Abstract
Lentiviral envelope antigenic variation and associated immune evasion are believed to present major obstacles to effective vaccine development. Although this perception is widely assumed by the scientific community, there is, to date, no rigorous experimental data assessing the effect of increasing levels of lentiviral Env variation on vaccine efficacy. It is our working hypothesis that Env is, in fact, a primary determinant of vaccine effectiveness. We previously reported that a successful experimental attenuated equine infectious anemia virus vaccine, derived by mutation of the viral S2 accessory gene, provided 100% protection from disease after virulent virus challenge. Here, we sought to comprehensively test our hypothesis by challenging vaccinated animals with proviral strains of defined, increasing Env variation, using variant envelope SU genes that arose naturally during experimental infection of ponies with equine infectious anemia virus. The reference attenuated vaccine combined with these variant Env challenge strains facilitated evaluation of the protection conferred by ancestral immunogens, because the Env of the attenuated vaccine is a direct ancestor to the variant proviral strain Envs. The results demonstrated that ancestral Env proteins did not impart broad levels of protection against challenge. Furthermore, the results displayed a significant inverse linear correlation of Env divergence and protection from disease. This study demonstrates potential obstacles to the use of single isolate ancestral Env immunogens. Finally, these findings reveal that relatively minor Env variation can pose a substantial challenge to lentiviral vaccine immunity, even when attenuated vaccines are used that, to date, achieve the highest levels of vaccine protection.
Keywords: ancestral immunogen, equine infectious anemia virus, lentivirus
Genomic and antigenic variation are recognized by the global scientific community as fundamental characteristics of HIV type 1 (HIV-1) infection, and it is widely accepted, although unproven, that HIV-1 antigenic diversity presents a major obstacle to HIV-1/AIDS vaccine development (1–5). Lentiviral antigenic variation is most pronounced in the viral Env proteins that serve as initial primary targets for host immune responses. Studies on the effect of Env variation on antigenic properties indicate that even minor changes in amino acid sequence can dramatically alter antibody and CTL specificities in in vitro assays and immune control of persistent infections in vivo (6–17). Nevertheless, even apparently extensive Env variations may not necessarily cause detectable changes in immune phenotype as measured by in vitro assays alone (18).
Equine infectious anemia virus (EIAV), a macrophage-tropic lentivirus, causes persistent infection and a dynamic chronic disease in equids (19). Infection, transmitted by blood-feeding horse flies, occurs in three stages: acute, chronic, and inapparent. The acute and chronic stages are defined by episodes of clinical disease, triggered by waves of viremia, and distinguished by fever, anemia, thrombocytopenia, edema, and various wasting signs. By 1 year after infection, animals typically progress to life-long inapparent carriers, continuing to harbor steady-state levels of viral replication in monocyte-rich tissue reservoirs (19–21). Stress or immune suppression of inapparent carriers can induce increases in viral replication and, potentially, a recrudescence of disease (19, 22). Among virulent lentiviruses, however, EIAV is unique in that, despite aggressive virus replication and associated rapid antigenic variation, >90% of infected animals progress from a chronic disease state to an inapparent carrier stage, which is achieved by a strict immunologic control over virus replication (19). The EIAV system therefore serves as a unique animal model for the natural immunologic control of lentiviral replication and disease. In addition, inapparent carriers of EIAV have proven to be remarkably resistant to subsequent virus exposure to diverse viral strains, indicating the development of a high level of prophylactic immunity. Thus, the EIAV system provides a useful model for identifying critical immune correlates of protection and ascertaining the potential for developing effective prophylactic lentivirus vaccines.
We have previously reported serial studies evaluating the efficacy of an attenuated EIAV proviral vaccine containing a mutation in the viral S2 accessory gene (EIAVD9) (23–25). The results of these studies indicate that horses inoculated with the EIAVD9 viral vaccine were 100% protected from disease by virulent EIAV challenge. Initial vaccine studies indicated that the experimentally immunized horses achieved an apparent “sterilizing immunity,” based on the lack of detectable challenge virus infection by using sensitive diagnostic serological and genetic assays. However, further rigorous assays of plasma RNA from vaccinated and challenged animals subjected to chemical immune suppression demonstrated that ≈50% of the animals harbored challenge virus, despite the fact that 100% remained asymptomatic for EIA (23). Although the attenuated EIAV proviral vaccine may not achieve sterilizing immunity, the attenuated EIAV vaccine consistently provides complete protection from disease. Thus, the EIAV system mirrors other animal lentivirus vaccine models that have consistently identified attenuated vaccines, among various vaccine strategies evaluated to date, as producing the highest level of vaccine protection, typically against homologous virus challenge (26, 27).
