Abstract
The aim of this study was to investigate the immunolocalization and the existence of thyroid hormone receptors (THR) (alpha1/alpha2) in rat uterus and oviduct. For this purpose 6 female Wistar albino rats found in estrous period were used. Tissue samples fixed in 10% neutral formalin were examined immunohistochemically. Sections were incubated with primary mouse-monoclonal THR (alpha1/alpha2) antibody. In uterus, THR (alpha1/alpha2) immunoreacted strongly with uterine luminal epithelium, endometrial gland epithelium and endometrial stromal cells and, moderately with myometrial smooth muscle. In oviduct, they were observed moderately in the epithelium of the tube and the smooth muscle cells of the muscular layer.
In conclusion, the presence of THR in uterus and oviduct suggests that these organs are an active site of thyroid hormones.
Keywords: uterus, oviduct, THR (alpha1/alpha2), immunohistochemistry, rat
I. Introduction
Thyroid hormones (THs) play an important role in reproduction and are essential for development in vertebrate species. It has been reported that hypothyroidism in women causes irregular menstruation, frank infertility and difficulty in maintaining pregnancy [10], and hypothyroidism in rodents induces alterations in the estrous cycle and uterine morphology [13]. It has been reported that thyroidectomy causes a decrease in basal plasma levels of luteinizing hormone (LH) and follicle stimulating hormone (FSH) [8, 28].
Thyroid hormone receptors (THR) mediate the cellular response to thyroid hormone (T3) by regulating target gene transcription. THR are the products of two different genes, erbAα and erbAβ. The mammalian erbAα gene produces two mRNAs, erbAα1 (alpha1) and erbAα2 (alpha2). Alpha1 codes for the alpha-thyroid hormone receptor (TRα1), whereas alpha2 codes for an orphan nuclear receptor (TRα2) which does not bind T3. TRα2 competes with TRα1 and TRβ for specific DNA binding sites, thereby antagonizing T3 action. Because the erbAα gene produces both a transcriptional activator (TRα1) and its specific inhibitor (TRα2), regulation of the alternative processing of alpha1 and alpha2 mRNA may provide an important mechanism for determining the cellular response to THs [12].
In the present study, we have immunohistochemically investigated the existence and localization of THR (alpha1/alpha2) in rat uterus and oviduct.
II. Materials and Methods
Experimental procedure
Mated adult female Wistar rats weighing about 200–210 g each (aged 13–14 wk, n=6) were used in this study. Animals were maintained at constant temperature (21±2°C) and humidity (50±5%) on a 12 hr light/12 hr dark cycle (light on from 07.00 hr to 19.00 hr). They were housed in plastic cages (six rats per cage) and fed with standard pellet food and tap water ad libitum. Tissue samples from female rats found in estrous were collected.
Immunohistochemical procedure
Immunohistochemistry was performed on paraffin-embedded specimens. Briefly, rats were ovariohysterectomized bilaterally under rompun/ketamine (5 and 60 mg/kg, i.p.) combination anesthesia. The anterior abdominal wall was opened, and tissue samples were taken. These samples were fixed in 10% neutral formalin, dehydrated in alcohol, embedded in paraffin, and then serial sections (5 µm thickness) were collected on slides with poly-L-lysine. After rehydration, samples were transferred to 0.01 M citrate buffer (pH 6) and subsequently heated twice in a microwave oven for 5 min each at 750 W for antigen retrieval. After cooling for 20 min at room temperature, the sections were washed with phosphate buffer saline (PBS). To remove endogenous peroxidase activity, sections were kept in 3% H2O2 for 20 min and afterwards washed with PBS. Sections were then incubated in a blocking serum (Ultra V Block, Lab Vision, Fremont, CA) for 10 min in order to block non-specific binding. Sections were incubated with primary mouse-monoclonal THR (alpha1/alpha2) antibody (Lab Vision, Fremont, CA) at 1:100 dilution overnight at 4°C. Negative control sections were treated with nonimmune serum diluted in the same manner. Labeling was visualized using the Universal LSAB kit (DAKO, Carpinteria, CA) according to manufacturer’s instructions. Staining was completed with DAB Chromogen (DAKO, Carpinteria, CA) for 1–2 min, and slides were counterstained with Harris’s hematoxylin, dehydrated and then coverslipped with Permount. All specimens were examined with a Nikon E600 light microscope.
