Abstract
Objective To determine the efficacy of oral morphine in relieving the sensation of breathlessness in patients in whom the underlying aetiology is maximally treated.
Design Randomised, double blind, placebo controlled crossover study.
Setting Four outpatient clinics at a hospital in South Australia.
Participants 48 participants who had not previously been treated with opioids (mean age 76, SD 5) with predominantly chronic obstructive pulmonary disease (42, 88%) were randomised to four days of 20 mg oral morphine with sustained release followed by four days of identically formulated placebo, or vice versa. Laxatives were provided as needed.
Main outcome measures Dyspnoea in the morning and evening as shown on a 100 mm visual analogue scale, quality of sleep, wellbeing, performance on physical exertion, and side effects as measured at the end of the four day treatment period.
Results 38 participants completed the study; three withdrew because of definite and two because of possible side effects of morphine (nausea, vomiting, and sedation). Participants reported significantly different dyspnoea scores when treated with morphine: an improvement of 6.6 mm (95% confidence interval 1.6 mm to 11.6 mm) in the morning and of 9.5 mm (3.0 mm to 16.1 mm) in the evening (P = 0.011 and P = 0.006, respectively). During the period in which they were taking morphine participants also reported better sleep (P = 0.039). More participants reported distressing constipation while taking morphine (9 v 1, P = 0.021) in spite of using laxatives. All other side effects were not significantly worse with morphine, although the study was not powered to address side effects.
Conclusions Sustained release, oral morphine at low dosage provides significant symptomatic improvement in refractory dyspnoea in the community setting.
Introduction
Breathlessness is a source of distress for 50-70% of patients requiring palliative care.1 A complex physiological and psychological sensation, its causes are often multifactorial, including the underlying disease, cachexia, and deconditioning.1,2 As disease progresses dyspnoea occurs more frequently and at rest.1,3 Depression, panic, anxiety, and insomnia can all result from the symptom and exacerbate it.4,5 Family and carers feel helpless as they face their distressed relative.
Despite optimal medical management many people are still breathless.2 Non-pharmacological approaches such as cognitive behaviour therapy, relaxation, breathing control, and cool air flowing from a fan directed at the face have provided some benefit.6 Respiratory rehabilitation is generally aimed at improving level of function rather than definitive symptomatic benefit.7
Some clinicians acknowledge that opioids have a role in the management of intractable dyspnoea.8-10 In Australia, consensus guidelines from the Therapeutic Guidelines Group in Palliative Care conclude that opioids contribute to the management of refractory dyspnoea.10 By contrast, the consensus summary of the Global Initiative on Chronic Obstructive Lung Disease (GOLD) of the National Heart, Lung, and Blood Institute of the US National Institutes of Health and the World Health Organization states that opioids are contraindicated in the management of dyspnoea in chronic obstructive pulmonary disease.11 Concerns about respiratory depression and hypercapnia are cited.
The lack of consensus is understandable since high quality studies evaluating the role of opioids in the management of dyspnoea have been lacking. A meta-analysis of the double blind, randomised, placebo controlled studies to date indicates that oral or parenteral opioids are beneficial, but this conclusion is based on small trials using different opioids, methods, and outcomes.9 Many of the studies thus far have focused on trying to establish whether opioids can improve function in the setting of dyspnoea. For patients, the relief of the sensation of dyspnoea is critical.8,12
We evaluated the ability of opioids to relieve the sensation of breathlessness when the underlying aetiology has been maximally treated. We chose oral, sustained release morphine to reflect practical clinical care for outpatients. Our hypothesis was that morphine would be superior to placebo.
Methods
Participants
We recruited participants during April-November 2001, from the outpatient clinics for respiratory, cardiac, general, and palliative medicine at the Repatriation General Hospital in South Australia. Participants needed to be opioid naive (not formerly treated with long term opioids) adults with dyspnoea at rest in spite of receiving optimal treatment of reversible factors. Optimal treatment was considered to be in place if a specialist for respiratory, cardiac, or palliative care had reviewed the clinical case, examined the patient, and treated all identified reversible causes of the dyspnoea. Other inclusion criteria were serum concentration of creatinine within twice the normal range, stable needs for oxygen and medication, and the ability to fill out diary cards. Exclusion criteria were recent use of opioids, confusion, obtundation, adverse reactions to opioids, and history of substance misuse.
