Abstract
1. Ligustrazine (tetramethylpyrazine, TMP) is a vasodilator that has been reported to have pulmonary selective properties in vivo, but not in vitro. Although TMP is generally described as being endothelium-independent, we provide evidence here that TMP may have an endothelium-dependent and nitric oxide (NO)-mediated mechanism in pulmonary arteries that could predominate at concentrations used therapeutically in China. 2. The study was performed on isolated pulmonary (1-2 mm i.d.), intrapulmonary (200-850 microns) and mesenteric (200-400 microns) arteries of the rat using a Mulvaney-Halpen small vessel myograph, following preconstriction with phenylephrine (PE, 10 microM), prostaglandin F2 alpha (PGF2 alpha, 100 microM), or 75 mM K+ (KPSS, equimolar substitution for Na+). Values are shown as mean +/- s.e.mean, or for EC50S as mean [+/-95% confidence limits]. 3. TMP caused a concentration-dependent relaxation against all three agonists in both large (1.56 +/- 0.04 mm) and small (399 +/- 20 microM) pulmonary arteries; it was more potent in small compared to large arteries constricted with PE or PGF2 alpha (P < 0.05), but not those constricted with KPSS. The NO synthase (NOS) inhibitor, NG-monomethyl-L-arginine (L-NMMA, 100 microM) caused a significant shift to the right of these relationships, such that the EC50 for TMP in large pulmonary arteries constricted with PE increased from 522 [+130, -104] microM (n = 12) to 1828 [+395, -325] microM (n = 6, P < 0.01). Both removal of the endothelium and methylene blue (10 microM) had similar effects. 4. L-Arginine substantially reduced the EC50 for TMP in pulmonary arteries; in the presence of 400 microM L-arginine the EC50 for TMP in large arteries constricted with PE was 14.7 [+21.0, -8.6] microM, (n = 6, P < 0.001), and with 10 microM L-arginine 96.7 [+45.1, -30.7] microM, (n = 6, P < 0.001). Similar effects were seen in small arteries. L-Arginine had no effect in the absence of an endothelium. D-Arginine was ineffective, and inhibition of L-arginine uptake with L-lysine blocked the action of L-arginine. L-Arginine (400 microM) had no significant effect on TMP-induced relaxation in mesenteric arteries (n = 5). 5. L-Arginine itself caused a concentration-dependent relaxation in intrapulmonary arteries (639 +/- 34 microM) constricted with PE, reaching a maximum relaxation around 100-400 microM (42.4 +/- 3.0%, n = 16), but this was independent of the endothelium. TMP (10 and 100 microM) significantly enhanced the relaxation to L-arginine, with a maximum relaxation in the presence of 100 microM TMP of 81.7 +/- 6.2% (n = 5, P < 0.01), but the effect of TMP was entirely dependent on the endothelium. A similar effect was observed in PGF2 alpha-constricted pulmonary arteries. 6. These results show that TMP stimulates NO production at low concentrations in pulmonary arteries, via an apparently novel endothelium-resident mechanism that is dependent on exogenous L-arginine. Normal plasma L-arginine levels of around 150 microM would allow this mechanism to be maximally activated. As mesenteric arteries do not seem to express the mechanism to any significant extent, at low concentrations TMP would be effectively selective to the pulmonary vasculature, and may thus have potential as a therapeutic agent in pulmonary vascular disease.
