Abstract
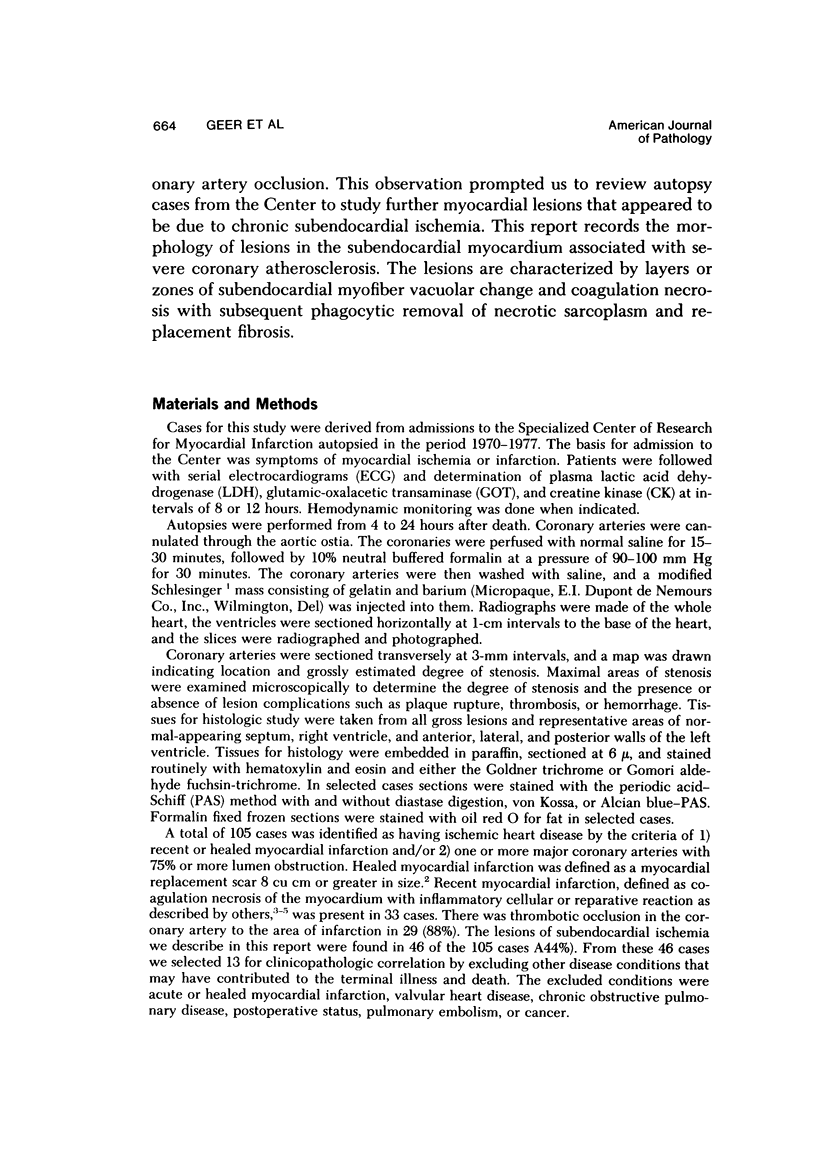
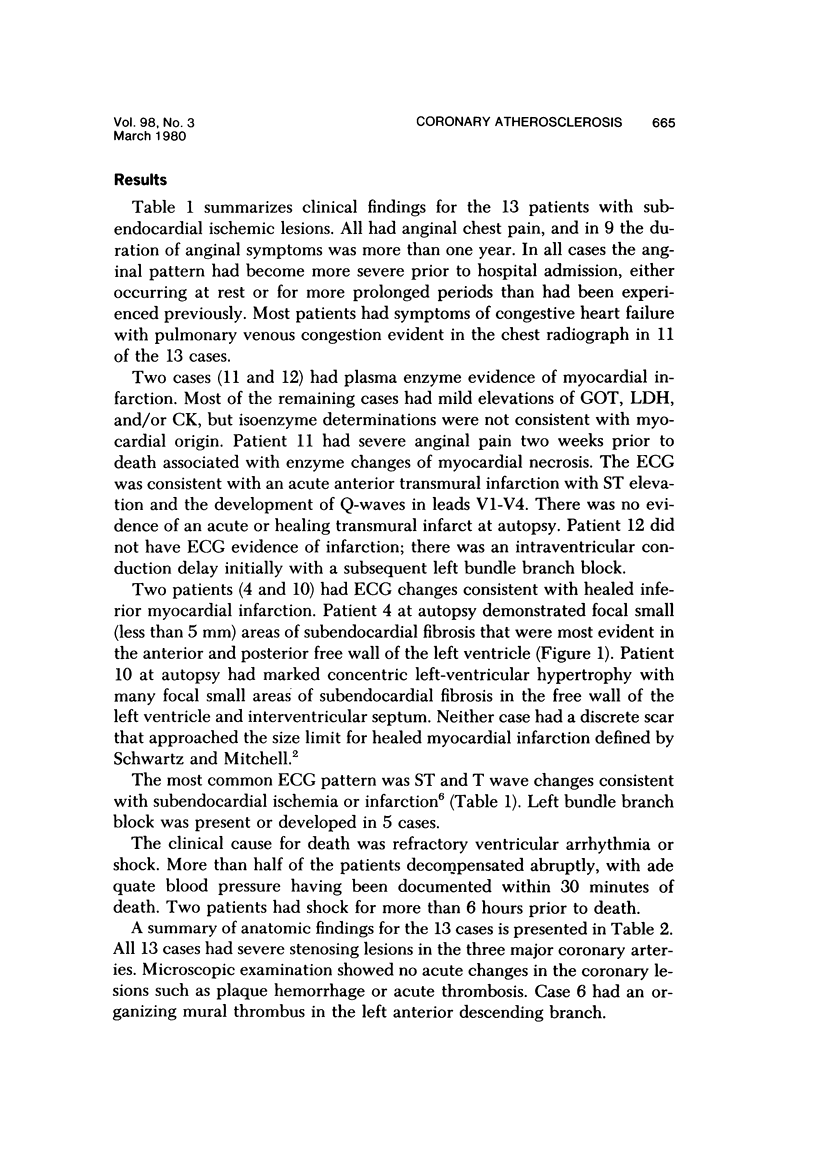
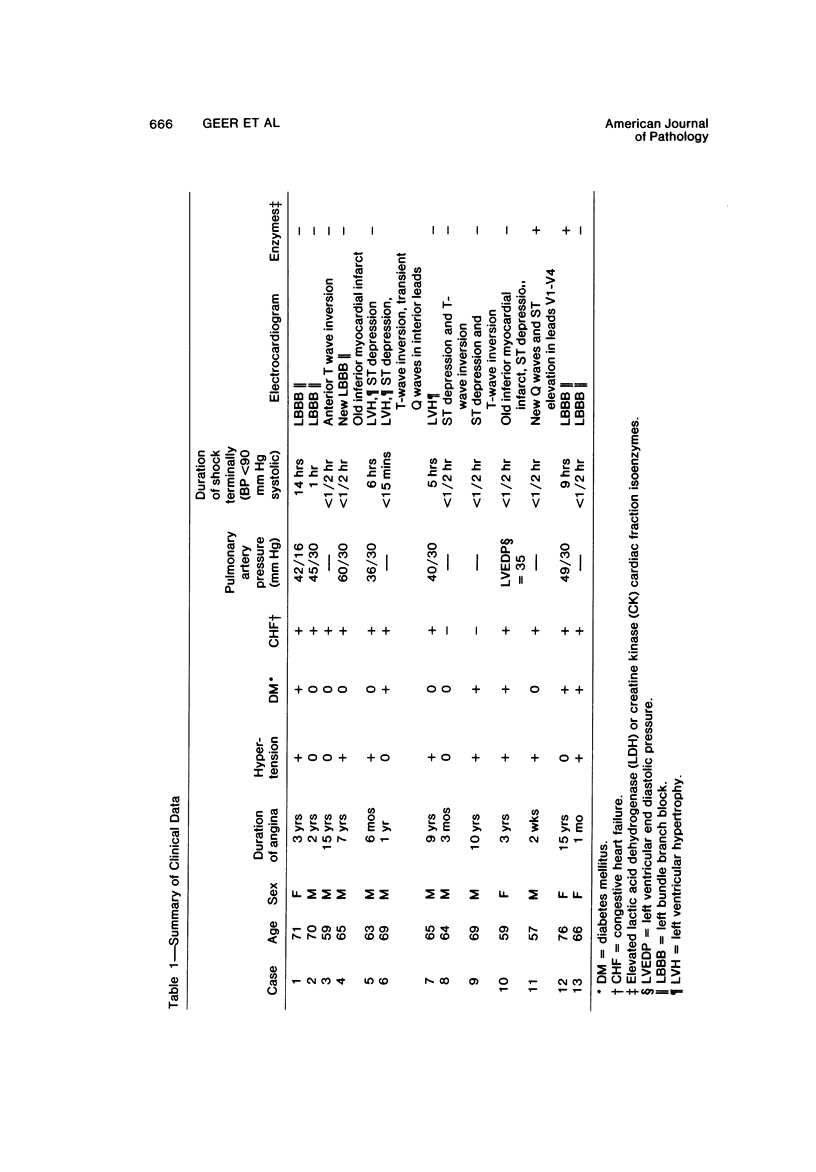
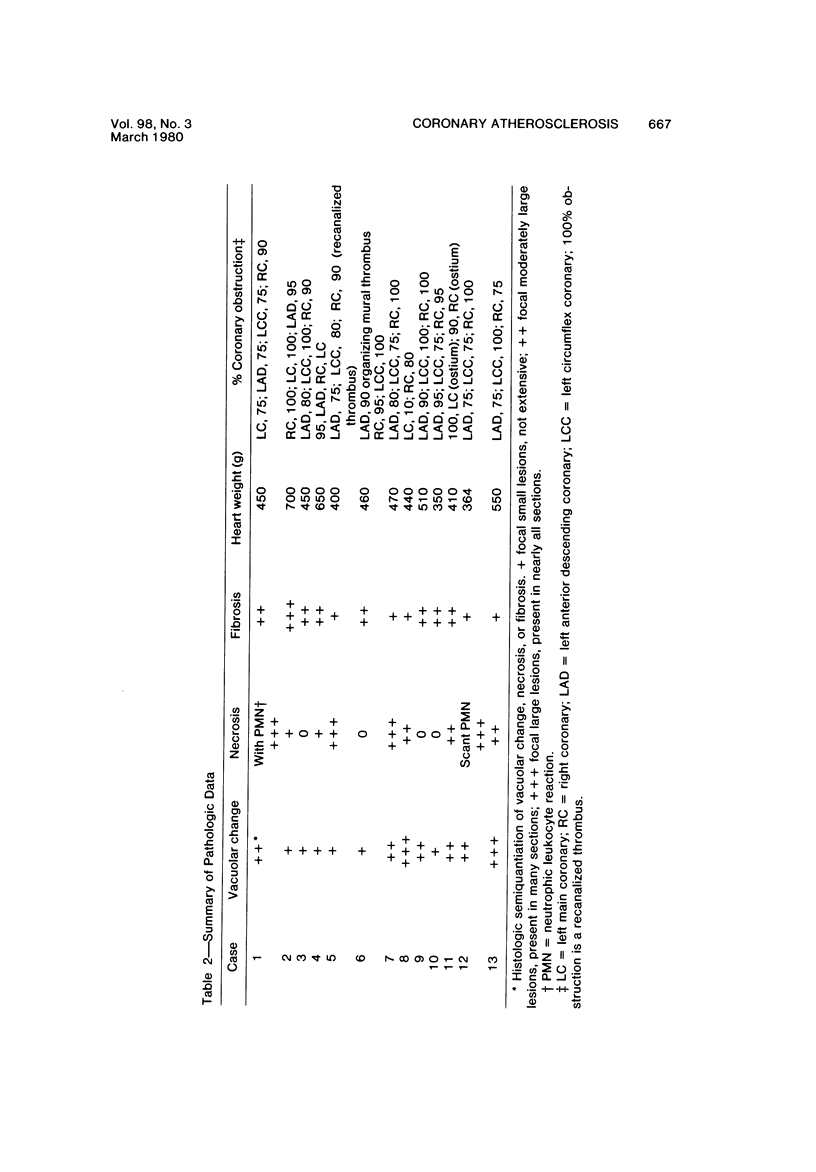
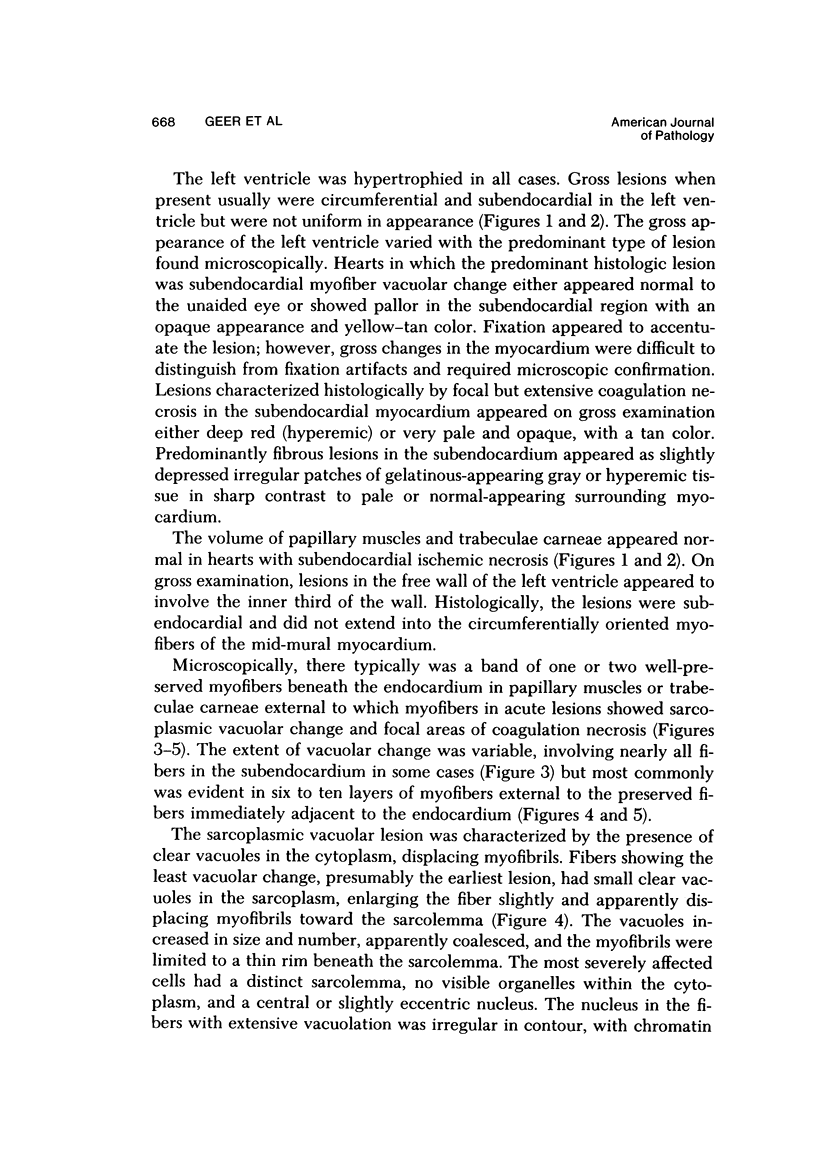
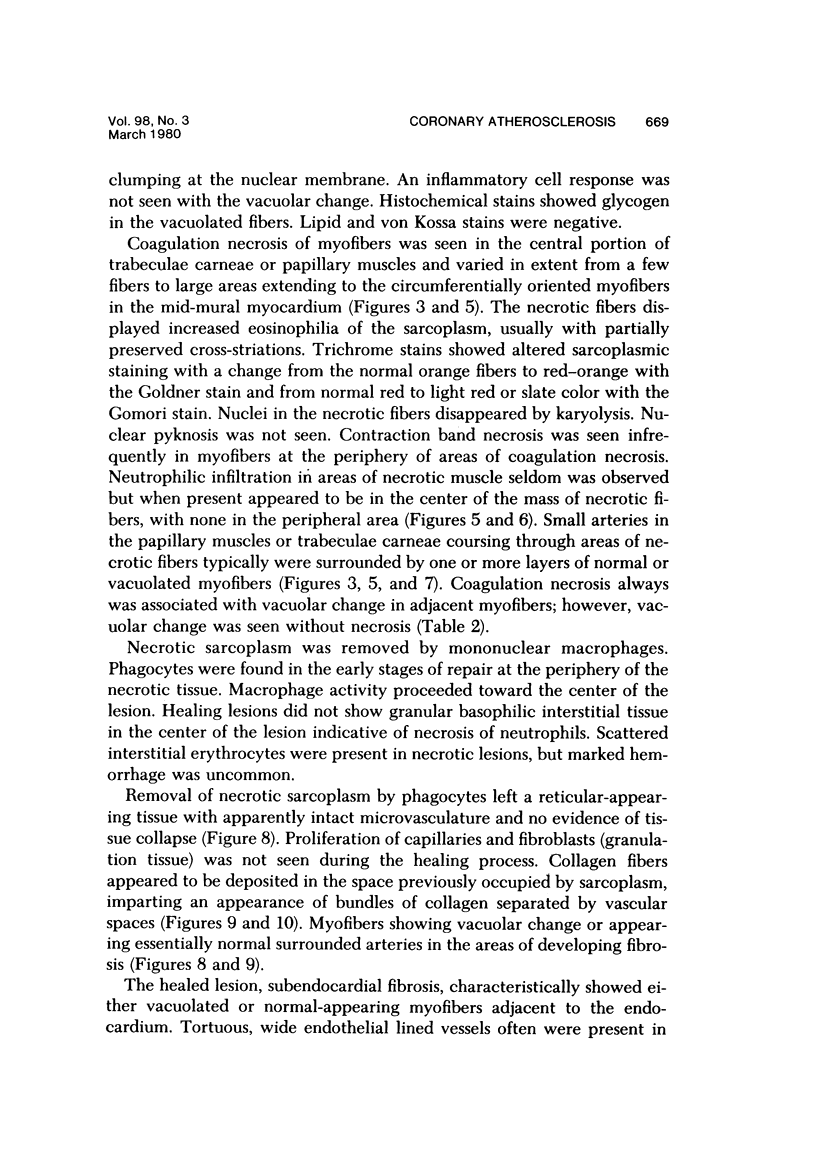
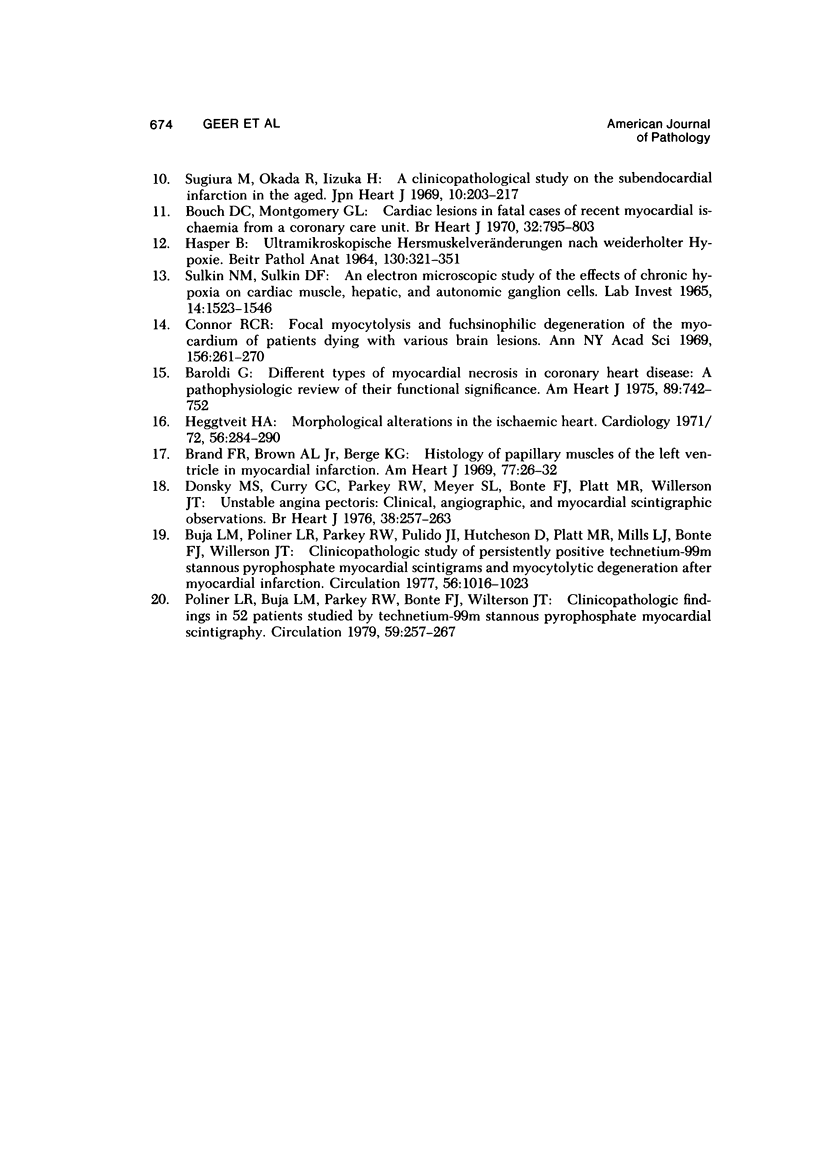
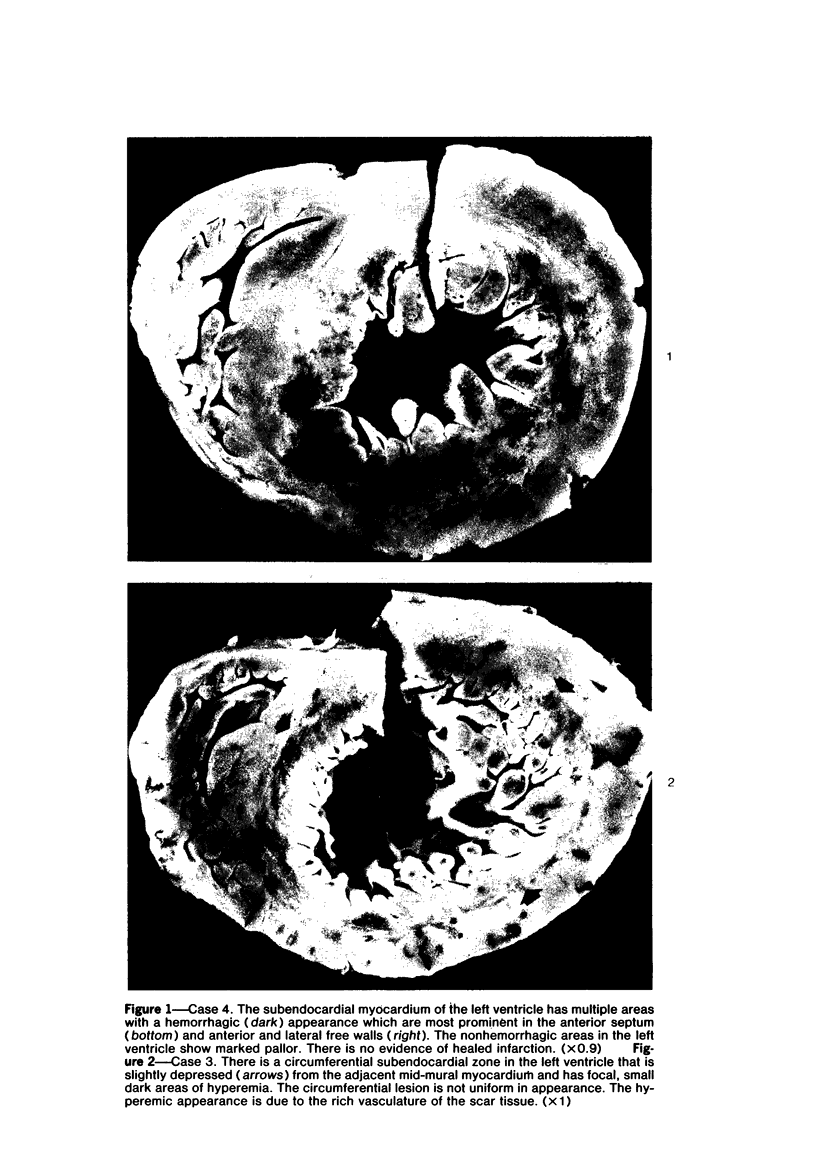
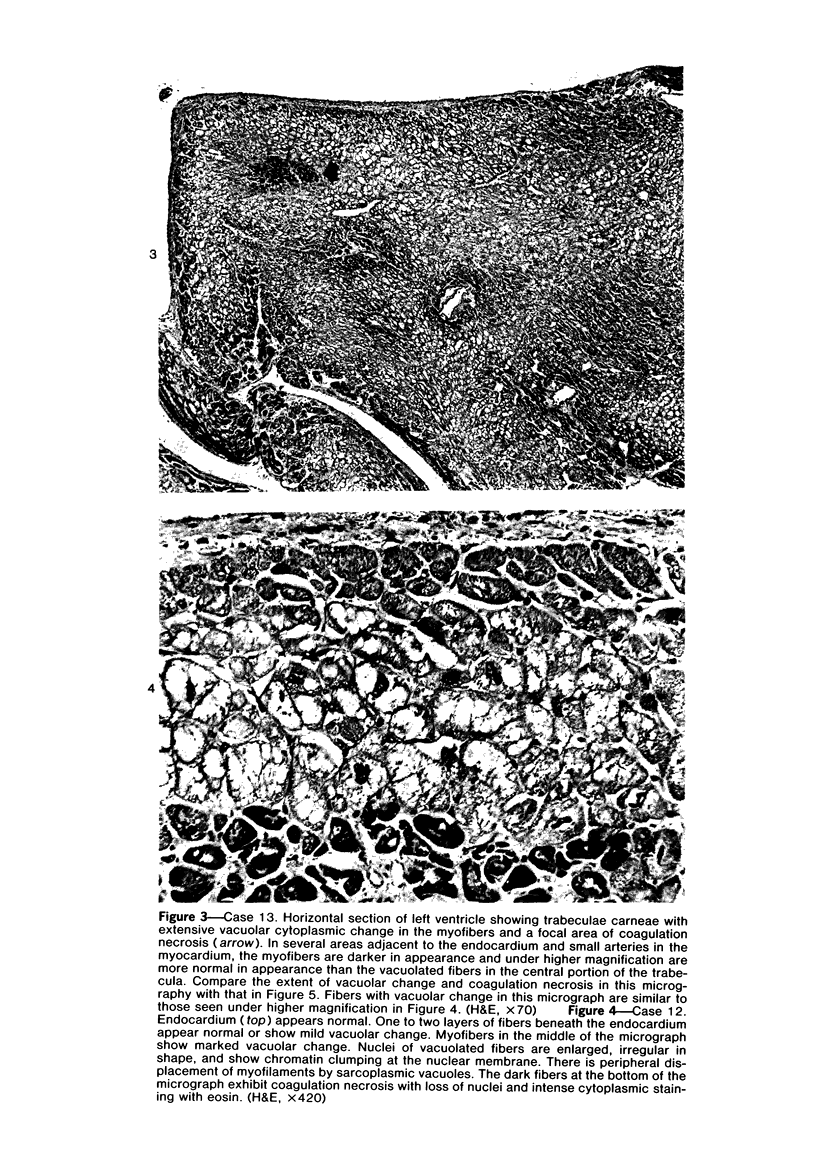
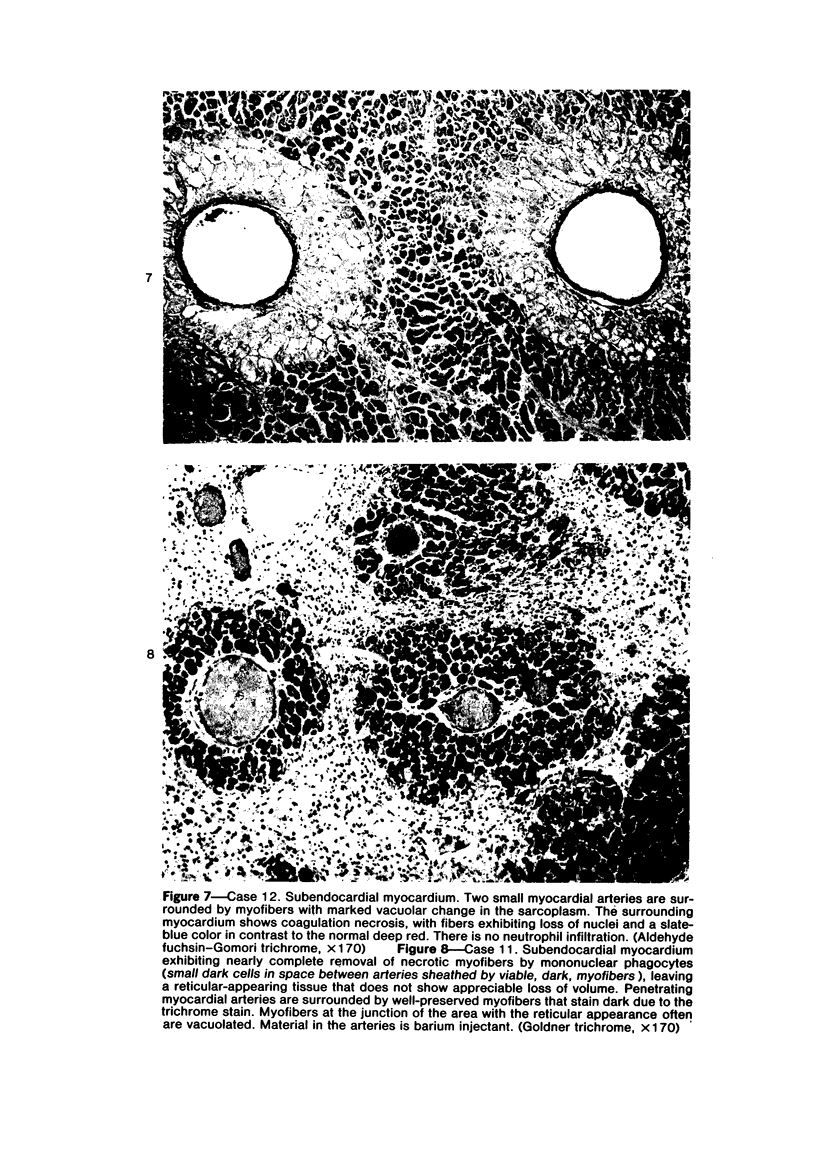
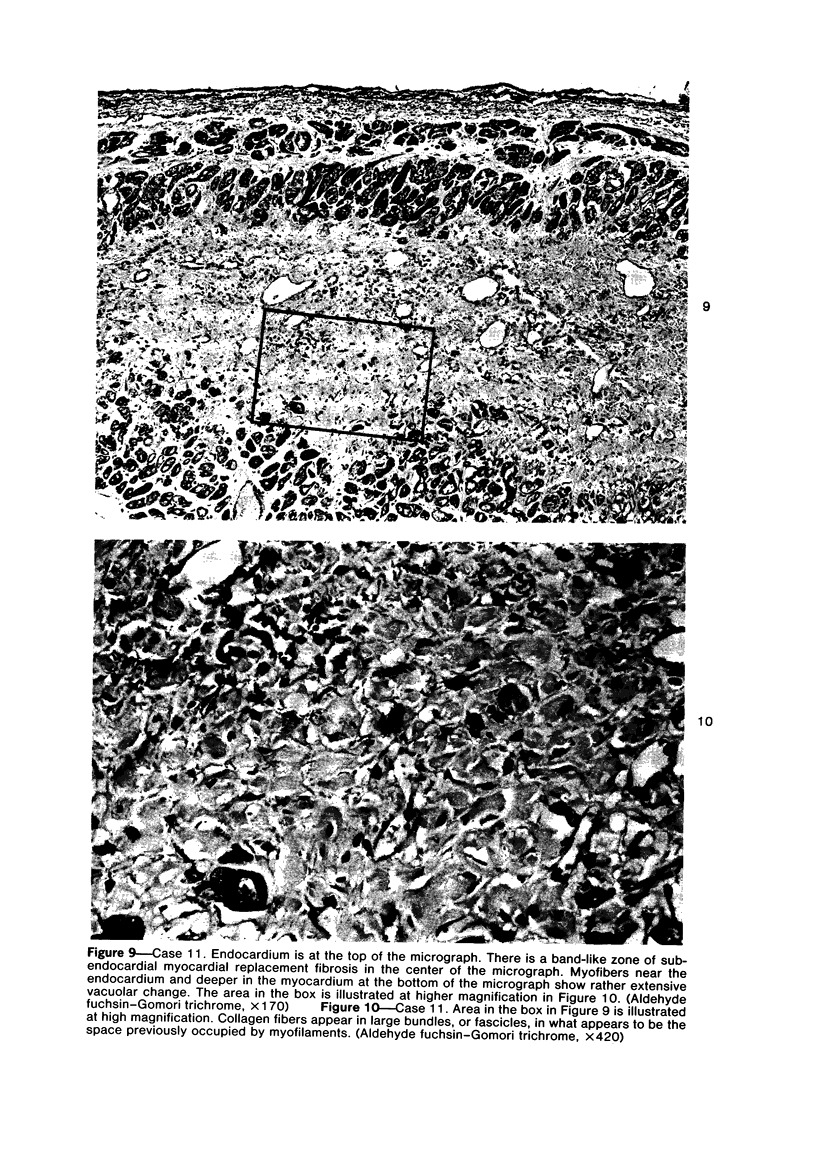
Morphologic changes in the subendocardial myocardium that appeared to be caused by severe, chronic subendocardial ischemia were studied in patients with fatal ischemic heart disease admitted to the Specialized Center of Research for Ischemic Heart Disease at the University of Alabama in Birmingham in the period 1970--1977. Thirteen patients