Abstract
Background
Survival of scleroderma has changed since the renal crisis treatment has become possible.
Aims
To document the changes in survival and organ system causes of mortality in systemic sclerosis (SSc) over the past 25 years in patients from a single medical centre.
Methods
Consecutive patients evaluated at the University of Pittsburgh, Pittsburgh, Pennsylvania, USA between 1 January 1972 and 31 December 1996 were studied. Survival was determined in five 5‐year time periods between 1972 and 1997. Causes of death included scleroderma‐related (scleroderma renal crisis, pulmonary arterial hypertension, pulmonary fibrosis (PF), gastrointestinal (GI), heart and multiorgan failure) and non‐scleroderma‐related (cancer, atherosclerotic cardiovascular or cerebrovascular disease, infection, sudden death, other and unknown) causes.
Results
The 10‐year survival improved steadily from 54% to 66% during each of the time intervals. There was a significant improvement in survival for patients during 1982–91 compared with those during 1972–81 (p<0.001), even when patients with renal crisis were excluded (p<0.005). The frequency of deaths due to renal crisis significantly decreased over the 30‐year time period, from 42% to 6% of scleroderma‐related deaths (p<0.001), whereas the proportion of patients with scleroderma who died of PF increased from 6% to 33% (p<0.001). The frequency of pulmonary hypertension, independent of PF, also significantly increased during this time period (p<0.05). There were no changes in scleroderma GI‐ and heart‐related deaths, nor in any of the non‐scleroderma‐related causes, although patients with scleroderma were less likely to die from scleroderma‐related problems in the past 15 years.
Conclusion
The change in the pattern of scleroderma‐related deaths over the past 30 years demonstrates that the lung (both pulmonary hypertension and PF) is the primary cause of scleroderma‐related deaths today. It is important that aggressive searches continue to develop better therapies for these severe pulmonary complications of SSc.
Systemic sclerosis (SSc) is a multisystem disease that is often fatal. Since 1980, the successful treatment of scleroderma renal crisis (SRC) has dramatically decreased mortality from SSc. Most scleroderma experts believe that, currently, the most frequent cause of death is pulmonary involvement, either interstitial lung disease or pulmonary arterial hypertension (PAH). The purpose of this study is to document the changes in organ system causes of mortality in SSc over the past 25 years in patients from a single medical centre.
Patients and methods
The Pittsburgh Scleroderma Databank is a prospective natural history study of consecutive patients with SSc first evaluated at the University of Pittsburgh, Pittsburgh, Pennsylvania, USA, since 1 January 1972. Patient outcomes, including severe organ system involvement and survival, were determined for all patients at follow‐up visits, every 1–2 years, using a standard patient‐completed questionnaire or by a telephone interview. Patients who had not been seen or did not respond to the questionnaire were traced by contacting their referring physician or next of kin. Dates of death were confirmed through the Social Security Death Index. We have previously validated our methods of obtaining accurate assessment of severe internal organ involvement and the cause of death.1
Survival
We determined changes in overall survival in five 5‐year time periods between 1972 and 1997. We included only patients who were first evaluated during each of those time periods, and then determined the 10‐year survival from the time that the patient was first diagnosed with SSc. Survival information was available for 93% of the patients as of 31 December 2001, and thus the survival of the 1992–6 groups was limited to 5 years.
Causes of death
We determined the cause of death for each deceased patient. Each death was classified as to whether it was primarily related to scleroderma or not. The scleroderma‐related death causes resulted from severe organ involvement.1 These are:
SRC—deaths during SRC itself or related to dialysis or renal transplantation.
PAH—as defined by a right heart catheterisation with a mean pulmonary artery pressure >25 mm Hg, or by an echocardiogram with a systolic pulmonary artery pressure >50 mm Hg, which was not associated with severe, hypoxic pulmonary fibrosis (PF)—that is, vasculopathic pulmonary hypertension.
PF—advanced PF (determined by radiograph, physiology from pulmonary function tests or hypoxaemia requiring oxygen supplementation).
Gastrointestinal (GI)—severe involvement of the oesophagus or small bowel, resulting in malabsorption, malnutrition or hyperalimentation.
Heart—primary cardiomyopathy, as shown by clinical signs of heart failure and an ejection fraction <50% (not associated with renal crisis or PAH), arrhythmias or conduction defects (not attributable to other cardiac conditions) requiring treatment.