Full text
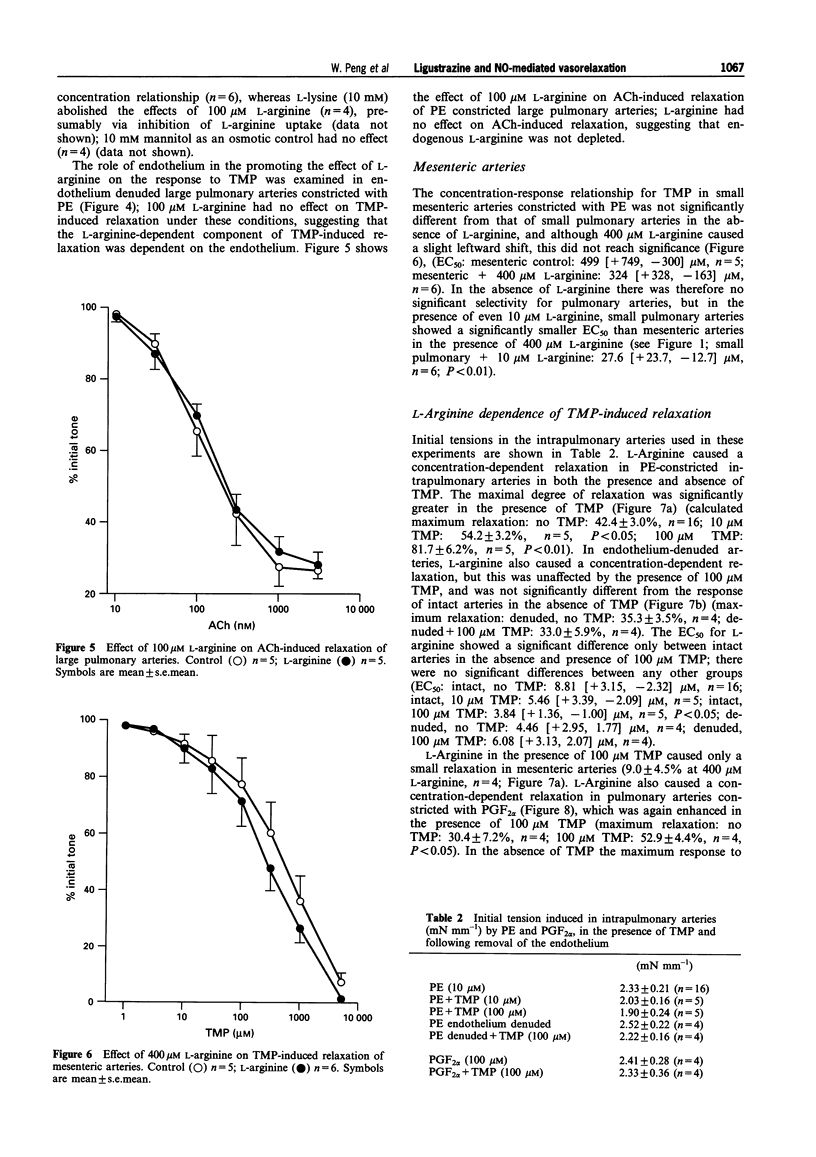
PDF

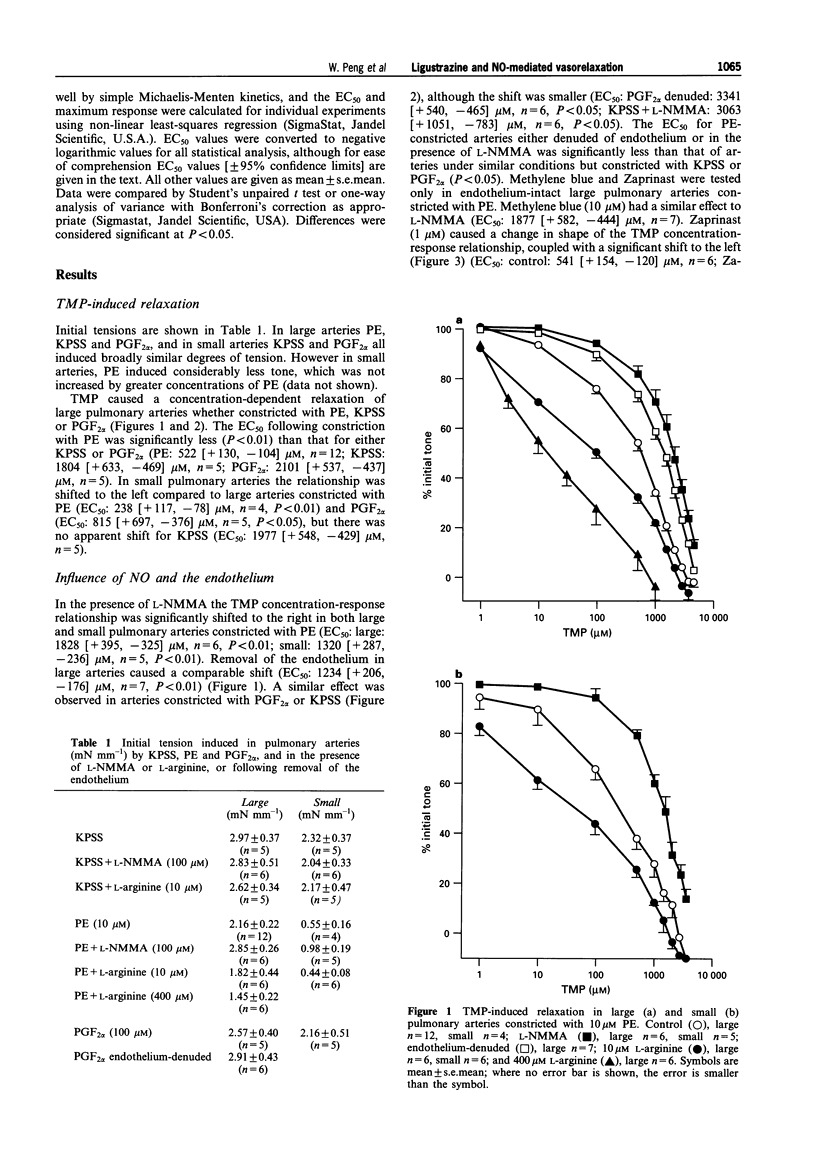
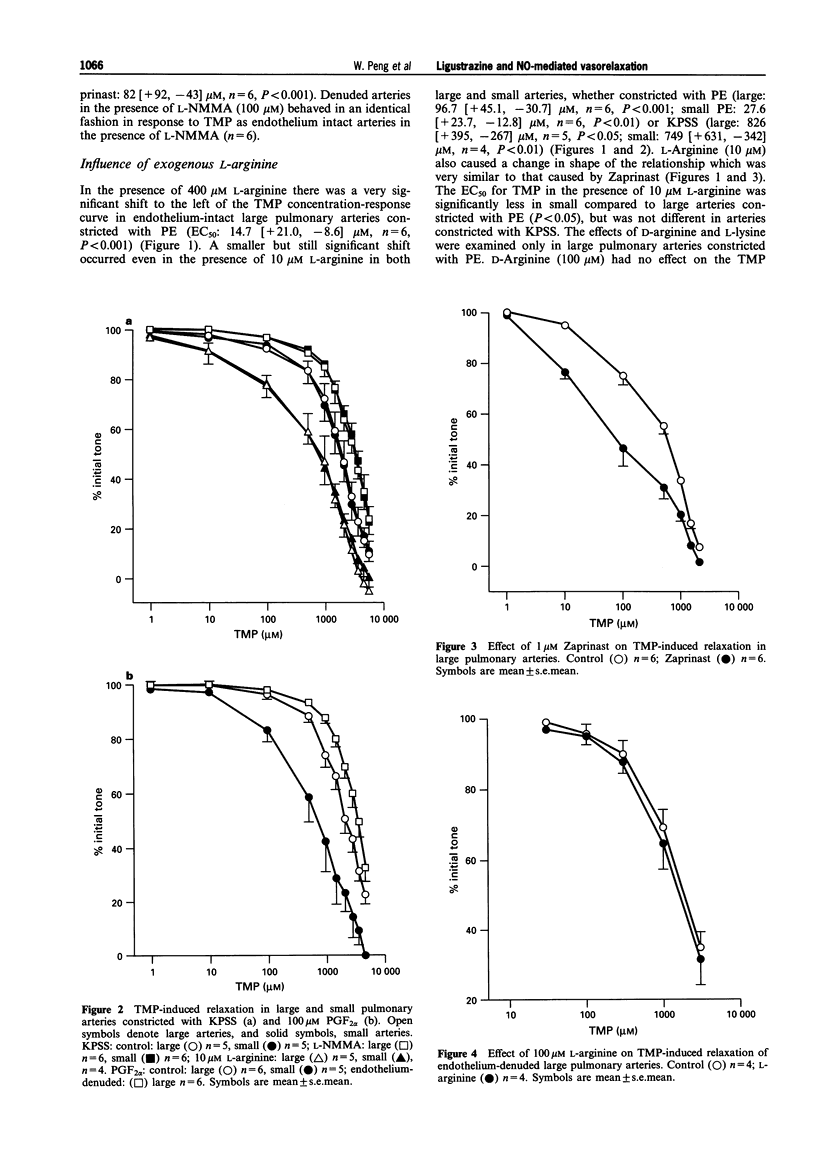
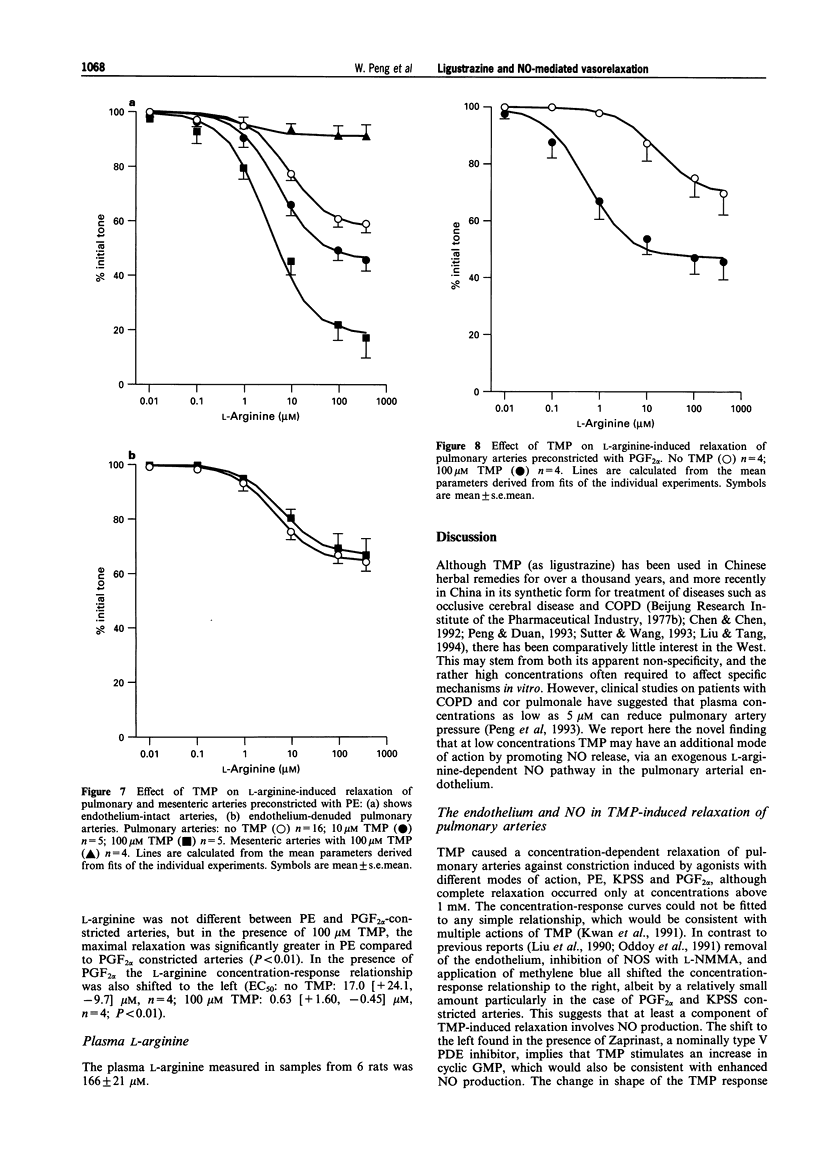


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Baydoun A. R., Emery P. W., Pearson J. D., Mann G. E. Substrate-dependent regulation of intracellular amino acid concentrations in cultured bovine aortic endothelial cells. Biochem Biophys Res Commun. 1990 Dec 31;173(3):940–948. doi: 10.1016/s0006-291x(05)80876-9. [DOI] [PubMed] [Google Scholar]
- Buckley B. J., Mirza Z., Whorton A. R. Regulation of Ca(2+)-dependent nitric oxide synthase in bovine aortic endothelial cells. Am J Physiol. 1995 Sep;269(3 Pt 1):C757–C765. doi: 10.1152/ajpcell.1995.269.3.C757. [DOI] [PubMed] [Google Scholar]
- Cai Y. N., Barer G. R. Effect of ligustrazine on pulmonary vascular changes induced by chronic hypoxia in rats. Clin Sci (Lond) 1989 Nov;77(5):515–520. doi: 10.1042/cs0770515. [DOI] [PubMed] [Google Scholar]
- Cai Y. N., Bee D., Barer G. Pulmonary vasodilator action of ligustrazine, active principle of a traditional Chinese remedy, in rats and ferrets. Proc Chin Acad Med Sci Peking Union Med Coll. 1989;4(3):147–152. [PubMed] [Google Scholar]