were selected for this report on the basis that they had the lesions in the subendocardial myocardium we believe to have been caused by subendocardial ischemia and had no evidence of acute or remote myocardial infarction or other conditions that may have contributed to their terminal illness or death. Clinical findings were unstable angina, congestive heart failure, usually no increase in plasma enzymes indicative of myocardial damage, and electrocardiographic changes consistent with subendocardial ischemia. All 13 patients had 75% or greater stenosis of the three major coronary arteries; none had acute thrombotic or embolic coronary artery occlusion. The left ventricle in all cases was hypertrophied. The subendocardial myocardium showed circumferential pallor, hyperemia, or focal fibrosis without perceptible loss of volume in papillary muscles or trabeculae carneae. Microscopically, acute lesions showed one to two layers of preserved myofibers adjacent to the endocardium, vacuolar change in the deeper fibers, and focal areas of coagulation necrosis of variable size in the myocardium external to the fibers with vacuolar change. Coagulation necrosis was extensive in some cases and usually was not associated with infiltration of neutrophils. The repair reaction involved removal of necrotic sarcoplasm by mononuclear phagocytes, resulting in a reticular-appearing tissue without evidence of stromal collapse. Granulation tissue was not seen. Collagen fibers appeared to be deposited within the area of previous sarcolemmal sheaths. The distribution and morphology of subendocardial myocardial