Red man syndrome with teicoplanin. Rev Infect Dis. 1991 Jul-Aug;13(4):770–770. doi: 10.1093/clinids/13.4.770. [DOI] [PubMed] [Google Scholar]
- Garrelts J. C., Peterie J. D. Vancomycin and the "red man's syndrome". N Engl J Med. 1985 Jan 24;312(4):245–245. [PubMed] [Google Scholar]
- Healy D. P., Sahai J. V., Fuller S. H., Polk R. E. Vancomycin-induced histamine release and "red man syndrome": comparison of 1- and 2-hour infusions. Antimicrob Agents Chemother. 1990 Apr;34(4):550–554. doi: 10.1128/aac.34.4.550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McBride P., Bradley D., Kaliner M. Evaluation of a radioimmunoassay for histamine measurement in biologic fluids. J Allergy Clin Immunol. 1988 Oct;82(4):638–646. doi: 10.1016/0091-6749(88)90977-3. [DOI] [PubMed] [Google Scholar]
- Moss J., Rosow C. E. Histamine release by narcotics and muscle relaxants in humans. Anesthesiology. 1983 Oct;59(4):330–339. doi: 10.1097/00000542-198310000-00011. [DOI] [PubMed] [Google Scholar]
- Newfield P., Roizen M. F. Hazards of rapid administration of vancomycin. Ann Intern Med. 1979 Oct;91(4):581–581. doi: 10.7326/0003-4819-91-4-581. [DOI] [PubMed] [Google Scholar]
- Pau A. K., Khakoo R. "Red-neck syndrome" with slow infusion of vancomycin. N Engl J Med. 1985 Sep 19;313(12):756–757. doi: 10.1056/NEJM198509193131214. [DOI] [PubMed] [Google Scholar]
- Polk R. E. Anaphylactoid reactions to glycopeptide antibiotics. J Antimicrob Chemother. 1991 Apr;27 (Suppl B):17–29. doi: 10.1093/jac/27.suppl_b.17. [DOI] [PubMed] [Google Scholar]
- Polk R. E., Healy D. P., Schwartz L. B., Rock D. T., Garson M. L., Roller K. Vancomycin and the red-man syndrome: pharmacodynamics of histamine release. J Infect Dis. 1988 Mar;157(3):502–507. doi: 10.1093/infdis/157.3.502. [DOI] [PubMed] [Google Scholar]
- Rybak M. J., Albrecht L. M., Berman J. R., Warbasse L. H., Svensson C. K. Vancomycin pharmacokinetics in burn patients and intravenous drug abusers. Antimicrob Agents Chemother. 1990 May;34(5):792–795. doi: 10.1128/aac.34.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rybak M. J., Bailey E. M., Reddy V. N. Clinical evaluation of teicoplanin fluorescence polarization immunoassay. Antimicrob Agents Chemother. 1991 Aug;35(8):1586–1590. doi: 10.1128/aac.35.8.1586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sahai J. V., Polk R. E., Schwartz L. B., Healy D. P., Westin E. H. Severe reaction to vancomycin not mediated by histamine release and documented by rechallenge. J Infect Dis. 1988 Dec;158(6):1413–1414. doi: 10.1093/infdis/158.6.1413. [DOI] [PubMed] [Google Scholar]
- Sahai J., Healy D. P., Garris R., Berry A., Polk R. E. Influence of antihistamine pretreatment on vancomycin-induced red-man syndrome. J Infect Dis. 1989 Nov;160(5):876–881. doi: 10.1093/infdis/160.5.876. [DOI] [PubMed] [Google Scholar]
- Sahai J., Healy D. P., Shelton M. J., Miller J. S., Ruberg S. J., Polk R. Comparison of vancomycin- and teicoplanin-induced histamine release and "red man syndrome". Antimicrob Agents Chemother. 1990 May;34(5):765–769. doi: 10.1128/aac.34.5.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallace M. R., Mascola J. R., Oldfield E. C., 3rd Red man syndrome: incidence, etiology, and prophylaxis. J Infect Dis. 1991 Dec;164(6):1180–1185. doi: 10.1093/infdis/164.6.1180. [DOI] [PubMed] [Google Scholar]