Multiorgan failure—severe simultaneous damage from >1 scleroderma‐related organ involvement, in which it was difficult to determine the primary organ that was the cause of death. Also included in this category were rare causes that did not fit into any of the above classifications—that is, sepsis from calcinosis, acute hepatic necrosis, etc. This classification was first added in 1980.
Patients with non‐scleroderma‐related deaths usually had some scleroderma internal organ compromise which would have contributed to the death but was not felt to play a primary role. In cases where it was difficult to determine what the primary cause of death was, the severity of the scleroderma‐related organ involvement was reviewed. For example, in a patient with malabsorption due to small bowel involvement who died of intravenous catheter‐associated septicaemia, GI was considered the cause of death. On the other hand, in a patient with PF who died of sepsis from pyelonephritis, the cause of death was considered to be infection. The non‐scleroderma‐related death categories included:
Cancer—patients who died of cancer, even though they had severe organ involvement.
Atherosclerotic cardiovascular or cerebrovascular disease—patients who died of myocardial infarction or a stroke, or of complications from chronic non‐scleroderma artherosclerotic heart disease.
Infection—not directly related to scleroderma organ involvement.
Sudden death—a sudden death without prior scleroderma heart disease and without other obvious aetiology (This included unwitnessed deaths, accidents and suicides).
Other—a variety of common causes of death, including chronic disease unrelated to scleroderma in older people, such as diabetes, other causes of lung (eg, emphysema), heart or kidney (eg, essential hypertension) disease (These patients did not have any evidence of severe scleroderma involvement).
Unknown—in some cases, a specific cause of death could not be determined, or information was pending.
Deaths were grouped into 5‐year time periods between 1972 and 2001 in which the death occurred. Statistical comparisons were performed across time periods adjusted for disease duration at the start of the time period.
Data analysis
The Pittsburgh Scleroderma Databank uses Medlog for data management. Data analysis included descriptive statistics, means, χ2, Pearson's correlations, Kaplan–Meier survival analysis, analysis of variance and Cox proportional modelling to adjust for disease duration between the groups over time.
Results
Survival
Table 1 shows the demographic characteristics of the patients seen in the five different time periods. There were no major differences across these time periods for any of the features. Fewer men were seen during 1982–6 (p<0.05). The earliest time period had a higher proportion of patients with SSc with limited cutaneous involvement (p<0.05), which accounts for the longer disease duration at the time of the initial evaluation at the University of Pittsburgh. Patients first seen during the final time period, 1992–6, had a shorter follow‐up because of the 31 December 2001 cut‐off time, and thus their disease duration at the last study visit was lower, and only their 5‐year cumulative survival rate is reported.
Table 1 Demographic findings according to the time period of first evaluation.
| 1972–6 | 1977–81 | 1982–6 | 1987–91 | 1992–6 | |
|---|---|---|---|---|---|
| n | 221 | 323 | 392 | 534 | 655 |
| Female sex (%) | 79 | 80 | 84* | 79 | 81 |
| Age (at first diagnosis by a doctor; years) | 40 | 43 | 42 | 40 | 42 |
| SSc subtype | |||||
| Diffuse SSc (%) | 40* | 47 | 49 | 44 | 47 |
| Disease duration* (years) | |||||
| At first diagnosis by a doctor | 2.1 | 2.5 | 2.3 | 2.7 | 2.4 |
| At first visit | 8.4* | 6.7 | 7.0 | 7.3 | 6.9 |
| At last study visit | 15.1 | 14.7 | 14.7 | 14.2 | 11.1** |
SSc, systemic sclerosis.
*p<0.05, **p<0.01.
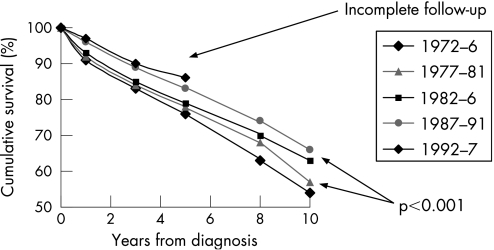
The 10‐year survival improved steadily during each of the time intervals (fig 1). The 5‐year survival in the most recent patients continued to show improvement compared with the 5‐year survival in previous patients. The 10‐year survival ranged from 54% to 66%, with an increase of approximately 3–4% during each consecutive period. However, after ACE inhibitors became available in the early 1980s, the 10‐year survival improved by 6%, from 57% to 63%. The survival across the entire 25‐year time period did not change significantly. However, there was a significant improvement in survival for patients during 1982–91 compared with those during the 1972–81 (p<0.001). Even excluding deaths due to renal crisis, there was still a significant improvement in survival for the period 1987–91 compared with 1972–6 (p<0.005).
