Abstract
Study Objectives:
This study sought to characterize sleep and the circadian rhythm of body core temperature of an individual with delayed sleep phase disorder (DSPD) in the absence of temporal cues and social entrainment and to compare those measures to age-matched normal control subjects studied under identical conditions.
Design:
Polysomnography and body temperature were recorded continuously for 4 days in entrained conditions, followed immediately by 17 days in a “free-running” environment.
Setting:
Temporal isolation facility in the Laboratory of Human Chronobiology, Weill Cornell Medical College.
Participants:
One individual who met criteria for delayed sleep phase disorder according to the International Classification of Sleep Disorders Diagnostic and Coding Manual (ICSD-2) and 3 age-matched control subjects.
Interventions:
None.
Measurements and Results:
The DSPD subject had a spontaneous period length (tau) of 25.38 hours compared to an average tau of 24.44 hours for the healthy controls. The DSPD subject also showed an altered phase relationship between sleep/wake and body temperature rhythms, as well as longer sleep latency, poorer sleep efficiency, and altered distribution of slow wave sleep (SWS) within sleep episodes, compared to control subjects.
Conclusions:
Delayed sleep phase disorder may be the reflection of an abnormal circadian timing system characterized not only by a long tau, but also by an altered internal phase relationship between the sleep/wake system and the circadian rhythm of body temperature. The latter results in significantly disturbed sleep, even when DSPD patients are permitted to sleep and wake at their preferred times.
Citation:
Campbell SS; Murphy PJ. Delayed sleep phase disorder in temporal isolation. SLEEP 2007;30(9):1225-1228.
Keywords: Delayed sleep phase, circadian rhythm, free-run, tau, polysomnography
INTRODUCTION
DELAYED SLEEP PHASE DISORDER (DSPD), THE MOST COMMONLY DIAGNOSED FORM OF A CLASS OF DISORDERS KNOWN AS “CIRCADIAN RHYTHM SLEEP disorders” is characterized by delayed major sleep episodes, in relation to the desired clock time, typically by more than 2 hours and often by as much as 6 hours.1,2 This results in symptoms of sleep-onset insomnia, as well as difficulty in awakening alert and refreshed at the desired time on the following day. Yet, once asleep, DSPD patients frequently report satisfactory sleep, and when permitted to sleep on a self-selected schedule, their sleep is reported to be of normal duration and quality, though, as discussed later, the limited objective data do not generally support this characterization.
Several theories have been offered regarding the pathophysiology of the disorder, all of which hypothesize a reduced capacity to achieve the daily phase advance required to entrain the endogenous clock to the 24-hour day. One assumption underlying such hypotheses is that individuals with DSPD have an abnormally long spontaneous period length, or tau.3 However, to date there are no published reports characterizing spontaneous circadian rhythmicity in DSPD patients. Thus, the question remains as to whether an abnormally long spontaneous period length may contribute to the constellation of symptoms that define DSPD. We describe the sleep and body temperature rhythms of an individual with DSPD studied in temporal isolation.
METHODS
Subjects
The DSPD subject was a 30-year-old male graduate student who reported a lifelong history of very late bedtimes and an inability to awaken refreshed until the early afternoon. Physical and psychiatric screenings revealed no pathology. His score on the Horne-Östberg Morningness-Eveningness scale4 was 31, which classified him as an extreme evening type. As part of an ongoing study to assess circadian rhythmicity in older vs younger individuals, data were obtained from 3 healthy normal subjects close to the DSPD subject's age (2 females, aged 19 and 26, and a male, aged 32).
Procedure
The study was approved by the Weill Cornell Medical College Committee on Human Rights in Research and subjects provided written informed consent. All were compensated for participation.
Following enrollment in the study, subjects maintained daily sleep logs for 2 consecutive weeks while living at home and continuing their usual daily activities. They then underwent a laboratory session that continued for 23 consecutive days and nights. Throughout their stay in the lab, subjects lived in a studio apartment that was shielded from any cues to time of day. Illumination was provided by desk and floor lamps situated around the apartment. Illumination in different areas of the apartment ranged from 10 lux to 100 lux, with a typical level (e.g., while seated on the sofa, or in a reclining chair) of between 30 and 50 lux.