- Cao W., Luo W., Guo Z. [Effects of ligustrazine and nitroglycerine on acute hypoxic pulmonary hypertension in anesthetized dogs]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 1994 Apr;16(2):79–83. [PubMed] [Google Scholar]
- Kwan C. Y., Daniel E. E., Chen M. C. Inhibition of vasoconstriction by tetramethylpyrazine: does it act by blocking the voltage-dependent Ca channel? J Cardiovasc Pharmacol. 1990 Jan;15(1):157–162. [PubMed] [Google Scholar]
- Kwan C. Y., Gaspar V., Shi A. G., Wang Z. L., Chen M. C., Ohta A., Cragoe E. J., Jr, Daniel E. E. Vascular effects of tetramethylpyrazine: direct interaction with smooth muscle alpha-adrenoceptors. Eur J Pharmacol. 1991 May 30;198(1):15–21. doi: 10.1016/0014-2999(91)90556-6. [DOI] [PubMed] [Google Scholar]
- Kwan C. Y. Plant-derived drugs acting on cellular Ca2+ mobilization in vascular smooth muscle: tetramethylpyrazine and tetrandrine. Stem Cells. 1994 Jan;12(1):64–67. doi: 10.1002/stem.5530120111. [DOI] [PubMed] [Google Scholar]
- Leach R. M., Robertson T. P., Twort C. H., Ward J. P. Hypoxic vasoconstriction in rat pulmonary and mesenteric arteries. Am J Physiol. 1994 Mar;266(3 Pt 1):L223–L231. doi: 10.1152/ajplung.1994.266.3.L223. [DOI] [PubMed] [Google Scholar]