Figure 1 Survival of patients with systemic sclerosis between 1972 and 2002.
Causes of death
We compared the primary causes of death for patients seen throughout the 30‐year time period using the time period of the death rather than the time period of the initial evaluation as in the survival analysis. Consequently, each of the time periods included all patients who were alive at some point during that time period. We then used a Cox proportional modelling analysis to evaluate the causes of death across the different time periods, adjusting for disease duration. Table 2 shows the demographic features of patients who were seen during those time periods. As expected, there were increasing numbers of patients over time, since patient accrual was cumulative. The age and disease duration from the time of presentation of the first symptom attributable to scleroderma were calculated at the time of the first contact with the patient during this time period for all patients, whether it was a clinic, hospitalisation visit, mail or outside information. The most recent time period (1997–2001) included patients who had been followed up for the longest period of time, and did not include a group of newly evaluated patients who had early disease, as those patients had the longest disease duration. The age, sex, frequency of diffuse scleroderma and frequency of death were similar in the middle four time groups. Race was similar over time, with African‐Americans averaging only 6% of all patients. The disease duration differed between the time groups, but the analysis was adjusted for this difference. About 20% of patients followed up during each time period died, with the exception of the most recent group (24%), who were older and had longer disease duration. Although the proportion of deaths was similar in all time periods, the proportion of scleroderma‐related deaths decreased significantly, from 70% in the first time period to only 50% in the last time period (p<0.001).
Table 2 Demographic features of patients who were followed up during each of six 5‐year time periods.
| 1972–6 | 1977–81 | 1982–6 | 1987–91 | 1992–6 | 1997–2001 | |
|---|---|---|---|---|---|---|
| At risk (n) | 221 | 493 | 768 | 1153 | 1460 | 1508 |
| Female sex (%) | 79 | 80 | 82 | 82 | 81 | 83 |
| Age (at onset of time period; years) | 48* | 50 | 51 | 51 | 52 | 55† |
| Disease duration at the beginning of the interval (years) | 8.4 | 8.4 | 9.2 | 10.6 | 11.2 | 13.9† |
| SSc subtype | ||||||
| Diffuse SSc (%) | 41 | 46 | 49 | 47 | 48 | 44 |
| Deaths | ||||||
| All deaths, n (%) | 42 (19) | 105 (21) | 148 (19) | 211 (18) | 289 (20) | 314 (24) |
| Deaths due to SSc (% of all deaths) | 70 | 68 | 58 | 53 | 57 | 50 |
SSc, systemic sclerosis.
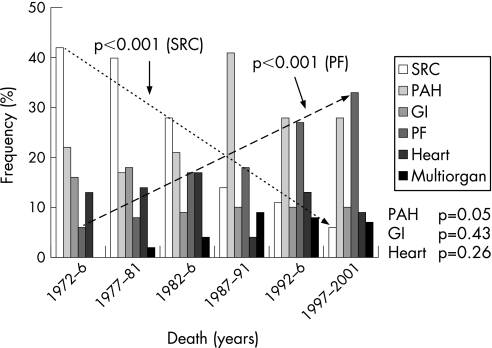
We examined the scleroderma‐related deaths in greater detail (fig 2). The frequency of deaths due to renal crisis decreased significantly over the 30‐year time period, from 42% to 6% of scleroderma‐related deaths and from 31% to 3% of all deaths (the data on the frequency of scleroderma‐related deaths within all deaths is not shown; for both, p<0.001). By contrast, the proportion of patients with scleroderma who died of PF increased from 6% to 33% of scleroderma‐related deaths, and from 5% to 16% of all deaths (for both, p<0.001). Hazard ratio over time was 1.33, and there was no interaction with disease duration. The frequency of deaths due to pulmonary hypertension, independent of PF, also significantly increased during this time period (p<0.05). In all, 60% of scleroderma‐related deaths are now from both of these lung complications combined, clearly establishing this as the most important scleroderma problem. The frequency of deaths due to scleroderma GI and heart diseases did not change significantly over this time period. There was a non‐significant decrease in the frequency of these causes among all deaths throughout this time. Deaths due to GI disease decreased from 12% of all deaths to 4%, and those due to scleroderma heart disease decreased from 10% to 5% (data not shown).