The first 2 nights in the lab were used for adaptation and to screen for sleep disorders (i.e., apnea and periodic leg movements of sleep [PLMS]). This was followed by a 4-day entrainment period, during which sleep and rising times, as well as meal times, were circumscribed. Before retiring on the fourth night, subjects were informed that the “free-run” portion of the study would commence when they awakened the following morning.
For the next 17 days, subjects were permitted to self-select bedtimes and wake times and to eat meals at their discretion. Subjects were allowed to engage in activities of their choice, with the exception of strenuous exercise, and they were not permitted to nap. If sleep was detected at any time other than when a subject declared his/her intention to retire “for the night,” (s)he was immediately awakened and reminded of the prohibition against napping. Sleep was recorded polygraphically on the adaptation and entrainment nights. EEG, EOG, and EMG were recorded continuously throughout the free-run portion (except when subjects showered), via a telemetry system (Biosentry, Torrance, CA) that permitted freedom of movement around the isolation apartment. Body core temperature was also recorded continuously, in 2-minute epochs, using a rectal thermistor, connected to an ambulatory data storage device (Minilogger, Minimitter, Inc. Bend, OR). Closed-circuit TV permitted observation of subjects throughout the laboratory session, and an intercom system permitted communication when necessary.
Data Analysis
Sleep records were scored in 30-second epochs using standard criteria.5 Sleep onset was defined by the first epoch of stage 2 sleep. Summary sleep measures were obtained by averaging data from sleep episodes recorded on 15 of the 17-day free-run period for the DSPD subject (data from 2 days were not available due to equipment malfunction) and from 48 of 54 free-run sleep episodes for the normal controls. Data from the first night were not used because subjects had circumscribed bedtimes.
Raw body temperature data were edited for artifact (e.g., when the thermistor is removed for showering). Curve-fitting techniques using a harmonic regression model were used to estimate parameters of the temperature rhythm, including the daily minimum (tmin). Linear regression on the daily time of tmin was used to calculate spontaneous period length (tau). Daily times of tmin was also used in the calculation of phase angle between sleep/wake and temperature rhythms.
All comparisons were made using one-way and two-way (for halves of the night analyses) ANOVA, with the exception of sleep onset latency. Because this measure showed significantly skewed distributions, the Kruskal-Wallis one-way ANOVA by ranks was used. All P values are based on two-tailed tests of significance.
RESULTS
Entrained Phase
The DSPD subject's home sleep log confirmed his report of very late sleep and waking times. Average bedtime was 03:38 and average waking time was 13:47 (average time in bed = 10.15 hrs). His mean estimated sleep latency was 50 minutes, resulting in an average sleep period time of 9.32 hours. On all but one day, the subject used an alarm clock to awaken. The day on which an alarm clock was not used, the subject reported a bedtime of 06:00 and an awakening time of 16:30. That the subject's circadian system was delayed was verified further by temperature data obtained during the entrainment portion of the lab session. Because his scheduled wake time in the lab was 10:00, the subject's temperature minimum was masked by rising from bed (i.e., he had not yet reached his tmin by 10:00). However, the curve fits of his 4-day entrained data revealed an average acrophase (temperature maximum) of 2452 h, compared to an average of 1953 h (SD=1 h 23 m) for the 3 controls.
Spontaneous Period
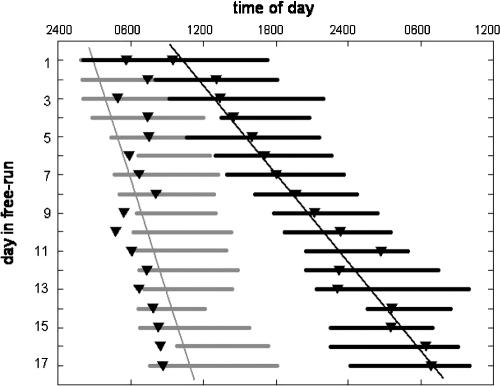
Figure 1 shows a plot of the DSPD subject's sleep/wake pattern and daily temperature minima (tmin) across the free-run portion of the protocol. For the entire 17-day interval, the subject exhibited an average tau of 25.38 hours. This is compared to an average tau of 24.44 hours for the 3 normal young adults.
