Abstract
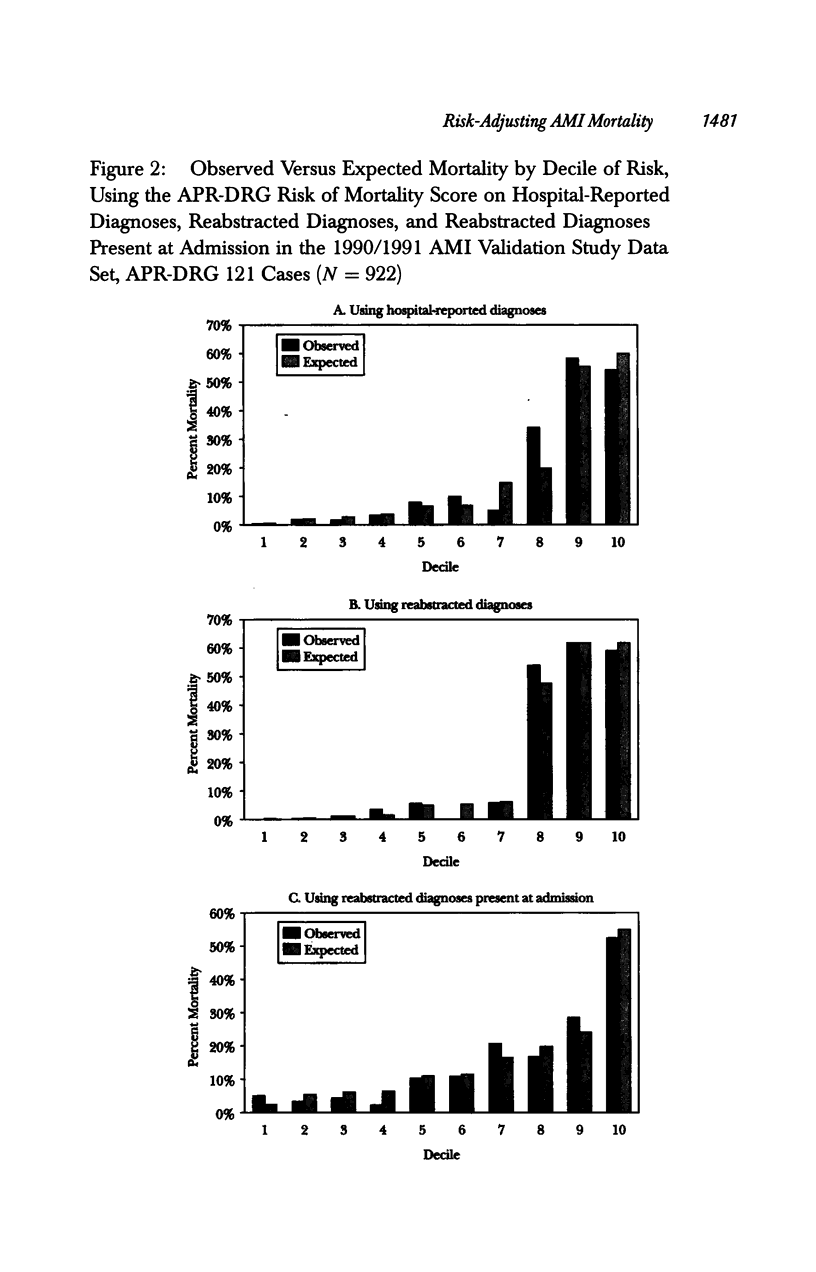
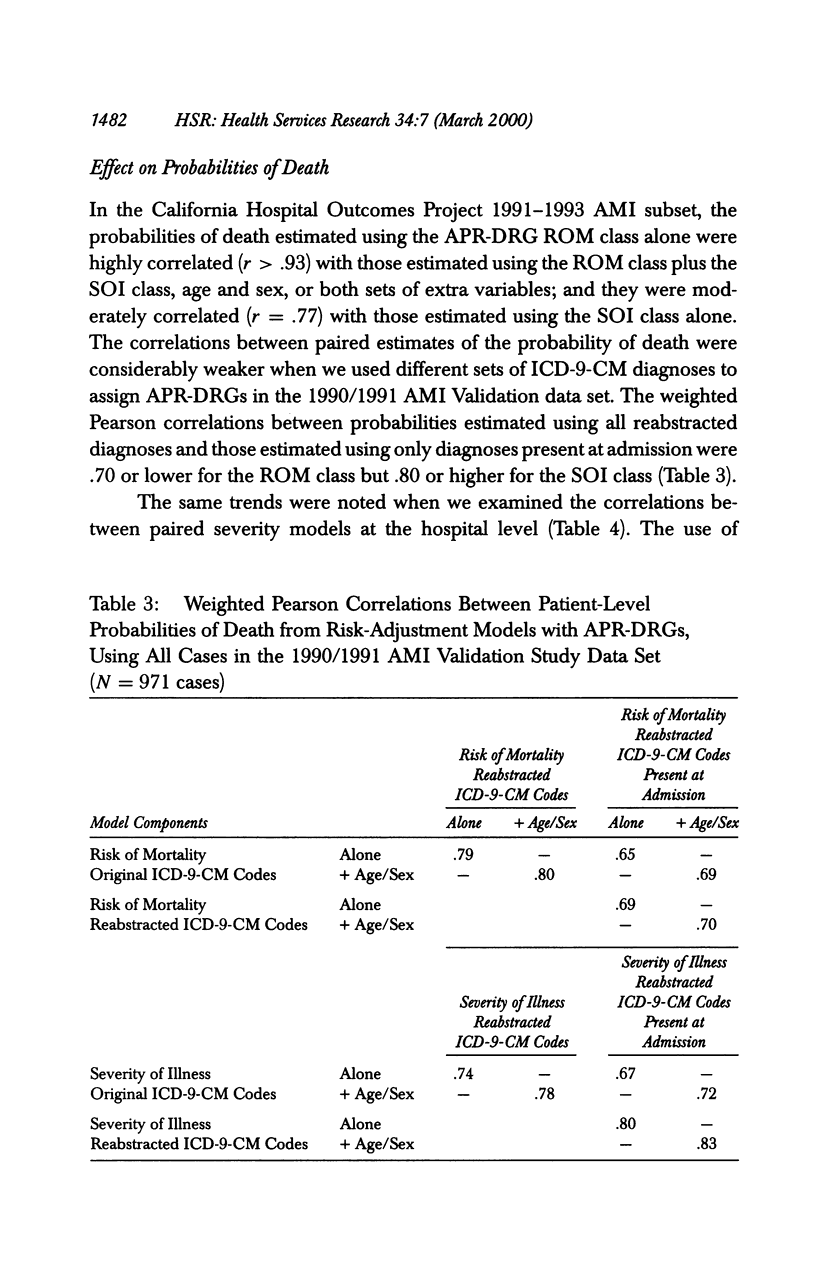
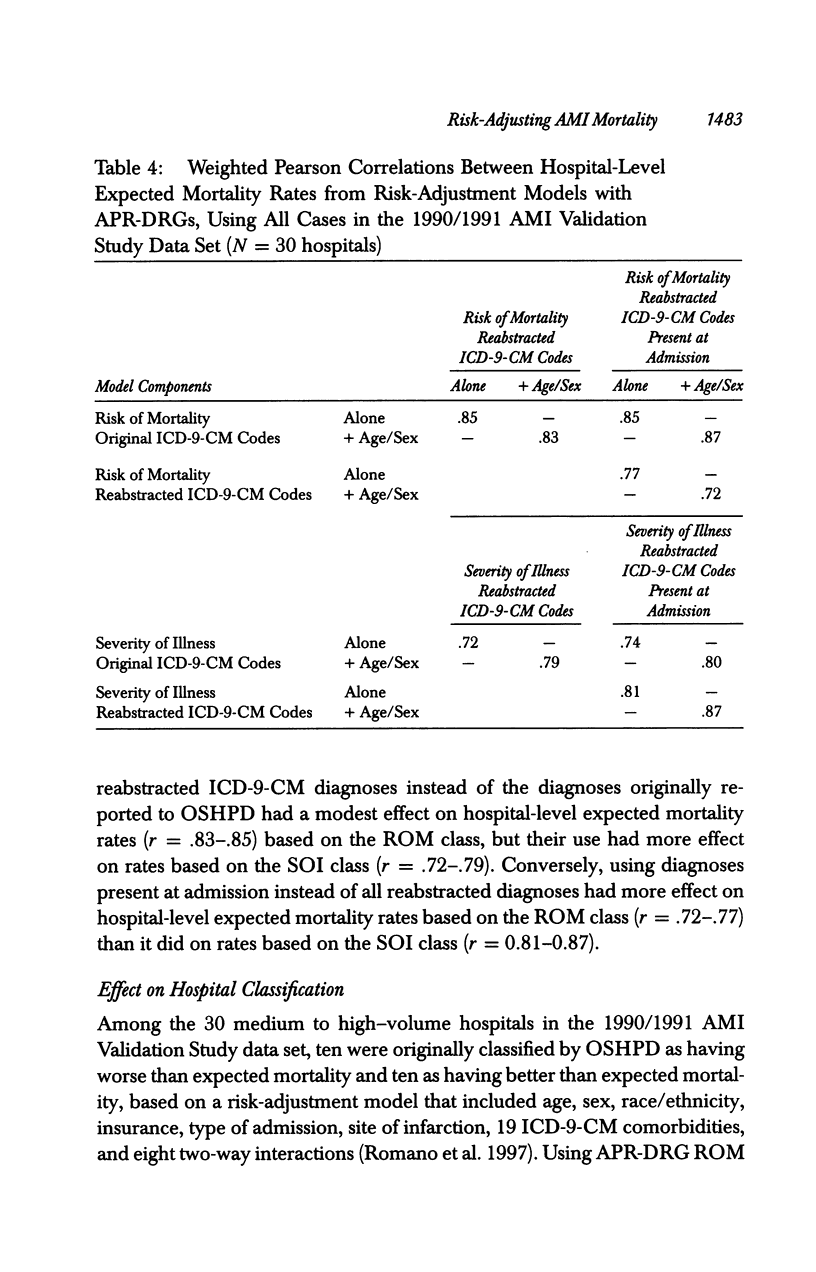
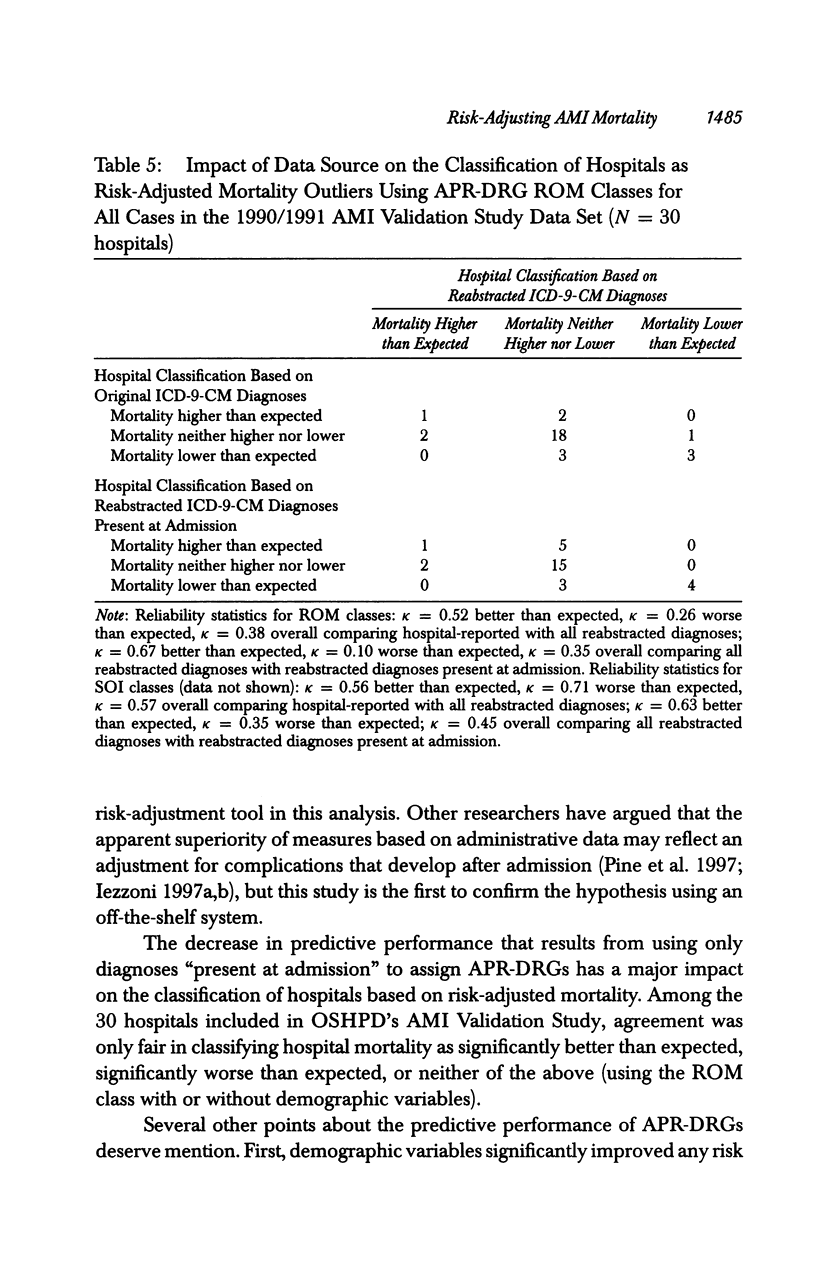
OBJECTIVE: To determine if a widely used proprietary risk-adjustment system, APR-DRGs, misadjusts for severity of illness and misclassifies provider performance. DATA SOURCES: (1) Discharge abstracts for 116,174 noninstitutionalized adults with acute myocardial infarction (AMI) admitted to nonfederal California hospitals in 1991-1993; (2) inpatient medical records for a stratified probability sample of 974 patients with AMIs admitted to 30 California hospitals between July 31, 1990 and May 31, 1991. STUDY DESIGN: Using the 1991-1993 data set, we evaluated the predictive performance of APR-DRGs Version 12. Using the 1990/1991 validation sample, we assessed the effect of assigning APR-DRGs based on different sources of ICD-9-CM data. DATA COLLECTION/EXTRACTION METHODS: Trained, blinded coders reabstracted all ICD-9-CM diagnoses and procedures, and established the timing of each diagnosis. APR-DRG Risk of Mortality and Severity of Illness classes were assigned based on (1) all hospital-reported diagnoses, (2) all