Despite the abundance of research dedicated to HIV-1 vaccine development and the commonly accepted notion that HIV-1 genetic diversity and antigenic variation directly impact immune recognition and vaccine efficacy, there is, to date, no conclusive experimental data assessing the effect of defined, increasing levels of lentiviral Env variation on vaccine efficacy. It is our working hypothesis that Env is, in fact, a primary determinant of lentiviral vaccine efficacy. Previous EIAV vaccine trials from our lab have used a challenge virus strain expressing envelope proteins homologous to the vaccine strain. In this study, we sought to directly test the role of defined Env variation in vaccine efficacy by the well characterized attenuated EIAV vaccine. The studies were designed (i) to evaluate the role of Env as an overall determinant of vaccine efficacy, (ii) to define the correlation of the extent of defined Env variation and vaccine efficacy, and (iii) to test the ability of a vaccine containing an ancestor Env to protect against naturally occurring derivative Env species.
Results
Development of Variant Challenge Strains.
To develop challenge strains of increasing divergence from the parental vaccine strain, we used EIAV variant strains from a quasispecies population previously isolated and characterized as part of various studies on EIAV genetic and antigenic evolution during persistent infections with the reference EIAVPV strain (21, 28–30). The EIAVD9 attenuated vaccine strain was derived from molecular clones generated from the EIAVPV strain (25, 31). Thus, the combination of the EIAVPV-derived EIAVD9 vaccine Env and the EIAVPV–evolved challenge quasispecies represent a natural ancestral relationship, allowing a direct test of the efficacy of vaccine immunity to ancestor envelope immunogens.
Genomic evolution in the EIAVPV envelope transmembrane (gp45) protein has been shown to be minimal among the characterized longitudinal EIAV isolates (28, 32); consequently, we elected to focus on the surface envelope protein, gp90, for the construction of variant envelope challenge strains. We chose viral isolates that varied over time from the inoculating strain (and hence the vaccine EIAVD9) by increasing amounts of divergence [see supporting information (SI) Fig. 4], were phylogenetically distinct (SI Fig. 5), and displayed amino acid sequence heterogeneity in previously identified immunological determinants of the gp90 protein (13, 14) (SI Fig. 6). The two proviral clones chosen for the production of variant challenge strains were derived from plasma viral isolates that were acquired ≈1,000 days apart and that diverged from EIAVPV and EIAVD9 at the amino acid level by 6% and 13%. The gp90 genes of these isolates were cloned by using standard techniques (14, 32) into our proviral molecular clone EIAVUK3 (33) and were termed EV6 and EV13, respectively. EIAVUK3, which is derived from our EIAVPV biological clone (hence the envelope is homologous to EIAVPV/EIAVD9) was also used as a proviral challenge strain and was termed EV0. Thus, the current strategy allowed us to use a common proviral backbone to create our series of challenge viruses with variant envelopes derived from a common parental strain, EIAVPV. Challenge virus strains differ only in envelope sequences and represent a logical ancestor relationship expected for an evolving lentiviral population, as would be observed within distinct geographical populations infected with HIV-1.
The resultant proviral clones were sequenced to verify the specific Env sequences and then transfected into equine dermal cells for production of infectious challenge virus stocks. The variant virus stocks were then titered and characterized for in vitro and in vivo replication kinetics (14, 31). All three proviral challenge strains demonstrated typical in vitro replication kinetics that peaked in virus production at ≈10 days after infection (data not shown). In vivo analysis of the proviral challenge strains by experimental infections of equids confirmed characteristic EIAV pathogenesis and virulence properties. Standard viral replication kinetics, including the induction of acute disease and progression to chronic disease, were observed for all three strains (19, 32, 34). Interestingly, assays of antibody responses elicited by experimental infections with variant challenge viruses indicated distinct neutralization phenotypes for the individual variant envelopes; each variant challenge virus was neutralized by immune serum from homologous virus infections, but not from heterologous virus infections (SI Fig. 7). Thus, these data demonstrate that the variant Env challenge viruses were similar in replication and virulence properties, but distinct in immune properties as a result of the defined Env sequence variations.
Experimental Vaccination and Challenge.