Figure 2 Changes in causes of systemic sclerosis‐related deaths between 1972 and 2001. GI, gastrointestinal; PAH, pulmonary arterial hypertension; PF, pulmonary fibrosis; SRC, scleroderma renal crisis.
As mentioned above, currently 50% of patients with SSc die of non‐scleroderma‐related causes, increased by 30% from that in earlier time periods (table 3). However, there were no changes in the distribution of the non‐SSc‐associated major causes of death, such as cancer, atherosclerotic cardiovascular disease or infection.
Table 3 Non‐scleroderma‐related causes of deaths over time.
| 1972–6 | 1977–81 | 1982–6 | 1987–91 | 1992–6 | 1997–2001 | |
|---|---|---|---|---|---|---|
| At risk (n) | 221 | 493 | 768 | 1153 | 1460 | 1508 |
| All deaths | 42 | 105 | 148 | 211 | 289 | 364 |
| Causes (% of all deaths) | ||||||
| Cancer | 10 | 10 | 10 | 15 | 11 | 7 |
| ASCVD | 3 | 4 | 8 | 7 | 6 | 2 |
| Infection | 2 | 3 | 6 | 7 | 9 | 5 |
| Other | 7 | 8 | 12 | 10 | 10 | 1 |
| Unknown | 9 | 7 | 6 | 7 | 8 | 10 |
| Pending | 0 | 0 | 0 | 1 | 1 | 13 |
ASCVD, atherosclerotic cardiovascular disease.
Discussion
Survival studies in scleroderma show diverse results, depending on the patient demographics, clinical subsets and organ system involvement, and are thus difficult to compare. Differences in the proportion of patients with limited and diffuse SSc, and in the frequency of serum autoantibodies, such as anticentromere antibodies and antiscleroderma 70 antibody, in different ethnic populations and countries are reasons why comparisons from one country to another are not easily interpreted. Differences observed in the starting time periods, such as the first symptom, first physician diagnosis or first study centre visit, have been used. Consequently, SSc survival studies from Canada, Hungary, Spain, England, Japan, Denmark, Sweden, Australia, Italy and Greece show a wide variation in outcomes.2,3,4,5,6,7
Our study compares the survival of patients with scleroderma seen at the same institution by the same investigators over a 30‐year time period. All patients were evaluated and were followed up in a similar fashion, making it possible to compare time periods. As of 2001, we had a 93% accountability of the patients first seen between 1972 and 1996. The 10‐year cumulative survival improved significantly from 53% in the 1970s to 67% in the 1990s. Although some of this difference is related to the improved outcome of renal crisis, the significant improvement still remained even when all patients with renal crisis throughout the time period studied were excluded. As the proportion of patients with diffuse scleroderma increased over time, it might be expected that survival would decrease. Instead, survival improved in both patients with limited and those with diffuse SSc. There was no difference in the disease duration at the time of the first physician diagnosis of SSc in these five time periods, which could be contributing to improved survival. It seems likely that improved physician management of patients with scleroderma, and earlier, more intensive treatment of scleroderma organ involvement has resulted in improved survival. Patients dying of scleroderma‐related causes died at an earlier age than (51 years, before 1986) than those dying of non‐scleroderma‐related causes (58 years, after 1986; p<0.001). This gives them a greater chance of dying from non‐scleroderma‐related causes.
Ferri et al's study had similar findings in their long‐term outcome of 1012 Italian patients with scleroderma.4 These patients' 10‐year survival from the time of diagnosis was 60.6% before 1985, which improved to 76.8% in more recent years. Although our survival figures, at 52% in the earliest time period, improving to 68% in the most recent time period, are not quite as good as those in the Italian population, both studies show the same significant improvement in outcome over time. Our population had more men and more patients with diffuse cutaneous scleroderma than the Italian patients, which probably accounts for the survival difference between these two large studies.