Semiquantitative evaluation
Sections were evaluated with respect to THR (alpha1/alpha2) localization in a semiquantitative manner using a light microscope and selected areas were photographed. Staining intensity was scored as negative (–), weak (+), moderate (++), strong (+++).
III. Results
The THR (alpha1/alpha2) expression observed in the rat uterus and oviduct is summarized in Table 1.
Table 1.
Semiquantitative analysis of THR (alpha1/alpha2) staining intensities in the rat uterus and oviduct
| Uterus | Oviduct | ||||||
|---|---|---|---|---|---|---|---|
| Uterus epithelium | Endometrial stromal cells | Endometrial glands | Myometrial smooth cells | Epithelium | Muscular layer | ||
| THR (alpha1/alpha2) | +++ | +++ | +++ | ++ | ++ | ++ | |
Semiquantitative scoring of immunostaining intensities: −, negative; +, weak; ++, moderate; +++, strong.
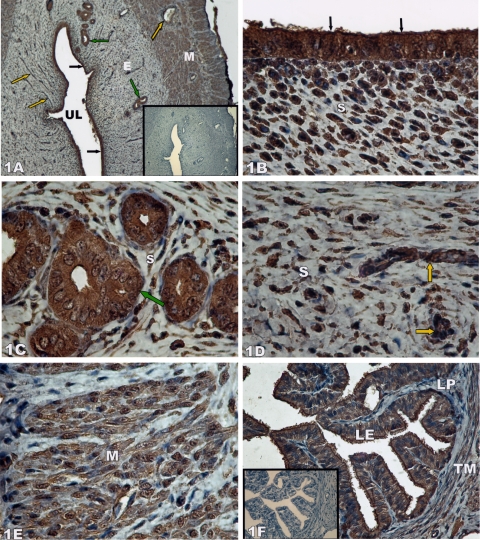
In uterus, THR (alpha1/alpha2) expression was strongly observed in uterine luminal epithelium, endometrial gland epithelium and endometrial stromal cells (Fig. 1A–D). THR (alpha1/alpha2) immunoreactivity was also observed in myometrial smooth muscle cells, but the intensity of immunostaining was moderate compared to those of the other areas (Fig. 1E).
Fig 1.
Thyroid hormone receptor (THR) (alpha1/alpha2) immunolocalization in rat uterus (A–D) and rat oviduct (F). E, endometrium; M, myometrium; UL, uterine lumen; yellow arrows, capillaries; green arrows, endometrial glandular epithelium; black arrows, uterine luminal epithelium; s, endometrial stroma; LE, lamina epithelialis of oviduct; LP, lamina propria of oviduct; TM, tunica muscularis of oviduct. Negative controls for THR (alpha1/alpha2) staining are shown as an insert. Magnifications: ×10 (A); ×100 (B–E); ×40 (F).
In oviduct, THR (alpha1/alpha2) expression was observed in the epithelium of the tube and the smooth muscle cells of muscular layer. The intensity of immunostaining was moderate in these areas. A noteworthy finding was that the basal portions of cilia in the ciliated epithelial cells, the area where the cilia originate, were strongly immunostained (Fig. 1F).
IV. Discussion
The results of the present study show that the THR (alpha1/alpha2) are expressed in the uterine luminal epithelium, gland epithelium, endometrial stromal cells, and myometrial smooth cells, as well as the epithelium and muscularis of oviduct.