Protocol
Baseline assessment on day 0 included recording the participant's demographic characteristics, medical history, physical examination, vital signs, medications, and oxygen requirements. We measured performance status by using the categorical scale of the Eastern Cooperative Oncology Group (ECOG), where 0 is “fully active” and 4 is “completely disabled.”13
This was an eight day, randomised, double blind, crossover study. Participants received 20 mg oral morphine sulphate with sustained release (Kapanol, Glaxo Wellcome Australia) in the morning for four days, followed by four days of identically formulated placebo, or vice versa. They also received open label docusate sodium (50 mg) plus senna (8 mg) capsules (Coloxyl with Senna, Sigma) and were advised to take up to four daily as needed.
Since the active medication was a sustained release preparation we defined steady state as five times the period from administration to maximum concentration. For the product used the time to maximum concentration was nine to 12 hours. Steady state was between 45 and 60 hours. Outcome measures on days 4 and 8 provided steady state data. The design did not include a washout period. We defined the analysis a priori to compare the results at the end of each period rather than the differences between the end of the period and baseline for the period.14,15
Participants filled out diary cards each morning and evening on days 1-8 to ensure consistent reporting. Study nurses visited on days 4 and 8 and telephoned on days 2 and 6 to answer questions and assess safety. Medication bottles were collected at the end of the study to document compliance.
The primary outcome variable was the sensation of dyspnoea as measured on a visual analogue scale in the evening on the final day of the period.16 Anchors were “no breathlessness” at 0 mm and “worst possible breathlessness” at 100 mm. Other variables included morning dyspnoea on the scale, exercise tolerance measured on the modified scale of the Medical Research Council of Great Britain, respiratory rate, blood pressure, heart rate, oxygen saturation, disturbance of sleep by breathlessness, and four or five point categorical scales for nausea and vomiting, constipation, confusion, somnolence, appetite, and overall well-being.17 Study nurses used a categorical scale to evaluate any sedation.
Assignment and blinding
Randomisation and blinding were coordinated through the hospital pharmacy's centralised service. This included computerised generation of the allocation sequence in random permuted blocks and blinded disbursement of medication. After review of eligibility and consent, participants were randomised to four days of taking active drug followed by four days of taking placebo, or vice versa. The placebo medication was identical in appearance and taste to the active medication; the bottle indicated which medication to take each day. Participants were unblinded to the investigators for serious adverse events only.
Sample size
We calculated the sample size by using previous reports of improvement in dyspnoea with morphine and local expectations for data variability in this crossover study; the predicted standard deviation of the visual analogue scale was 16 mm.16 We estimated that 48 participants would provide 80% power to detect a 10 mm difference in the scale, with an α of 0.05, allowing for a 20% dropout rate.
Statistical analysis
We prespecified all analyses on an intention to treat basis. Data were double entered, and we used SPSS for Windows, version 11.0, for our statistical analysis. We used descriptive statistics to summarise the population's characteristics, breathlessness, and side effects.
We evaluated sequence and period effects before testing for any treatment effect; if either was identified we did not conduct an analysis of the treatment.14,18 We used Student's t test, χ2 test, and Fisher's exact test to evaluate sequence effects and the paired samples t test and McNemar's test to evaluate period effects. We approached analysis of the treatment effect in this two period, crossover trial by looking at the differences in the final result for each period.14 Since data on the visual analogue scale were acceptably normally distributed we used the paired samples t test to test relations for this continuous variable. We used McNemar's test for relations between categorical variables. We reported two tailed P values and assumed statistical significance if P < 0.05. We conducted sensitivity analysis by modelling worsening dyspnoea from baseline for patients who had withdrawn, by increasing end period morphine scores on the visual analogue scale by 5-30%.