Previous studies have focused on risk factors for poor survival that included older age, male sex, poor socioeconomic status, scleroderma subtype and specific organ involvement. Other factors such as erythrocyte sedimentation rate and anaemia have also been shown to affect survival.3,8,9 Not surprisingly, the presence of any major organ involvement is associated with decreased survival.8,10 A recent study showed that severity of disease also predicted early death.11 In patients with severe skin (modified Rodnan skin score >40), lung (vital capacity <55% predicted), GI (malabsorption, pseudo‐obstruction), heart (severe arrhythmia or congestive heart failure) or kidney involvement (renal crisis), the 9‐year cumulative survival was 38%, whereas, in patients who had mild organ involvement, the 9‐year cumulative survival was 78%.
The most significant change in survival over time occurred in those patients with SRC. Earlier diagnosis and aggressive use of ACE inhibitors can prevent or even reverse renal failure, with more than half of the cases pertaining to dialysis.12,13 The 5‐year cumulative survival for patients with SRC increased from <10% before the use of ACE inhibitors to 65% after the use of these drugs.13 During the past 10 years, patients with a good outcome from renal crisis had a 5‐year cumulative survival equivalent to that of patients with diffuse cutaneous SSc who did not have renal crisis, approximately 90% of potential. Some people question whether there is also an actual decrease in the frequency of deaths due to renal crisis because of the increased use of ACE inhibitors. However, we have not used ACE inhibitors prophylactically, and have previously demonstrated the dramatic improvement in survival in our patients.13 Patients who survive the initial renal crisis do not contribute to the increased deaths from PF. Most survivors of renal crisis who died later succumbed to non‐scleroderma‐related illnesses. Only 3% of patients who have survived SRC died of PF, and 5% died of pulmonary hypertension. This result should not be surprising, as the most common antibody found in patients with renal crisis is anti‐RNA polymerase III, an autoantibody that is associated with a low frequency of severe PF.14,15
PAH was the second most frequent cause of scleroderma‐related deaths in the 1970s. It has continued to be a leading cause of death, with close to 30% of scleroderma‐related deaths being due to PAH. There is no apparent explanation for the increase in causes of death due to PAH during the 1987–91 time period. There was no change in the frequency of direct new PAH referrals during this time. Around that time, we became more aware that PAH occurred in patients with diffuse scleroderma independent of PF. However, 11% of the patients who died of PAH in the time periods before and after that time period had diffuse SSc. The slight increase in deaths due to PAH over the 25 years is likely to be the result of our more aggressive search for this complication since treatment had become available. Over the past 5 years, there has been a significant improvement in the pharmacological treatment of pulmonary hypertension.16,17 Recent studies suggest that there has been improvement in short‐term survival in patients with PAH‐SSc treated with these new drugs,18 but it is too soon to conclude that there will be improvement in the long‐term survival.
The proportion of deaths due to PF has increased from 5% of scleroderma‐related deaths in the 1970s to >30% of scleroderma‐related deaths in the 1990s. Even considering the overall decrease in scleroderma‐related deaths over time, deaths due to PF were found to be increased from 3% of all deaths in the 1970s to 18% of all deaths in the 1990s (p<0.001). This is not related to the differences in disease duration in patients seen during these time periods. It is possible that patients who would have died of other SSc‐related causes in the 1970s are now living longer. These additional years, along with slow progression of fibrosis, ageing or infection, are likely to contribute to the increase in deaths due to PF. We considered other possible explanations, such as an increased frequency of anti‐topoisomerase I antibodies or referral bias of patients with severe interstitial lung disease, but did not find these to be important factors.
The survival of patients with scleroderma has improved over the past 30 years. Although the global mortality has not changed, fewer scleroderma‐related deaths are being reported, with patients living longer despite having the disease. The change in the distribution of scleroderma‐related deaths over the past 30 years confirms that lung disease (both pulmonary hypertension and PF) is the primary cause of scleroderma‐related deaths today. It is important that aggressive searches continue to develop better therapies for these severe pulmonary complications of SSc.
Acknowledgements
We thank Ms Mary Lucas, RN, MPH, for her long‐term assistance in data management.
Abbreviations
GI - gastrointestinal
PAH - pulmonary arterial hypertension
PF - pulmonary fibrosis
SRC - scleroderma renal crisis
SSc - systemic sclerosis
Footnotes
Funding: This study was funded partly by a grant from the Scleroderma Foundation, Danvers, Massachusetts, USA.
Competing interests: None declared.