The effect of THs on the uterus and fallopian tubes is controversial. Chan and Ng [7] did not observe morphological changes in the uterus and fallopian tubes when hypothyroidism was induced in rats on postnatal day one, but they reported a decrease in the number of primordial, antral and Graafian follicles. However, it has been shown that hypothyroidism decreases the absolute epithelial cell volume and the height of the luminal epithelium in rat uterus as well as a decrease in muscle layer [13, 14]. They have suggested that THs might be importantly concerned in the maintenance of the normal structure of uterine epithelial cells. It has been suggested that hypothyroidism may cause the inhibition of uterine rhythmic contractions by reducing the myometrial Ca2+ channel function in rats [25, 26]. In contrast, Wegener et al. [34] have reported that hypothyroidism does not change dihydropyridine sensitivity (i.e., the pattern of Ca2+-channel expression) in the murine uterus.
Although it is well known that the altered thyroid status disturbs reproductive function both in humans and experimental animals, the direct and indirect mechanisms of THs on the uterus have not been completely established. Most of the previous reports regarding the relationship between thyroid status and gonadal function only mention the direct effects of hypothyroidism on the pituitary-gonadal axis in female animals [2, 18, 32]. Other studies report that THs regulate insulin-like growth factor I activity in the uterus [5] and alter the uterine response to estrogens [31]. However, Kirkland et al. [17] and Evans et al. [9] have documented the existence of receptors for triiodothyronine (T3) in human and rat uterus. They have revealed a direct effect of T3 on this organ.
We have observed that THR (alpha1/alpha2) distributes in both nuclei and cytoplasm of the uterus and oviduct cells. The classical genomic actions of T3 are mediated by the THRs. THRs are members of the nuclear receptor superfamily and act as hormone inducible transcription factors [3]. They modulate transcription mainly by binding to specific DNA sites known as “thyroid hormone response elements” (TREs) [11], and many authors have reported the nuclear localization of THRs [9, 17, 22]. It has also been reported that THs accumulate in mitochondria [21], and are major regulators of mitochondrial biogenesis having a role in proliferation, differentiation and maturation [1], and regulate mitochondrial gene expression by increasing steady state mitochondrial mRNA levels, respiration, enzyme activity and protein synthesis [23, 24]. Recently, the presence of a T3 mitochondrial receptor, which has the truncated form of the T3 nuclear receptor c-ErbAα1 in the mitochondrial matrix, and which could act as a T3-dependent transcription factor, has been reported. ErbA/thyroid hormone receptor is a nuclear receptor that can affect transcription from promoters containing a TRE in a thyroid hormone (T3)-dependent manner [4, 29]. Wrutniak et al. [35] have observed two specific T3-binding proteins in the inner membrane (a 28 kDa c-ErbAα1 protein) and in the matrix (43 kDa c-ErbAα1 protein) of rat liver mitochondria, i.e., via Western blots with highly purified rat liver mitochondrial extracts and two different antisera raised against c-ErbA, immunoprecipitation of a T3-binding 43-kDa mitochondrial protein with one of these antisera, and electron microscopy. In addition, by using DNA binding analysis, they have presented evidence that this mitochondrial protein specifically binds to a natural or a synthetic T3 response element (T3RE). Among these T3-binding proteins, they also observed a 41-kDa protein obviously not related to c-ErbA nuclear receptors. They have observed by T3-PAL (T3 photoaffinity label derivative) binding that it was also detected in microsomes, plasma membrane, and lysosome preparations, thus ruling out a specific mitochondrial localization. It has been indicated in binding experiments that a 43-kDa c-ErbAα1 protein identified in the mitochondrial matrix of rat liver displays an affinity for T3 similar to that of the T3 nuclear receptor [6]. According to the results of present study, we hypothesized that the cytoplasmic localization of THR (alpha1/alpha2) in the uterus and oviduct cells would be essentially related to mitochondrial localization. The more darkly stained basal portions of cilia in the ciliated epithelial cells of the oviduct supports our hypothesis, because they have numerous small mitochondria which supply ATP for ciliary beating [16].