reabstracted diagnoses, and (3) reabstracted diagnoses present at admission. The outcome variables were 30-day mortality in the 1991-1993 data set and 30-day inpatient mortality in the 1990/1991 validation sample. PRINCIPAL FINDINGS: The APR-DRG Risk of Mortality class was a strong predictor of death (c = .831-.847), but was further enhanced by adding age and sex. Reabstracting diagnoses improved the apparent performance of APR-DRGs (c = .93 versus c = .87), while using only the diagnoses present at admission decreased apparent performance (c = .74). Reabstracting diagnoses had less effect on hospitals' expected mortality rates (r = .83-.85) than using diagnoses present at admission instead of all reabstracted diagnoses (r = .72-.77). There was fair agreement in classifying hospital performance based on these three sets of diagnostic data (K = 0.35-0.38). CONCUSIONS: The APR-DRG Risk of Mortality system is a powerful risk-adjustment tool, largely because it includes all relevant diagnoses, regardless of timing. Although some late diagnoses may not be preventable, APR-DRGs appear suitable only if one assumes that none is preventable.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alemi F., Rice J., Hankins R. Predicting in-hospital survival of myocardial infarction. A comparative study of various severity measures. Med Care. 1990 Sep;28(9):762–775. doi: 10.1097/00005650-199009000-00006. [DOI] [PubMed] [Google Scholar]
- Brailer D. J., Kroch E., Pauly M. V., Huang J. Comorbidity-adjusted complication risk: a new outcome quality measure. Med Care. 1996 May;34(5):490–505. doi: 10.1097/00005650-199605000-00010. [DOI] [PubMed] [Google Scholar]
- Hanley J. A., McNeil B. J. The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982 Apr;143(1):29–36. doi: 10.1148/radiology.143.1.7063747. [DOI] [PubMed] [Google Scholar]
- Hosmer D. W., Hosmer T., Le Cessie S., Lemeshow S. A comparison of goodness-of-fit tests for the logistic regression model. Stat Med. 1997 May 15;16(9):965–980. doi: 10.1002/(sici)1097-0258(19970515)16:9<965::aid-sim509>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I., Ash A. S., Shwartz M., Daley J., Hughes J. S., Mackiernan Y. D. Judging hospitals by severity-adjusted mortality rates: the influence of the severity-adjustment method. Am J Public Health. 