References
- 1.Steen V D, Medsger T A., Jr Severe organ involvement in systemic sclerosis with diffuse scleroderma. Arthritis Rheum 2000432437–2444. [DOI] [PubMed] [Google Scholar]
- 2.Bond C, Pile K D, McNeil J D, Ahern M J, Smith M D, Cleland L G.et al South Australian Scleroderma Register: analysis of deceased patients. Pathology 199830386–390. [DOI] [PubMed] [Google Scholar]
- 3.Bryan C, Knight C, Black C M, Silman A J. Prediction of five‐year survival following presentation with scleroderma: development of a simple model using three disease factors at first visit. Arthritis Rheum 1999422660–2665. [DOI] [PubMed] [Google Scholar]
- 4.Ferri C, Valentini G, Cozzi F, Sebastiani M, Michelassi C, La Montagna G.et al Systemic sclerosis: demographic, clinical, and serologic features and survival in 1,012 Italian patients. Medicine (Baltimore) 200281139–153. [DOI] [PubMed] [Google Scholar]
- 5.Ioannidis J P, Vlachoyiannopoulos P G, Haidich A B, Medsger T A, Jr, Lucas M, Michet C J.et al Mortality in systemic sclerosis: an international meta‐analysis of individual patient data. Am J Med 20051182–10. [DOI] [PubMed] [Google Scholar]
- 6.Jacobsen S, Halberg P, Ullman S. Mortality and causes of death of 344 Danish patients with systemic sclerosis (scleroderma). Br J Rheumatol 199837750–755. [DOI] [PubMed] [Google Scholar]
- 7.Kuwana M, Kaburaki J, Arnett F C, Howard R F, Medsger T A, Jr, Wright T M. Influence of ethnic background on clinical and serologic features in patients with systemic sclerosis and anti‐DNA topoisomerase I antibody. Arthritis Rheum 199942465–474. [DOI] [PubMed] [Google Scholar]
- 8.Altman R D, Medsger T A, Jr, Bloch D A, Michel B A. Predictors of survival in systemic sclerosis (scleroderma). Arthritis Rheum 199134403–413. [DOI] [PubMed] [Google Scholar]
- 9.Bulpitt K J, Clements P J, Lachenbruch P A, Paulus H E, Peter J B, Agopian M S.et al Early undifferentiated connective tissue disease: III. Outcome and prognostic indicators in early scleroderma (systemic sclerosis). Ann Intern Med 1993118602–609. [DOI] [PubMed] [Google Scholar]
- 10.Medsger T A, Jr, Masi A T, Rodnan G P, Benedek T G, Robinson H. Survival with systemic sclerosis (scleroderma). A life‐table analysis of clinical and demographic factors in 309 patients. Ann Intern Med 197175369–376. [DOI] [PubMed] [Google Scholar]
- 11.Steen VD M T J. Severe organ involvement in systemic sclerosis with diffuse scleroderma. Arthritis Rheum 2000432437–2444. [DOI] [PubMed] [Google Scholar]
- 12.Steen V D, Costantino J P, Shapiro A P, Medsger T A., Jr Outcome of renal crisis in systemic sclerosis: relation to availability of angiotensin converting enzyme (ACE) inhibitors [see comments]. Ann Intern Med 1990113352–357. [DOI] [PubMed] [Google Scholar]
- 13.Steen V D, Medsger T A., Jr Long‐term outcomes of scleroderma renal crisis. Ann Intern Med 2000133600–603. [DOI] [PubMed] [Google Scholar]
- 14.Steen V D. Autoantibodies in systemic sclerosis. Semin Arthritis Rheum 20053535–42. [DOI] [PubMed] [Google Scholar]
- 15.Okano Y, Steen V D, Medsger T A., Jr Autoantibody reactive with RNA polymerase III in systemic sclerosis. Ann Intern Med 19931191005–1013. [DOI] [PubMed] [Google Scholar]
- 16.McLaughlin V V, McGoon M D. Pulmonary arterial hypertension. Circulation 20061141417–1431. [DOI] [PubMed] [Google Scholar]
- 17.Robertson L, Pignone A, Kowal‐Bielecka O, Fiori G, Denton C P, Matucci‐Cerinic M. Pulmonary arterial hypertension in systemic sclerosis: diagnostic pathway and therapeutic approach. Ann Rheum Dis 200564804–807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Williams M H, Das C, Handler C E, Akram M R, Davar J, Denton C P.et al Systemic sclerosis associated pulmonary hypertension: improved survival in the current era. Heart 200692926–932. [DOI] [PMC free article] [PubMed] [Google Scholar]