Recent research into steroid-receptor-related signaling identified a group of molecules termed steroid receptor cofactors. These factors bind to steroid receptors in a ligand dependent fashion, and the receptor-bound cofactors then bind to the basal transcriptional machineries of the target genes, resulting in the transcription. Thus, the steroid receptor cofactors are important molecules intervening between the receptors and target genes and are now functionally divided into two subclasses, i.e., coactivators and corepressors. The former stimulates and the latter suppresses the transcription of target genes [19, 20, 27, 30]. To examine the sex steroid-dependent growth mechanisms of the human endometrium, Shiozawa et al. [30] have examined the expression of the steroid receptor coactivators [steroid receptor coactivator-1 (SRC-1) and p300/CREB-binding protein (p300/CBP)] and corepressors [nuclear receptor corepressor (NCoR) and the silencing mediator for retinoid and thyroid hormone receptors (SMRT)] by immunohistochemistry and Western blot analysis. They have reported that SMRT expression is found only sporadically both in the nucleus and in the cytoplasm of the glandular and stromal cells in the proliferative phase of the human endometrium. Similarly, Jain et al. [15] have reported that the immunoreactivity of SMRT is localized to the nuclei of stromal compartment and the cytoplasm of focal gland and stroma in the secretory phase endometrium. In another study, SMRT were also detected by multiprobe ribonuclease protection assay and real-time reverse transcriptase polymerase chain reaction, which showed that SMRT are expressed during the menstrual cycle in both endometrium and myometrium [33]. In the present study, the localization of THRs was similar to the localization of corepressor proteins reported above.
In conclusion, the presence of thyroid hormone receptors in uterus and oviduct suggest that these organs are an active site of THs and also indicates that THs could have a direct effect on these organs.
Figure and Table
V. References
- 1.Almeida A., Orfao A., Lopez-Mediavilla C., Medina J. M. Hypothyroidism prevents postnatal changes in rat liver mitochondrial populations defined by rhodamine-123 staining. Endocrinology. 1995;136:4448–4453. doi: 10.1210/endo.136.10.7545104. [DOI] [PubMed] [Google Scholar]
- 2.Baksi S. N. Effect of propylthiouracil-induced hypothyroidism on serum levels of luteinizing hormone and follicle-stimulating hormone in the rat. J. Endocrinol. 1973;59:655–656. doi: 10.1677/joe.0.0590655. [DOI] [PubMed] [Google Scholar]
- 3.Bassett J. H. D., Harvey C. B., Williams G. R. Mechanisms of thyroid hormone receptor-specific nuclear and extra nuclear actions. Mol. Cell. Endocrinol. 2003;213:1–11. doi: 10.1016/j.mce.2003.10.033. [DOI] [PubMed] [Google Scholar]
- 4.Bigler J., Hokanson W., Eisenman R. N. Thyroid hormone receptor transcriptional activity is potentially autoregulated by truncated forms of the receptor. Mol. Cell. Biol. 1992;12:2406–2417. doi: 10.1128/mcb.12.5.2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bottazzi C., Demori I., Leone M., Fugassa E. Thyroid hormone affects rat uterine expression of IGF-1 and IGFBP-4. Boll. Soc. Ital. Biol. Sper. 1996;72:133–138. [PubMed] [Google Scholar]