Results
Flow of participants and follow up
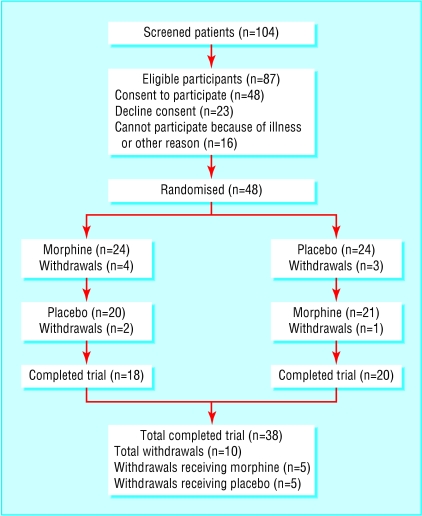
Figure 1 shows the progress of participants through the study. Ten participants withdrew; five during the morphine period and five during the placebo period. Thirty eight participants completed the study, and compliance with the intervention and follow up were complete for all participants.
Figure 1.
Flow of participants through the trial
Participants were mainly elderly men with chronic obstructive pulmonary disease who were receiving supplemental oxygen (table 1). Functional status was generally poor, with 71% (34) unable to carry out any work activities (ECOG ≥ 2). Baseline characteristics were similar for both groups.
Table 1.
Baseline characteristics of participants (n=48). Values are numbers (percentages) unless otherwise indicated
| Characteristic | |
|---|---|
| Mean (SD) age in years | 76 (5) |
| Male sex | 35 (73) |
| Dominant aetiology of dyspnoea: | |
| Chronic obstructive pulmonary disease | 42 (88) |
| Cancer | 3 (6) |
| Motor neurone disease | 1 (2) |
| Restrictive lung disease | 2 (4) |
| Receiving supplemental oxygen | 34 (71) |
| Mean (SD) litres per minute | 1.4 (1.2) |
| ECOG performance status score: | |
| 0=fully active | 0 (0) |
| 1=restricted in strenuous activity only | 14 (29) |
| 2=unable to work; up and about more than 50% of waking hours | 20 (42) |
| 3=confined to bed or chair more than 50% of waking hours | 13 (27) |
| 4=completely disabled; totally confined to bed or chair | 1 (2) |
| Respiratory rate in breaths per minute (SD) | 20 (4) |
| Mean (SD) haemoglobin (mmol/l) | 8.4 (1.1) |
| Mean (SD) morning dyspnoea score (VAS) | 43 (26) |
| Mean (SD) morning dyspnoea score (VAS) range | 2-92 |
ECOG=Eastern Cooperative Oncology Group.
VAS=visual analogue score.
Sequence and period analysis
A sequence effect is noted when a difference occurs in response to treatment in period 1 compared with period 2, most commonly seen because an effect from active treatment is carried over into the outcome measurements of the next period. A period effect is noted when the underlying condition or ability to respond to treatment changes from one period to the next. In a crossover design, responses to treatment are suspect if any sequence or period effects are noted. In this study, we identified no notable sequence or period effects.
Treatment analysis
Dyspnoea control
At the end of the four day period, sustained release morphine was superior to placebo in diminishing dyspnoea (table 2). In the evening morphine resulted in an improvement of 9.5 mm (SD 19, 95% confidence interval 3.0 mm to 16.1 mm, P = 0.006) in the reported dyspnoea score on the visual analogue scale. In the morning morphine resulted in an improvement of 6.6 mm (SD 15, 1.6 mm to 11.6 mm, P = 0.011). Significantly fewer participants receiving morphine reported that their sleep was disturbed by breathlessness (1 v 8, P = 0.039; table 3). Exertional performance and overall sense of wellbeing were not significantly different (data not presented).
Table 2.