- Leach R. M., Twort C. H., Cameron I. R., Ward J. P. A comparison of the pharmacological and mechanical properties in vitro of large and small pulmonary arteries of the rat. Clin Sci (Lond) 1992 Jan;82(1):55–62. doi: 10.1042/cs0820055. [DOI] [PubMed] [Google Scholar]
- Li Y. J., Li Y. J., Wu J. X., Yu X. J., Yan Y. F. Protective effect of tetramethylpyrazine against damages of aortic endothelial cells elicited by low-density lipoproteins. Zhongguo Yao Li Xue Bao. 1994 Sep;15(5):407–410. [PubMed] [Google Scholar]
- Lin C. I., Wu S. L., Tao P. L., Chen H. M., Wei J. The role of cyclic AMP and phosphodiesterase activity in the mechanism of action of tetramethylpyrazine on human and dog cardiac and dog coronary arterial tissues. J Pharm Pharmacol. 1993 Nov;45(11):963–966. doi: 10.1111/j.2042-7158.1993.tb05636.x. [DOI] [PubMed] [Google Scholar]
- Liu S. F., Cai Y. N., Evans T. W., McCormack D. G., Barer G. R., Barnes P. J. Ligustrazine is a vasodilator of human pulmonary and bronchial arteries. Eur J Pharmacol. 1990 Dec 4;191(3):345–350. doi: 10.1016/0014-2999(90)94167-v. [DOI] [PubMed] [Google Scholar]
- Liu S. M., Tang T. Q. [Clinical and experimental studies of feiyaning in treating pulmonary arterial hypertension in cor pulmonale]. Zhongguo Zhong Xi Yi Jie He Za Zhi. 1994 Aug;14(8):469–473. [PubMed] [Google Scholar]