lesions associated with severe coronary atherosclerosis are distinctive and can be distinguished from myocardial necrosis or fibrosis associated with acute total occlusion of a coronary artery.
Full text
PDF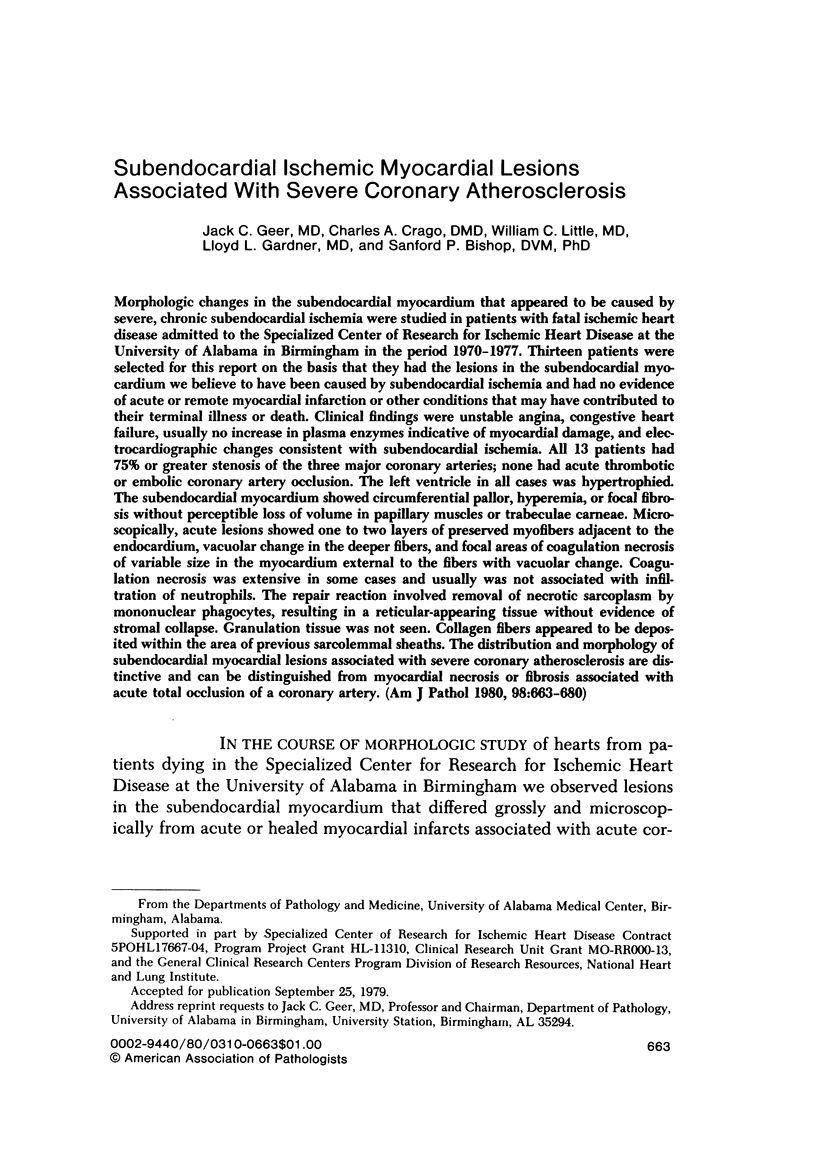

Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baroldi G. Different types of myocardial necrosis in coronary heart disease: a pathophysiologic review of their functional significance. Am Heart J. 1975 Jun;89(6):742–752. doi: 10.1016/0002-8703(75)90189-1. [DOI] [PubMed] [Google Scholar]
- Bouch D. C., Montgomery G. L. Cardiac lesions in fatal cases of recent myocardial ischaemia from a coronary care unit. Br Heart J. 1970 Nov;32(6):795–803. doi: 10.1136/hrt.32.6.795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brand F. R., Brown A. L., Jr, Berge