- 6.Casas F., Rochard P., Rodier A., Cassar-Malek I., Marchal-Victorion S., Wiesner R. J., Cabello G., Wrutniak C. A variant form of the nuclear triiodothyronine receptor c-ErbAα1 plays a direct role in regulation of mitochondrial RNA synthesis. Mol. Cell. Biol. 1999;19:7913–7924. doi: 10.1128/mcb.19.12.7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chan W. Y., Ng T. B. Effect of hypothyroidism induced by propylthiouracil and thiourea on male and female reproductive systems of neonatal mice. J. Exp. Zool. 1995;273:160–169. doi: 10.1002/jez.1402730209. [DOI] [PubMed] [Google Scholar]
- 8.Dunn J., Peppler R., Hess M., Johnson D. C. Proestrous gonadotropin levels in thyroidectomized female rats. Experimentaria. 1976;32:1342–1344. doi: 10.1007/BF01953129. [DOI] [PubMed] [Google Scholar]
- 9.Evans R. W., Farwell A. P., Braverman L. E. Nuclear thyroid hormone receptors in the rat uterus. Endocrinology. 1983;113:1459–1463. doi: 10.1210/endo-113-4-1459. [DOI] [PubMed] [Google Scholar]
- 10.Galton V. A., Martinez E., Hernandez A., St. Germain E. A., Bates J. M., St. Germain D. L. The type 2 iodothyronine deiodinase is expressed in the rat uterus and induced during pregnancy. Endocrinology. 2001;142:2123–2128. doi: 10.1210/endo.142.5.8169. [DOI] [PubMed] [Google Scholar]
- 11.Goglia F., Moreno M., Lanni A. Action of thyroid hormones at the cellular level: the mitochondrial target. FEBS Lett. 1999;452:115–120. doi: 10.1016/s0014-5793(99)00642-0. [DOI] [PubMed] [Google Scholar]
- 12.Hastings M. L., Milcarek C., Martincic K., Peterson M. L., Munroe S. H. Expression of the thyroid hormone receptor gene, erbAa, in B lymphocytes: alternative mRNA processing is independent of differentiation but correlates with antisense RNA levels. Nucleic Acids Res. 1997;25:4296–4300. doi: 10.1093/nar/25.21.4296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inuwa I., Williams M. A. Morphometric study on the uterine horn and thyroid gland in hypothyroid, and thyroxine treated hypothyroid rats. J. Anat. 1996;188:383–393. [PMC free article] [PubMed] [Google Scholar]
- 14.Inuwa I. M., Williams M. A. A morphometric study on the endometrium of rat uterus in hypothyroid and thyroxine treated hypothyroid rats. Ups. J. Med. Sci. 2006;111:215–225. doi: 10.3109/2000-1967-042. [DOI] [PubMed] [Google Scholar]
- 15.Jain J. K., Li A., Yang W., Minoo P., Felix J. C. Mifepristone alters expression of endometrial steroid receptors and their cofactors in new users of medroxyprogesterone acetate. Fertil. Steril. 2007;87:8–23. doi: 10.1016/j.fertnstert.2006.05.076. [DOI] [PubMed] [Google Scholar]
- 16.Junqueira L. C., Carneiro J. Basic Histology: Text & Atlas, 10th ed. McGraw-Hill Companies; London: 2003. [Google Scholar]
- 17.Kirkland J. L., Mukku V., Hardy M., Young R. Evidence for triiodothyronine receptors in human endometrium and myometrium. Am. J. Obstet. Gynecol. 1983;146:380–383. doi: 10.1016/0002-9378(83)90817-7. [DOI] [PubMed] [Google Scholar]
- 18.Mattheij J. A. M., Swarts J. J. M., Lokerse P., van Kampen J. T., van der Heide D. Effect of hypothyroidism on the pituitary-gonadal axis in the adult female rat. J. Endocrinol. 1995;146:87–94. doi: 10.1677/joe.0.1460087. [DOI] [PubMed] [Google Scholar]
- 19.McKenna N. J., Lanz R. B., O’Malley B. W. Nuclear receptor coregulators: cellular and molecular biology. Endocr. Rev. 1999;20:321–344. doi: 10.1210/edrv.20.3.0366. [DOI] [PubMed] [Google Scholar]
- 20.McKenna N. J., O’Malley B. W. From ligand to response: generating diversity in nuclear receptor coregulator function. J. Steroid Biochem. Mol. Biol. 2000;74:351–356. doi: 10.1016/s0960-0760(00)00112-6. [DOI] [PubMed] [Google Scholar]
- 21.Morel G., Ricard-Blum S., Ardail D. Kinetics of internalization and subcellular binding sites for T3 in mouse liver. Biol. Cell. 1996; 86:167–174. doi: 10.1016/0248-4900(96)84781-2. [DOI] [PubMed] [Google Scholar]