Effect of morphine versus placebo on the sensation of dyspnoea at the end of the treatment period. End period values for morphine and placebo are means (SD). In this paired t test the differences in the same patient between morphine and placebo are presented as absolute values of the means (SD); 95% confidence intervals are also absolute values
|
Dyspnoea*
|
|||||
|---|---|---|---|---|---|
| Morphine (n=38) | Placebo (n=38) | Mean improvement in dyspnoea scores on morphine compared with placebo | 95% Cl of the mean improvement | P value (paired t test) | |
| Morning | 40.1 (24) | 47.7 (26) | 6.6 (15) | 1.6 to 11.6 | 0.011 |
| Evening | 40.3 (23) | 49.9 (24) | 9.5 (19) | 3.0 to 16.1 | 0.006 |
Dyspnoea is measured on a 100 mm visual analogue scale (VAS), with zero as “no breathlessness” and 100 as “worst possible breathlessness.”
Table 3.
Effect of morphine versus placebo on sleep at the end of the four day treatment period. Variable is measured on a categorical scale; response items are collapsed into dichotomous functional groupings. Values are numbers
|
Sleep disturbed by breathlessness on placebo
|
|||
|---|---|---|---|
| Sleep disturbed by breathlessness on morphine | Yes | No | Totals |
| Yes | 4 | 1 | 5 |
| No | 8 | 25 | 33 |
| Totals | 12 | 26 | 38 |
| P=0.039 | |||
Side effects
The respiratory rate was similar for patients receiving morphine (mean 20, SD 5) and placebo (mean 21, SD 4; P = 0.143). No episodes of severe sedation or obtundation were recorded. Side effects potentially attributable to morphine were quantified. Categorical responses were collapsed into categories for “no” or “mild” distress and “moderate” or “severe” distress. Morphine caused more distressing constipation than placebo (9 v 1, P = 0.021; table 44). Neither treatment caused significantly more distressing vomiting, confusion, sedation, or suppression of appetite (data not presented).
Table 4.
Effect of morphine versus placebo on constipation at the end of the four day treatment period. Variable is measured on a categorical scale; response items are collapsed into dichotomous functional groupings. Values are numbers
|
|
Constipation on placebo
|
||
|---|---|---|---|
| Constipation on morphine | None or mild | Moderate or severe | Totals |
| None or mild | 26 | 1 | 27 |
| Moderate or severe | 9 | 1 | 10 |
| Totals | 35 | 2 | 37 |
| P=0.021 | |||
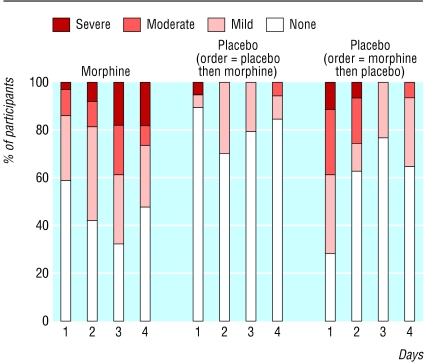
As the occurrence of a side effect may have changed over the treatment period, the frequency of symptoms throughout the treatment period was reviewed. The morphine group consistently reported more constipation across the period. When morphine was administered first, the carry over of constipation into the placebo period was resolved by the end of the placebo period (figure 2). Other symptoms were relatively stable across both periods; the results are not shown here.
Figure 2.
Frequency of constipation throughout the treatment periods, by treatment intervention. Data are presented as the percentage of participants indicating each categorical response on each day of the treatment period. Placebo responses are divided between participants who received placebo during the first period (first placebo, then morphine) or the second period (first morphine, then placebo) to show carry over effects
Participants' withdrawals
Ten participants withdrew from the study; three because of morphine side effects, two because of potential morphine effects, and five for reasons unlikely to be related to morphine (table 5). All of those who withdrew because of side effects of morphine reported that the symptom was causing them “moderate” or “severe” distress. Notably, one participant's dyspnoea was so improved with the first treatment (morphine) that the participant withdrew at crossover.
Table 5.
