Abstract
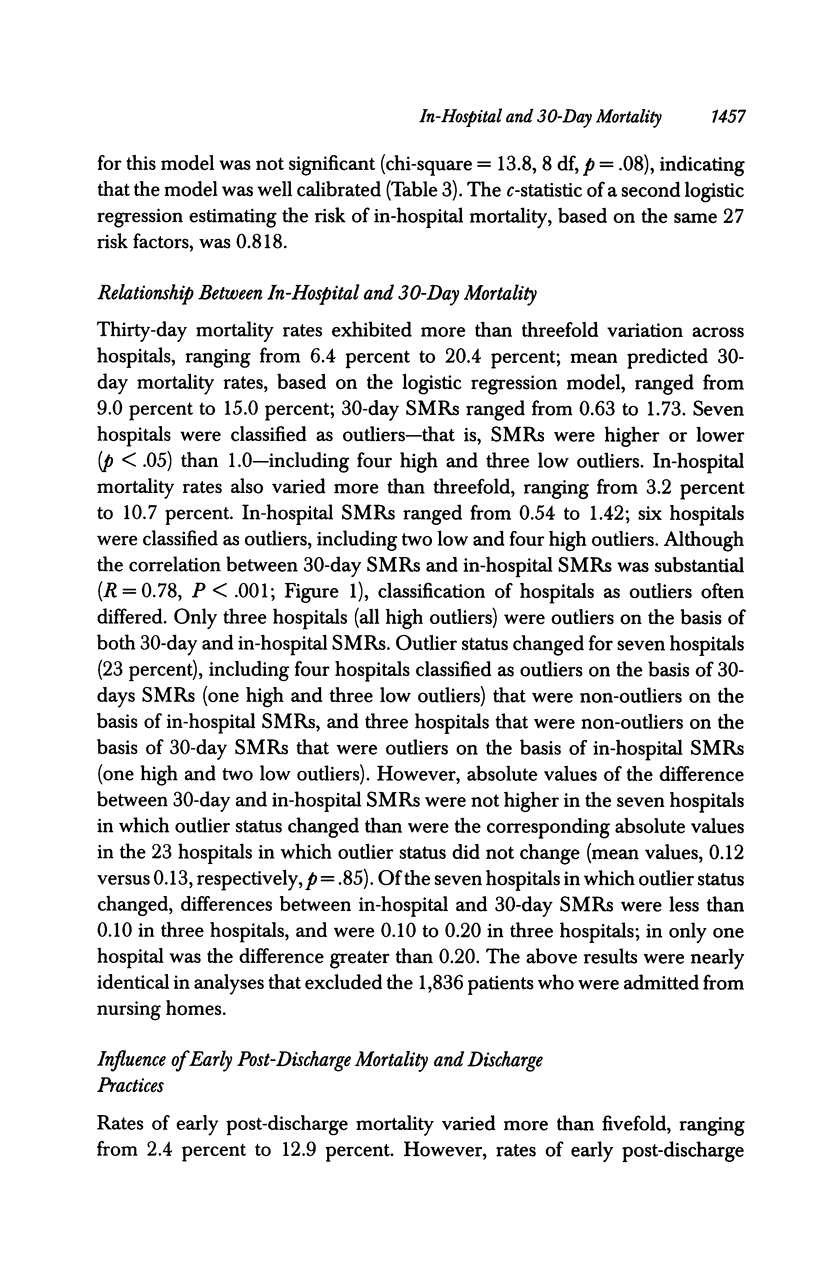
OBJECTIVE: To examine the relationship of in-hospital and 30-day mortality rates and the association between in-hospital mortality and hospital discharge practices. DATA SOURCES/STUDY SETTING: A secondary analysis of data for 13,834 patients with congestive heart failure who were admitted to 30 hospitals in northeast Ohio in 1992-1994. DESIGN: A retrospective cohort study was conducted. DATA COLLECTION: Demographic and clinical data were collected from patients' medical records and were used to develop multivariable models that estimated the risk of in-hospital and 30-day (post-admission) mortality. Standardized mortality ratios (SMRs) for in-hospital and 30-day mortality were determined by dividing observed death rates by predicted death rates. PRINCIPAL FINDINGS: In-hospital SMRs ranged from 0.54 to 1.42, and six hospitals were classified as statistical outliers (p <.05); 30-day SMRs ranged from 0.63 to 1.73, and seven hospitals were outliers. Although the correlation between in-hospital SMRs and 30-day SMRs was substantial (R = 0.78, p < .001), outlier status changed for seven of the 30 hospitals. Nonetheless, changes in outlier status reflected relatively small differences between in-hospital and 30-day SMRs. Rates of discharge to nursing homes or other inpatient facilities varied from 5.4 percent to 34.2 percent across hospitals. However, relationships between discharge rates to such facilities and in-hospital SMRs (R = 0.08; p = .65) and early post-discharge mortality rates (R = 0.23; p = .21) were not significant. CONCLUSIONS: SMRs based on in-hospital and 30-day mortality were relatively similar, although classification of hospitals as statistical outliers often differed. However, there was no evidence that in-hospital SMRs were biased by differences in post-discharge mortality or discharge practices.