K. G. Histology of papillary muscles of the left ventricle in myocardial infarction. Am Heart J. 1969 Jan;77(1):26–32. doi: 10.1016/0002-8703(69)90126-4. [DOI] [PubMed] [Google Scholar]
- Buja L. M., Poliner L. R., Parkey R. W., Pulido J. I., Hutcheson D., Platt M. R., Mills L. J., Bonte F. J., Willerson J. T. Clinicopathologic study of persistently positive technetium-99m stannous pyrophosphate myocardial scintigrams and myocytolytic degeneration after myocardial infarction. Circulation. 1977 Dec;56(6):1016–1023. doi: 10.1161/01.cir.56.6.1016. [DOI] [PubMed] [Google Scholar]
- Connor R. C. Focal myocytolysis and fuchsinophilic degeneration of the myocardium of patients dying with various brain lesions. Ann N Y Acad Sci. 1969 Jan 31;156(1):261–270. doi: 10.1111/j.1749-6632.1969.tb16732.x. [DOI] [PubMed] [Google Scholar]
- Donsky M. S., Curry G. C., Parkey R. W., Meyer S. L., Bonte F. J., Platt M. R., Willerson J. T. Unstable angina pectoris. Clinical, angiographic, and myocardial scintigraphic observations. Br Heart J. 1976 Mar;38(3):257–263. doi: 10.1136/hrt.38.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- HASPER B. ULTRAMIKROSKOPISCHE HERZMUSKELVERAENDERUNGEN NACH WIEDERHOLTER HYPOXIE. Beitr Pathol Anat. 1964 Aug;130:321–351. [PubMed] [Google Scholar]
- HORN H., FIELD L. E., DACK S., MASTER A. M. Acute coronary insufficiency: pathological and physiological aspects; an analysis of twenty-five cases of subendocardial necrosis. Am Heart J. 1950 Jul;40(1):63–80. doi: 10.1016/0002-8703(50)90150-5. [DOI] [PubMed] [Google Scholar]