Reasons for withdrawal of 10 patients from the study
| Patient | Treatment on day of withdrawal | Day (of 8) | Reason for withdrawal | Comment |
|---|---|---|---|---|
| 1 | Morphine | 1 | Nausea and vomiting | Likely to be caused by morphine |
| 2 | Morphine | 2 | Sedation | Likely to be caused by morphine |
| 3 | Morphine | 3 | Nausea and vomiting | Likely to be caused by morphine |
| 4 | Morphine | 4 | Chest pain and nausea | Nausea may be caused by morphine |
| 5 | Morphine | 6 | Rapid atrial fibrillation, admitted to intensive care unit | Unlikely to be caused by morphine |
| 6 | Placebo | 2 | Chest infection | Not caused by morphine |
| 7 | Placebo | 2 | Fall with fracture | Not caused by morphine |
| 8 | Placebo | 4 | Wanted to take opioids for shoulder pain | Not caused by morphine |
| 9 | Placebo | 5 | Increased dyspnoea with treatment change | Likely to be caused by change from morphine to placebo; refused to continue with crossover |
| 10 | Placebo | 6 | Constipation and sedation | Likely carry over effects of morphine |
Sensitivity analysis
A conservative sensitivity analysis model assumed that all participants who withdrew did so because of problems with morphine. We included baseline scores on the visual analogue scale for the 10 withdrawn participants in the study dataset and then increased the scores for the end period on morphine systematically to model worsening dyspnoea. All participants who withdrew could have had at least a 10% worsening of their morning scores for dyspnoea or a 25% worsening of their evening scores, and the results of this study would still show a statistically significant improvement with morphine.
Discussion
Oral, sustained release morphine can provide added relief to patients who have intractable breathlessness despite maximal treatment of the underlying causes of dyspnoea. In this adequately powered, randomised controlled trial, morphine provided a 7-10 mm improvement in the visual analogue scale for dyspnoea—results with both clinical and statistical significance. These results were corroborated by participants' reports of much better sleep during the morphine period. Sensitivity analysis showed that morphine still provided clinical benefit to the study population even if the modelled participants who withdrew experienced 25% worsening of their dyspnoea. Further, the results showed the same magnitude of improvement as seen in the pooled results of other trials (8 mm on the visual analogue scale).9
The results of this study are applicable to many outpatient settings in general practice, palliative care, and respiratory care. The study population of elderly, poorly functioning people predominantly with chronic obstructive pulmonary disease represents patients we encounter often, for whom few symptomatic options are available. The criteria used to identify participants were simple and as broad as possible. Patients needed only to be suffering from the symptom of refractory breathlessness. We specifically avoided invasive procedures such as measuring arterial blood gases or pulmonary function to identify eligible candidates as this would not be generalisable or ethical for many outpatient and palliative care settings.
Oral, long acting morphine was chosen for its convenience and continuous action. The sustained release morphine product used can be given once daily; evidence for its efficacy as a 24 hour medication was provided by the dramatic improvements in the evening dyspnoea scores. A small background dose of opioid may be better tolerated than the peaks and troughs of immediate release formulations.19
Although the results are significant and generalisable, clinicians should prescribe morphine for the control of dyspnoea with care. This was not a safety study, and it was not powered to detect significant side effects. The data imply that side effects were minimal. Neither respiratory depression nor severe sedation was identified. All participants who withdrew because of morphine encountered vomiting or sedation, which may be transient or treatable. Constipation was the only notable and common side effect. Review of the daily constipation scores showed that the constipation started to improve by the fourth day of the morphine period; early intervention could have an impact. An important consideration is that most patients who would be considering this treatment do not have any other options and are otherwise severely distressed and limited by their breathlessness. Hence, although the risk of constipation and other side effects is real, this may be an appropriate treatment for many patients, provided that the patient and doctor monitor for clinical benefit and side effects together.