Figure 1.
Timing of spontaneous sleep periods (bars) and daily temperature minima (inverted triangles) for the subject with DSPD (dark) and for a normal 32-year-old male subject (light gray), across 17 days of temporal isolation. The DSPD subject exhibited a spontaneous period length (tau) of 25.38 hrs compared to 24.19 hrs for the normal subject. The figure also shows the altered phase relationship between sleep and body temperature in the DSPD subject (see text and Figure 2 for details).
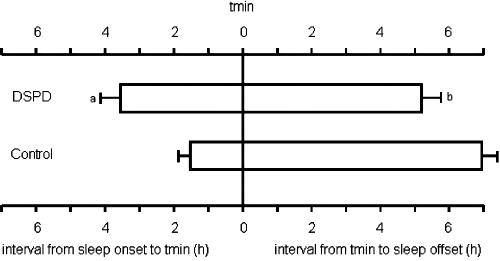
As shown in Figure 2, the phase relationship between the subject's sleep and body temperature was also altered relative to normal subjects. Whereas, the average phase angle between sleep onset and tmin was 1.63 h (SD = 2.74) for the 3 normal subjects, the DSPD subject showed an average phase angle of 3.62 h (SD = 2.22) (P < 0.02). Conversely, sleep offset occurred more closely to tmin in the DSPD subject than in the normal subjects (5.15 ± 2.26 h versus 6.96 ± 3.16 h, P = 0.053).
Figure 2.
Average phase relationship between the timing of spontaneous sleep (open bars) and the minimum of body temperature (tmin; vertical line) for the DSPD subject (top) and for three similarly-aged control subjects studied under identical conditions. Shown are average intervals (and standard error) from sleep onset to tmin (3.62 h vs 1.63 h, P <0.02) and from tmin to sleep offset (5.15 h versus 6.96 h, P = 0.053).
Spontaneous Sleep
Table 1 shows the comparison of sleep between the DSPD subject and the 3 comparison subjects. Based on data averaged over 14 sleep periods for the DSPD subject and 47 sleep episodes for the comparison subjects, the DSPD subject exhibited a significantly longer sleep onset latency, significantly greater wake time after sleep onset (WASO), significantly less stage 2 sleep and significantly poorer sleep efficiency. Examination of sleep by halves of the night revealed that the distribution of SWS was altered in the DSPD subject, with 35.2% of his total SWS occurring in the second half of the night, compared to 11.8 % in the control subjects (P <0.0001).
Table 1.
Comparison of Polysomnographically Derived Sleep Measures (with SD) Averaged From Spontaneous Sleep Episodes Recorded During Temporal Isolation From One DSPD Subject (14 Episodes) and 3 Similarly-aged Normal Subjects (47 Episodes)
| Sleep measure | DSPD (14 sleep episodes) | Normal (47 sleep episodes) |
|---|---|---|
| sleep onset latency (SOL) | 38.1 (36.8)* | 16.7 (16.8) |
| total sleep time (TST) | 436.8 (99.4) | 455.8 (101.1) |
| sleep period time (SPT) | 524.4 (108.2) | 510.6 (109.9) |
| sleep efficiency (TST/SPT) | 82.8 (8.9) ** | 89.4 (6.2) |
| % wake after sleep onset (WASO) | 16.9 (9.0) ** | 10.5 (6.2) |
| % stage 1 | 4.9 (1.8) | 5.3 (2.5) |
| % stage 2 | 36.3 (4.5)** | 44.2 (7.7) |
| % stages 3 & 4 (SWS) | 14.8 (6.6) | 13.2 (6.6) |
| % REM | 26.9 (8.2) | 26.7 (5.6) |
significantly different from normal (one-way ANOVAs; P <0.01).
significantly different from normal (due to skewed distribution in SOL, Kruskal-Wallis one-way ANOVA by ranks was used; P <0.01).