1996 Oct;86(10):1379–1387. doi: 10.2105/ajph.86.10.1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iezzoni L. I., Ash A. S., Shwartz M., Landon B. E., Mackiernan Y. D. Predicting in-hospital deaths from coronary artery bypass graft surgery. Do different severity measures give different predictions? Med Care. 1998 Jan;36(1):28–39. doi: 10.1097/00005650-199801000-00005. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I., Daley J., Heeren T., Foley S. M., Fisher E. S., Duncan C., Hughes J. S., Coffman G. A. Identifying complications of care using administrative data. Med Care. 1994 Jul;32(7):700–715. doi: 10.1097/00005650-199407000-00004. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I., Shwartz M., Ash A. S., Hughes J. S., Daley J., Mackiernan Y. D. Severity measurement methods and judging hospital death rates for pneumonia. Med Care. 1996 Jan;34(1):11–28. doi: 10.1097/00005650-199601000-00002. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I., Shwartz M., Ash A. S., Hughes J. S., Daley J., Mackiernan Y. D. Using severity-adjusted stroke mortality rates to judge hospitals. Int J Qual Health Care. 1995 Jun;7(2):81–94. doi: 10.1093/intqhc/7.2.81. [DOI] [PubMed] [Google Scholar]
- Iezzoni L. I. The risks of risk adjustment. JAMA. 1997 Nov 19;278(19):1600–1607. doi: 10.1001/jama.278.19.1600. [DOI] [PubMed] [Google Scholar]
- Landis J. R., Koch G. G. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–174. [PubMed] [Google Scholar]
- Pine M., Norusis M., Jones B., Rosenthal G. E. Predictions of hospital mortality rates: a comparison of data sources. Ann Intern Med. 1997 Mar 1;126(5):347–354. doi: 10.7326/0003-4819-126-5-199703010-00002. [DOI] [PubMed] [Google Scholar]
- Selker H. P., Griffith J. L., D'Agostino R. B. A time-insensitive predictive instrument for acute myocardial infarction mortality: a multicenter study. Med Care. 1991 Dec;29(12):1196–1211. doi: 10.1097/00005650-199112000-00003. [DOI] [PubMed] [Google Scholar]
- Silber J. H., Williams S. V., Krakauer H., Schwartz J. S. Hospital and patient characteristics associated with death after surgery. A study of adverse occurrence and failure to rescue. Med Care. 1992 Jul;30(7):615–629. doi: 10.1097/00005650-199207000-00004. [DOI] [PubMed] [Google Scholar]
- Soeken K. L., Prescott P. A. Issues in the use of kappa to estimate reliability. Med Care. 1986 Aug;24(8):733–741. doi: 10.1097/00005650-198608000-00008. [DOI] [PubMed] [Google Scholar]