Limitations
The study design has several limitations. Firstly, there was no washout (no treatment) period. Figure 2 shows the persistence of the side effects of morphine into the early part of the placebo period. We recognised these risks a priori. The challenge was to develop a short protocol that would be acceptable and ethical for a group of very ill patients who did not have any other medical options. Although a parallel trial would have addressed this concern, it would have doubled numbers in a clinical population for which others have had difficulty recruiting. Instead we elected a crossover trial with an analysis plan that concentrated on the end of the treatment period only.14 We planned that sequence and period analyses would precede any analysis of treatment; fortunately, neither sequence nor period effects were identified.
Secondly, there was no blinding for constipation. To accommodate this, the only investigator aware of the constipation was the study nurse (AM), who was not involved in the analysis. Thirdly, the morphine dose chosen was 20 mg daily. Some clinicians may regard this as a relatively high dose in patients who had not been treated with opioids before. As the study was being designed it was the lowest once daily, sustained release formulation available. Subsequent dose ranging studies are needed.
Fourthly, the reduced evening dyspnoea scores and improved sleep may have been related to changes made by the participant, such as increased use of oxygen during the day or continuous positive airway pressure at night. Such potential confounders should have been equally distributed between the groups through randomisation. Finally, the clinical significance of a 7-10 mm change in the visual analogue scale may be questioned. We are not aware of any studies that correlate direct clinical meaning with specific changes of distance in the dyspnoea scale. None the less, in a population of patients in whom pharmacological treatment is not an option, the opportunity for a 5-10% improvement in a disabling symptom is welcome.
This study shows that rigorous randomised controlled trials can be performed in this population. Key factors were a short study period, simple bedside evaluation, collaboration across disciplines, one identified recruitment nurse, once daily dosing, and an evolving clinical culture that seeks evidence based approaches to care. Future directions include an effectiveness study that is adequately powered to evaluate safety. Such a study may well show that, with close monitoring, patients could continue taking opioids while tolerance develops to the nausea and sedation. Dose ranging studies in opioid tolerant and naive participants are also planned.
What is already known on this topic
Pooled data in a meta-analysis of eight small underpowered randomised trials support the clinical use of oral or parenteral opioids including morphine to manage refractory breathlessness
Clinical guidelines for the management of intractable dyspnoea in the palliative care and respiratory settings are contradictory owing to inadequate primary evidence supporting the efficacy and safety of morphine in this setting
What this study adds
This is the first adequately powered randomised controlled trial that showed the superiority of oral morphine for relief of the sensation of breathlessness.
This study was completed before the meta-analysis was published; it confirms the main findings of the meta-analysis with results of the same magnitude
The morphine administered in this study was an oral, once daily, sustained release formulation.
Side effects were minimal and no evidence of respiratory depression was found. Constipation was treated expectantly
We thank Greg Samsa of Duke University Medical Center, Durham, North Carolina, United States, and Adrian Esterman of Flinders Medical Centre, Bedford Park, South Australia, Australia, for reviewing the statistical analysis and providing critical feedback.
Contributors: APA was responsible for study design; obtaining funding; logistic, administrative, and technical support; recruitment of participants; collection, assembly, and analysis of data; statistical expertise; and data interpretation; drafting, critical revision, and final approval of the article. DCC was responsible for conception and design of the study; logistic, administrative, and technical support; analysis and interpretation of data; and drafting, critical revision, and final approval of the article. PF was responsible for study design; obtaining funding; logistic support; recruitment of participants; data interpretation; and drafting, critical revision, and final approval of the article. BSF was responsible for logistic, administrative, and technical support; recruitment of participants; collection, assembly, and analysis of data; and drafting, critical revision, and final approval of the article. AM was responsible for logistic and technical support; recruitment of participants, collection, assembly, and interpretation of data; and drafting, critical revision, and final approval of the article. CB was responsible for conception and design of the study and critical revision and final approval of the article. APA is the guarantor.
Funding: Funds for the conduct of the study were provided by the Flinders Medical Centre Foundation of Bedford Park, South Australia, Australia ($A6000; €3500; £2400). APA's salary was provided through a clinical scientist development award from the Doris Duke Charitable Foundation of New York, New York, United States.