Full text
PDF









Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Chassin M. R., Park R. E., Lohr K. N., Keesey J., Brook R. H. Differences among hospitals in Medicare patient mortality. Health Serv Res. 1989 Apr;24(1):1–31. [PMC free article] [PubMed] [Google Scholar]
- Garnick D. W., DeLong E. R., Luft H. S. Measuring hospital mortality rates: are 30-day data enough? Ischemic Heart Disease Patient Outcomes Research Team. Health Serv Res. 1995 Feb;29(6):679–695. [PMC free article] [PubMed] [Google Scholar]
- Gostin L. O., Lazzarini Z., Neslund V. S., Osterholm M. T. The public health information infrastructure. A national review of the law on health information privacy. JAMA. 1996 Jun 26;275(24):1921–1927. [PubMed] [Google Scholar]
- Green J., Wintfeld N., Sharkey P., Passman L. J. The importance of severity of illness in assessing hospital mortality. JAMA. 1990 Jan 12;263(2):241–246. [PubMed] [Google Scholar]
- Grover F. L., Johnson R. R., Marshall G., Hammermeister K. E. Factors predictive of operative mortality among coronary artery bypass subsets. Ann Thorac Surg. 1993 Dec;56(6):1296–1307. doi: 10.1016/0003-4975(93)90670-d. [DOI] [PubMed] [Google Scholar]
- Hannan E. L., Kilburn H., Jr, O'Donnell J. F., Lukacik G., Shields E. P. Adult open heart surgery in New York State. An analysis of risk factors and hospital mortality rates. JAMA. 1990 Dec 5;264(21):2768–2774. [PubMed] [Google Scholar]
- Jencks S. F., Williams D. K., Kay T. L. Assessing hospital-associated deaths from discharge data. The role of length of stay and comorbidities. JAMA. 1988 Oct 21;260(15):2240–2246. [PubMed] [Google Scholar]
- Kahn K. L., Brook R. H., Draper D., Keeler E. B., Rubenstein L. V., Rogers W. H., Kosecoff J. Interpreting hospital mortality data. How can we proceed? JAMA. 1988 Dec 23;260(24):3625–3628. [PubMed] [Google Scholar]
- Kahn K. L., Keeler E. B., Sherwood M. J., Rogers W. H., Draper D., Bentow S. S., Reinisch E. J., Rubenstein L. V., Kosecoff J., Brook R. H. Comparing outcomes of care before and after implementation of the DRG-based prospective payment system. JAMA. 1990 Oct 17;264(15):1984–1988. [PubMed] [Google Scholar]
- Knaus W. A., Wagner D. P., Zimmerman J. E., Draper E. A. Variations in mortality and length of stay in intensive care units. Ann Intern Med. 1993 May 15;118(10):753–761. doi: 10.7326/0003-4819-118-10-199305150-00001. [DOI] [PubMed] [Google Scholar]
- Park R. E., Brook R. H., Kosecoff J., Keesey J., Rubenstein L., Keeler E., Kahn K. L., Rogers W. H., Chassin M. R. Explaining variations in hospital death rates. Randomness, severity of illness, quality of care. JAMA. 1990 Jul 25;264(4):484–490. [PubMed] [Google Scholar]
- Rosenthal G. E., Harper D. L. Cleveland health quality choice: a model for collaborative community-based outcomes assessment. Jt Comm J Qual Improv. 1994 Aug;20(8):425–442. doi: 10.1016/s1070-3241(16)30088-8. [DOI] [PubMed] [Google Scholar]
- Rosenthal G. E., Quinn L., Harper D. L. Declines in hospital mortality associated with a regional initiative to measure hospital performance. Am J Med Qual. 1997 Summer;12(2):103–112. doi: 10.1177/0885713X9701200204. [DOI] [PubMed] [Google Scholar]
- Rosenthal G. E., Shah A., Way L. E., Harper D. L. Variations in standardized hospital mortality rates for six common medical diagnoses: implications for profiling hospital quality. Med Care. 1998 Jul;36(7):955–964. doi: 10.1097/00005650-199807000-00003. [DOI] [PubMed] [Google Scholar]
- Steen P. M., Brewster A. C., Bradbury R. C., Estabrook E., Young J. A. Predicted probabilities of hospital death as a measure of admission severity of illness. Inquiry. 1993 Summer;30(2):128–141. [PubMed] [Google Scholar]