Twenty-four ponies of mixed age and gender (SI Table 3) were inoculated intramuscularly with two 103 TCID50 doses, at a 4-week interval, of EIAVD9. The inoculated ponies were monitored daily for clinical signs of EIA, and blood samples were taken at regular intervals for standard measurements of disease, virus replication, and host immune responses, as described (23–25, 35). Fig. 1 displays representative clinical profiles of vaccinated animals (detailed clinical profiles of each animal [24 vaccinates and 18 controls] are included in the SI). The vaccinates exhibited no clinical signs of EIA disease from the attenuated vaccine strain during the 7-month observation period, a time frame that allows complete maturation of vaccine immunity before virus challenge (21, 30, 36) (SI Figs. 8A–10A).
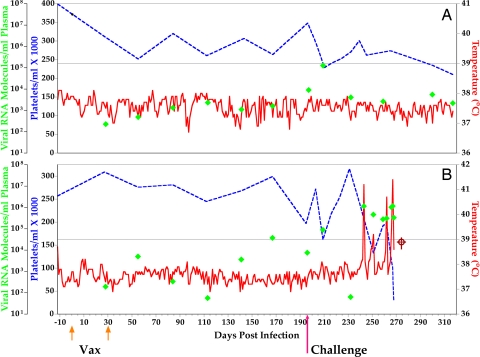
Fig. 1.
Representative clinical and virological profiles of a protected (A) and unprotected (B) challenged vaccinate. EIAV-naïve ponies were vaccinated with 103 TCID50 EIAVD9 I.M. (↑Vax↑). Rectal temperature (solid line, right y axis) and platelet counts (dashed line, first left y axis) were followed daily for up to 370 days (x axis) after the first vaccine dose. Quantification of the virus load (♦, second left y axis) was performed on viral RNA extracted from plasma at periodic time points before and after virulent virus challenge 7 months after the first vaccination with 103 TCID50 EV0, EV6, or EV13 I.M (↑Challenge). Febrile episodes were defined by a achieving a combination of two to three features such as rectal temperature >39°C in conjunction with thrombocytopenia (platelet decrease of ≥70,000/μl of whole blood), EIAV viral load ≥105 as well as other clinical signs of EIA. ⌖, animal euthanized because of severe disease.
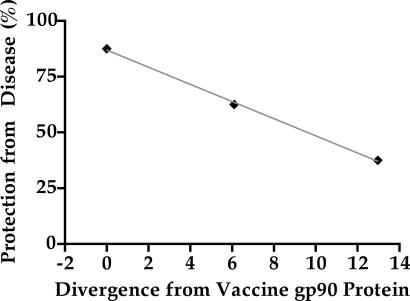
Six months after the second vaccination, the immunized ponies were randomly divided into three challenge groups, each consisting of eight animals (SI Table 3). Each trial group was then challenged by i.v. inoculation with 103 TCID50 of EV0, EV6, or EV13 (Table 1). Control groups consisting of six naïve ponies each were challenged with the three variant challenge strains, as performed with the vaccinates (SI Table 3 and SI Figs. 8B–10B). Analyses of day of challenge viral loads (Table 1) and vaccine immune responses (Table 2) indicated similar levels of vaccine virus replication and a similar maturation of vaccine immunity in all groups. Despite these similar vaccine responses, however, the groups displayed markedly different levels of disease caused by the variant virus challenges (see Fig. 1 for representative protected and unprotected clinical profiles). One EV0, three EV6, and five EV13 animals displayed clinical signs of EIA disease during the observation period after challenge (Table 1, SI Table 4, and SI Figs. 8–10). Chronic disease was observed in the majority of vaccinates that experienced initial acute disease. All six control animals of each variant virus challenge group developed clinical EIA disease, indicating 100% virulence of each variant challenge under the current experimental conditions. Linear regression analysis was used to evaluate whether Env divergence from vaccine strain was a predictive factor for protection from disease. These results of the linear regression demonstrated a direct, significant inverse linear (r2 = 0.99, P = 0.02) relationship between challenge strain Env divergence from vaccine strain and protection from disease (Fig. 2).
Table 1.
Summary of vaccine results
| Trial group | DOC average (104) viral load (SEM) | Challenge strain gp90 divergence from vaccine | Protected from disease (%) |
Protected from infection (%) |
||
|---|---|---|---|---|---|---|
| Pre-IS | Post-IS | Pre-IS | Post-IS | |||
| EV0 | 1.6 (±0.7) | 0% | 7 of 8 (87.5) | 4 of 6 (66.7) | 6 of 8 (75) | 0 of 8 (0) |
| EV6 | 0.94 (±0.2) | 6% | 5 of 8 (62.5) | 1 of 4 (25) | 3 of 8 (37.5) | 0 of 8 (0) |
| EV13 | 1.4 (±0.4) | 13% | 3 of 8 (37.5) | ND | 0 of 8 (0) | ND |
DOC, day of challenge; IS, immune suppression; ND, not done.