DISCUSSION
To our knowledge, this is the first report of a documented case of DSPD studied under conditions in which spontaneous period length (tau) could be measured. The results suggest that the phase disturbances that characterize DSPD under entrained conditions may be the consequence of a fundamental abnormality of the circadian timing system. For the subject studied here, this was reflected not only in a long tau, but also in an altered phase relationship between the timing of sleep and the circadian rhythm of body core temperature.
Although the latter finding has been reported previously in patients studied in entrained conditions,6,7 that such an alteration was also observed in temporal isolation supports the notion that the etiology of DSPD goes beyond simply a reduced capacity to achieve and maintain the appropriate phase relationship between sleep timing and the 24-hour day. Rather, the disorder may also reflect a fundamental inability of the endogenous circadian timing system to maintain normal internal phase relationships among physiological systems, and to properly adjust those internal relationships within the confines of the 24-hour day.
In normal subjects, the phase relationship between sleep and temperature changes in temporal isolation relative to that observed under entrained conditions8: in isolation, tmin tends to occur toward the beginning of sleep. Under entrained conditions, tmin occurs, instead, toward the end of the sleep period, a change in phase angle of several hours. A comparison of our findings with those from DSPD patients studied in entrainment6,7 suggests that those with DSPD may have a reduced capacity to achieve such a change in phase angle in response to entrainment.
Our findings further suggest, possibly as a consequence of these altered internal phase relationships, that the quality of sleep in DSPD may be substantially poorer than that of normal subjects, even when bedtimes and wake times are self-selected. Our DSPD subject exhibited an average sleep onset latency twice that of the 3 control subjects and almost twice the amount of wakefulness after sleep onset (WASO) as control subjects, resulting in significantly poorer sleep efficiency. Also, the temporal distribution of slow wave sleep was significantly altered in the DSPD subject. This finding may suggest that, in addition to abnormal circadian clock function, DSPD may be characterized by alteration(s) in the homeostatic regulation of sleep, as well. Specifically, the rate with which Process S 9 is depleted during sleep may be slowed. This could, conceivably, contribute to the excessive sleep inertia upon awakening that is often reported by DSPD sufferers.
The few published reports of polysomnographically recorded sleep in DSPD are in general agreement with those reported here. For example, in their initial description of the disorder, Weitzman and coworkers reported polysomnographic sleep measures in 6 individuals diagnosed with DSPD.10 With sleep times scheduled to correspond to subjects' preferred sleep times (average bedtime: 04:04), the investigators reported an average sleep efficiency of only 80% and an average sleep onset latency of 41 minutes. Thorpy et al11 reported similar results for 9 adolescent DSPD patients (mean sleep latency: 51.9 min; mean sleep efficiency: 83.9%) and Watanabe and coworkers7 observed significantly longer sleep onset latencies, more WASO, and reduced sleep efficiency, and altered distribution of slow wave sleep in 11 DSPD patients sleeping at their habitual sleep times, when compared to age-matched controls.
Though quite limited in terms of the total number of DSPD patients studied, such data seem to contradict the notion that DSPD is merely a disorder of sleep timing, rather than a disorder of the sleep system itself. If additional studies support these results, a reassessment of the nature of sleep in DSPD, the diagnostic guidelines derived there from, as well as, revised approaches to treatment of the disorder, may be warranted.