- Liu S. Y., Sylvester D. M. Antiplatelet activity of tetramethylpyrazine. Thromb Res. 1994 Jul 1;75(1):51–62. doi: 10.1016/0049-3848(94)90139-2. [DOI] [PubMed] [Google Scholar]
- Magee F., Wright J. L., Wiggs B. R., Paré P. D., Hogg J. C. Pulmonary vascular structure and function in chronic obstructive pulmonary disease. Thorax. 1988 Mar;43(3):183–189. doi: 10.1136/thx.43.3.183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oddoy A., Bee D., Emery C., Barer G. Effects of ligustrazine on the pressure/flow relationship in isolated perfused rat lungs. Eur Respir J. 1991 Nov;4(10):1223–1227. [PubMed] [Google Scholar]
- Peng W., Duan S. F. Effects of ligustrazine controlled release capsule in chronic pulmonary heart disease. J Tongji Med Univ. 1991;11(2):101–105. doi: 10.1007/BF02888096. [DOI] [PubMed] [Google Scholar]
- Peng W., Duan S. F. [Effect of ligustrazine controlled release capsule on hemorrheology in patients with cor pulmonale]. Zhonghua Nei Ke Za Zhi. 1993 Jan;32(1):37–39. [PubMed] [Google Scholar]
- Pollock J. S., Förstermann U., Mitchell J. A., Warner T. D., Schmidt H. H., Nakane M., Murad F. Purification and characterization of particulate endothelium-derived relaxing factor synthase from cultured and native bovine aortic endothelial cells. Proc Natl Acad Sci U S A. 1991 Dec 1;88(23):10480–10484. doi: 