Competing interests: Placebo capsules of identical appearance were provided by the company that manufactures sustained release morphine sulphate (Kapanol, Glaxo Wellcome Australia); no direct funds were provided by the drug company.
Ethical approval: The study was approved by the local institutional research and ethics committee, and the trial was registered with the Australian therapeutic goods administration.
References
- 1.Reuben DB, Mor V. Dyspnea in terminally ill cancer patients. Chest 1986;89: 234-6. [DOI] [PubMed] [Google Scholar]
- 2.Burdon JGW, Pain MCF, Rubinfeld AR, Nana A. Chronic lung disease and the perception of breathlessness: a clinical perspective. Eur Respir J 1994;7: 1342-9. [DOI] [PubMed] [Google Scholar]
- 3.Higginson I, McCarthy M. Measuring symptoms in terminal cancer: are pain and dyspnoea controlled? J R Soc Med 1989;82: 264-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.O'Driscoll M, Corner J, Bailey C. The experience of breathlessness in lung cancer. Eur J Cancer Care (Engl) 1999;8: 37-43. [DOI] [PubMed] [Google Scholar]
- 5.Tanaka K, Akechi T, Okuyama T, Nishiwaki Y, Uchitomi Y. Factors correlated with dyspnea in advanced lung cancer patients: organic causes and what else? J Pain Symptom Manage 2002;23: 490-500. [DOI] [PubMed] [Google Scholar]
- 6.Bredin M, Corner J, Krishnasamy M, Plant H, Bailey C, A'Hern R. Multi-centre randomised controlled trial of nursing intervention for breathlessness in patients with lung cancer. Br Med J 1999;318: 901-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.British Thoracic Society Standards of Care Subcommittee on Pulmonary Rehabilitation. Pulmonary rehabilitation. Thorax 2001;56: 827-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ripamonti C. Management of dyspnea in advanced cancer patients. Support Care Cancer 1999;7: 233-43. [DOI] [PubMed] [Google Scholar]
- 9.Jennings AL, Davies AN, Higgins JP, Gibbs JS, Broadley KE. A systematic review of the use of opioids in the management of dyspnoea. Thorax 2002;57: 939-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mashford ML, Aranda S, Ashby M, Bowman J, Brooksbank M, Cairns W, et al. Therapeutic Guidelines Palliative Care. Version 1. North Melbourne, Victoria, Australia: Therapeutic Guidelines Limited, 2001.
- 11.Pauwels RA, Buist AS, Calverley PM, Jenkins CR, Hurd SS. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. NHLBI/WHO Global Initiative for Chronic Obstructive Lung Disease (GOLD) Workshop summary. Am J Respir Crit Care Med 2001;163: 1256-76. [DOI] [PubMed] [Google Scholar]
- 12.Chua TP, Harrington D, Ponikowski P, Webb-Peploe K, Poole-Wilson PA, Coats AJ. Effects of dihydrocodeine on chemosensitivity and exercise tolerance in patients with chronic heart failure. J Am Coll Cardiol 1997;29: 147-52. [DOI] [PubMed] [Google Scholar]
- 13.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 1982;5: 649-55. [PubMed] [Google Scholar]
- 14.Hills M, Armitage P. The two-period cross-over clinical trial. Br J Clin Pharmacol 1979;8: 7-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sibbald B, Roberts C. Understanding controlled trials. Crossover trials. Br Med J 1998;316: 1719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mazzocato C, Buclin T, Rapin CH. The effects of morphine on dyspnea and ventilatory function in elderly patients with advanced cancer: a randomized double-blind controlled trial. Ann Oncol 1999;10: 1511-4. [DOI] [PubMed] [Google Scholar]
- 17.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax 1999;54: 581-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grizzle JE. The two-period change-over design and its use in clinical trials. Biometrics 1965(June): 467-80. [PubMed]
- 19.Robin ED, Burke CM. Single-patient randomized clinical trial. Opiates for intractable dyspnea. Chest 1986;90: 888-92.- [DOI] [PubMed] [Google Scholar]