It is unlikely that light exposure during temporal isolation contributed to the long period length observed in our DSPD subject. As mentioned, illumination was maintained at well below 50 lux in the isolation apartment. Moreover, as there is no reason to assume that control subjects were exposed to light in a fundamentally different manner than the DSPD subject, any impact of light would be expected to be consistent across all subjects. Nevertheless, we cannot entirely rule out the possibility that light acted differentially on the endogenous clock of our DSPD subject, resulting in the longer tau. It has been suggested, for example, that symptoms of DSPD may be the reflection of a “weak” portion of the phase response curve (PRC) to one or more phase re-setting stimuli,10 of which light is clearly a major one. It has also been hypothesized that, due to the altered phase angle between sleep and temperature observed in DSPD, and the tendency for longer sleep periods, these individuals may simply sleep through the phase-advance portion of the light PRC.12 As more individuals with DSPD are studied under conditions in which spontaneous period length can be measured, a more complete understanding of the factors underlying the disorder is sure to emerge.
ACKNOWLEDGMENTS
This work was supported by NIH grants R01 MH54617, R01 AG12112, R56 AG15370, R01 NS052495 and the Department of Psychiatry's Reader's Digest DeWitt-Wallace Fund. The authors gratefully acknowledge the technical assistance of the staff of the Laboratory of Human Chronobiology and the substantial commitment of time and effort by our research participants.
Footnotes
Disclosure Statement
This was not an industry supported study. Drs. Campbell and Murphy have indicated no financial conflicts of interest.
REFERENCES
- 1.American Academy of Sleep Medicine. diagnostic and coding manual. 2nd ed. Westchester, Illinois: American Academy of Sleep Medicine; 2005. International classification of sleep disorders. [Google Scholar]
- 2.Campbell S, Murphy P, Van den Heuvel C, Roberts M, Stauble T. Etiology and treatment of intrinsic circadian rhythm sleep disorders. Sleep Med Rev. 1999;3:179–200. doi: 10.1016/s1087-0792(99)90001-1. [DOI] [PubMed] [Google Scholar]
- 3.Czeisler C, Richardson G, Coleman R, et al. Chronotherapy: resetting the circadian clocks of patients with delayed sleep phase insomnia. Sleep. 1981;4:1–21. doi: 10.1093/sleep/4.1.1. [DOI] [PubMed] [Google Scholar]
- 4.Horne JA, Ostberg O. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 1976;4:97–110. [PubMed] [Google Scholar]
- 5.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: UCLA Brain Information Service/Brain Research Institute; 1968. [Google Scholar]
- 6.Uchiyama M, Okawa M, Shibui K, et al. Altered phase relation between sleep timing and core body temperature rhythm in delayed sleep phase syndrome and non-24-hour sleep-wake syndrome in humans. Neurosci Lett. 2000;294:101–4. doi: 10.1016/s0304-3940(00)01551-2. [DOI] [PubMed] [Google Scholar]
- 7.Watanabe T, Kajimura N, Kato M, et al. Sleep and circadian rhythm disturbances in patients with delayed sleep phase syndrome. Sleep. 2003;26:657–61. doi: 10.1093/sleep/26.6.657. [DOI] [PubMed] [Google Scholar]
- 8.Wever R. The circadian system of man: results of experiments under temporal isolation. New York: Springer-Verlag; 1979. [Google Scholar]
- 9.Daan S, Beersma D, Borbely A. Timing of human sleep: recovery process gated by a circadian pacemaker. Am J Physiol. 1984;2:R161–83. doi: 10.1152/ajpregu.1984.246.2.R161. [DOI] [PubMed] [Google Scholar]
- 10.Weitzman E, Czeisler C, Coleman R, Spielman A, Zimmerman J, Dement W. Delayed sleep phase syndrome. Arch Gen Psychiatry. 1981;38:737–46. doi: 10.1001/archpsyc.1981.01780320017001. [DOI] [PubMed] [Google Scholar]
- 11.Thorpy M, Korman E, Spielman A, Glovinsky P. Delayed sleep phase syndrome in adolescents. J Adolesc Health Care. 1988;9:22–7. doi: 10.1016/0197-0070(88)90014-9. [DOI] [PubMed] [Google Scholar]
- 12.Ozaki S, Uchiyama M, Shirakawa S, Okawa M. Prolonged interval from body temperature nadir to sleep offset in patients with delayed sleep phase syndrome. Sleep. 1996;19:36–40. [PubMed] [Google Scholar]