10.1073/pnas.88.23.10480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radomski M. W., Palmer R. M., Moncada S. Glucocorticoids inhibit the expression of an inducible, but not the constitutive, nitric oxide synthase in vascular endothelial cells. Proc Natl Acad Sci U S A. 1990 Dec;87(24):10043–10047. doi: 10.1073/pnas.87.24.10043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rebich S., Devine J. O., Armstead W. M. Role of nitric oxide and cAMP in beta-adrenoceptor-induced pial artery vasodilation. Am J Physiol. 1995 Mar;268(3 Pt 2):H1071–H1076. doi: 10.1152/ajpheart.1995.268.3.H1071. [DOI] [PubMed] [Google Scholar]
- Sutter M. C., Wang Y. X. Recent cardiovascular drugs from Chinese medicinal plants. Cardiovasc Res. 1993 Nov;27(11):1891–1901. doi: 10.1093/cvr/27.11.1891. [DOI] [PubMed] [Google Scholar]
- Wang Y. L., Ba Y. K. [Effect of Ligustrazini (a new calcium antagonist?) on cardiovascular tissue: pharmacodynamic and electrophysiological studies]. Zhong Xi Yi Jie He Za Zhi. 1985 May;5(5):291-4, 320, 260. [PubMed] [Google Scholar]
- Zhang Z. H., Yu S. Z., Wang Z. T., Zhao B. L., Hou J. W., Yang F. J., Xin W. J. Scavenging effects of tetramethylpyrazine on active oxygen free radicals. Zhongguo Yao Li Xue Bao. 1994 May;15(3):229–231. [PubMed] [Google Scholar]