- 22.Mukku V. R., Kirkland J. L., Hardy M., Stancel G. M. Evidence for thyroid hormone receptors in uterine nuclei. Metabolism. 1983;32:142–145. doi: 10.1016/0026-0495(83)90219-6. [DOI] [PubMed] [Google Scholar]
- 23.Mutvei A., Husman B., Andersson G., Nelson B. D. Thyroid hormone and not growth hormone is the principle regulator of mammalian mitochondrial biogenesis. Acta Endocrinol. 1989;121:223–228. doi: 10.1530/acta.0.1210223. [DOI] [PubMed] [Google Scholar]
- 24.Mutvei A., Kuzela S., Nelson B. D. Control of mitochondrial transcription by thyroid hormone. Eur. J. Biochem. 1989;180:235–240. doi: 10.1111/j.1432-1033.1989.tb14638.x. [DOI] [PubMed] [Google Scholar]
- 25.Parija S. C., Mishra S. K., Raviprakash V. Hypothyroid state reduces calcium channel function in 18-day pregnant rat uterus. Indian. J. Exp. Biol. 2006;44:19–27. [PubMed] [Google Scholar]
- 26.Parija S. C., Raviprakash V., Telang A. G., Varhsney V. P., Mishra S. K. Influence of hypothyroid state on 45Ca(2+) influx and sensitivity of rat uterus to nifedipine and diltiazem. Eur. J. Pharmacol. 2001;421:207–213. doi: 10.1016/s0014-2999(01)01023-8. [DOI] [PubMed] [Google Scholar]
- 27.Rachez C., Freedman L. P. Mediator complexes and transcription. Curr. Opin. Cell. Biol. 2001;13:274–280. doi: 10.1016/s0955-0674(00)00209-x. [DOI] [PubMed] [Google Scholar]
- 28.Ruiz M., Diego A. M., Reyes A., Alonso A., Morell M. Influence of thyroidectomy on serum and pituitary FSH in control and orchidectomized rats. Res. Exp. Med. 1989;189:85–90. doi: 10.1007/BF01851258. [DOI] [PubMed] [Google Scholar]
- 29.Sap J., Munoz A., Damm K., Goldberg Y., Ghysdael J., Leutz A., Beug H., Vennstrom B. The c-erb-A protein is a high-affinity receptor for thyroid hormone. Nature. 1986;324:635–640. doi: 10.1038/324635a0. [DOI] [PubMed] [Google Scholar]
- 30.Shiozawa T., Shih H. C., Miyamoto T., Feng Y. Z., Uchikawa J., Itoh K., Konishi I. Cyclic changes in the expression of steroid receptor coactivators and corepressors in the normal human endometrium. J. Clin. Endocrinol. Metab. 2003;88:871–878. doi: 10.1210/jc.2002-020946. [DOI] [PubMed] [Google Scholar]
- 31.Steinsapir J., Rojasi A. M., Mena M., Techernitchin A. N. Effects of thyroid hormones on some uterine responses to estrogens. Endocrinology. 1982;110:1773–1779. doi: 10.1210/endo-110-5-1773. [DOI] [PubMed] [Google Scholar]
- 32.Tohei A., Imai A., Watanabe G., Taya K. Influence of thiouracil-induced hypothyroidism on adrenal and gonadal functions in adult female rats. J. Vet. Med. Sci. 1998;60:439–446. doi: 10.1292/jvms.60.439. [DOI] [PubMed] [Google Scholar]
- 33.Vienonen A., Miettinen S., Blauer M., Martikainen P. M., Tomas E., Heinonen P. K., Ylikomi T. Expression of nuclear receptors and cofactors in human endometrium and myometrium. J. Soc. Gynecol. Investig. 2004;11:104–112. doi: 10.1016/j.jsgi.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 34.Wegener J. W., Lee M., Hofmann F. Hypothyroidism does not affect the dihydropyridine sensitivity of precontracted murine uterus. Can. J. Physiol. Pharmacol. 2003;81:890–893. doi: 10.1139/y03-090. [DOI] [PubMed] [Google Scholar]
- 35.Wrutniak C., Cassar-Malek I., Marchal S., Rascle A., Heusser S., Keller J. M., Fléchon J., Dauça M., Samarut J., Ghysdael J., Cabello G. A 43-kDa protein related to c-Erb A alpha 1 is located in the mitochondrial matrix of rat liver. J. Biol. Chem. 1995;270:16347–16354. doi: 10.1074/jbc.270.27.16347. [DOI] [PubMed] [Google Scholar]