- Heggtveit H. A. Morphological alterations in the ischaemic heart. Cardiology. 1971;56(1):284–290. doi: 10.1159/000169372. [DOI] [PubMed] [Google Scholar]
- LEVINE H. D., FORD R. V. Subendocardial infarction; report of six cases and critical survey of the literature. Circulation. 1950 Feb;1(2):246–263. doi: 10.1161/01.cir.1.2.246. [DOI] [PubMed] [Google Scholar]
- LODGE-PATCH I. The ageing of cardiac infarcts, and its influence on cardiac rupture. Br Heart J. 1951 Jan;13(1):37–42. doi: 10.1136/hrt.13.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poliner L. R., Buja L. M., Parkey R. W., Bonte F. J., Willerson J. T. Clinicopathologic findings in 52 patients studied by technetium-99m stannous pyrophosphate myocardial scintigraphy. Circulation. 1979 Feb;59(2):257–267. doi: 10.1161/01.cir.59.2.257. [DOI] [PubMed] [Google Scholar]
- SCHLESINGER M. J., REINER L. Focal myocytolysis of the heart. Am J Pathol. 1955 May-Jun;31(3):443–459. [PMC free article] [PubMed] [Google Scholar]
- SCHWARTZ C. J., MITCHELL J. R. The relation between myocardial lesions and coronary artery disease. I. An unselected necropsy study. Br Heart J. 1962 Nov;24:761–786. doi: 10.1136/hrt.24.6.761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sugiura M., Okada R., Iizuka H. A clinicopathological study on the subendocardial infarction in the aged. Jpn Heart J. 1969 May;10(3):203–217. doi: 10.1536/ihj.10.203. [DOI] [PubMed] [Google Scholar]
- Sulkin N. M., Sulkin D. F. An electron microscopic study of the effects of chronic hypoxia on cardiac muscle, hepatic, and autonomic ganglion cells. Lab Invest. 1965 Aug;14(8):1523–1546. [PubMed] [Google Scholar]