Table 2.
Characterization of vaccine immune responses before challenge
| Trial Group | Env-specific antibody responses |
Env-specific cellular immune responses§ |
||||
|---|---|---|---|---|---|---|
| Reciprocal antibody titer (103) | Avidity*, % | Conformation ratio† | Reciprocal NAB titer‡ | CTL-specific lysis, % | T-helper stimulation index | |
| EV0 | 6.1 (±3.3) | 32 (±2) | 1.1 (±0.03) | <25 | 6 (±3) | 6 (±3) |
| EV6 | 6.8 (±1.8) | 32 (±2) | 1.1 (±0.03) | <25 | 6 (±2) | 2 (±1) |
| EV13 | 7.0 (±2.2) | 37 (±3) | 1.1 (±0.04) | 70 (±30) | 7 (±2) | 4 (±1) |
Numbers represent averages for each trial group, All values in parentheses are SEM. DOC, day of challenge; NAB, neutralizing antibody.
*Avidity determines the relative resistance of serum antibody; antigen binding to washes with 8 M urea in ELISA assays, as described (30).
†Conformation ratios reflect the relative serum antibody reactivity to linear or conformational epitopes by comparisons of antibody reactivity with intact and denatured Env antigens in ELISA assays, as described (30); conformation ratio, denatured Env reactivity/native Env reactivity.
‡Serum neutralization titer analyses were against EIAVPV. Positive neutralization determined as reciprocal titers >25 (30).
§Cellular immune responses determined by using comprehensive pools of overlapping Env peptides, as described (52).
Fig. 2.
Linear regression analysis of the relationship between Env divergence from vaccine strain and protection from EIA. The percentage of animals protected from disease in each trial group was plotted as a function of the level of amino acid divergence of the challenge strain envelope from the vaccine strain envelope. Linear regression (gray line) analysis (GraphPad Prism v. 4.0) revealed a direct, significant inverse linear relationship between the two variables, with an r2 value of 0.99 (P = 0.02). Hence, “X” is predictive of “Y,” or divergence away from the Env of the vaccine strain is predictive of protection from disease.
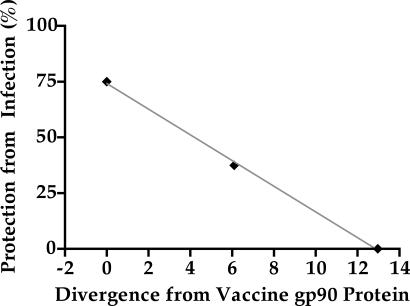
The extent of protection achieved by EIAVD9 was determined in each trial group through determinations of the circulating virus strain (vaccine vs. challenge) in the vaccinated ponies. Differential diagnostics that consisted of sensitive RT-PCR and sequencing techniques of infecting viral strains were preformed at day of challenge and after challenge (during febrile episode or 3 weeks after challenge if nonfebrile) on each animal from all three groups as previously described (23). The results of these diagnostic assays revealed distinct differences among the three challenge groups; challenge virus was detected in two EV0, five EV6, and all eight EV13 ponies. (Table 1, SI Table 4, and SI Figs. 8–10). Linear regression analysis was performed to evaluate whether Env divergence from vaccine strain was a predictive factor for protection from detectable infection with challenge strain. Once more, the results exhibited a direct, significant inverse linear (r2 = 0.99, P = 0.02) correlation of challenge strain Env divergence from vaccine strain and protection from detectable infection by challenge strain (Fig. 3).
Fig. 3.
Linear regression analysis of the relationship between Env divergence from vaccine strain and protection from detectable infection. The percentage of animals protected from detectable infection with viral strain in each trial group was plotted as a function of the level of amino acid divergence of the challenge strain envelope from the vaccine strain envelope. Linear regression (gray line) analysis (GraphPad Prism v. 4.0) revealed a direct, significant inverse linear relationship between the two variables, with an r2 value of 0.99 (P = 0.02). Hence, “X” is predictive of “Y,” or divergence away from the Env of the vaccine strain is predictive of protection from detectable infection by challenge strain.
Immune Suppression of Challenge Groups.
We previously demonstrated that chemical immune suppression with dexamethasone is critical for the accurate determination of latent infections by challenge EIAV strains. To rigorously search for the presence of challenge strain virus, we chose to immune suppress all 10 ponies from the EV0 and EV6 groups that tested negative in the diagnostic assays for challenge virus. Immune suppression was carried out over a period of 14 days, as described (23) (SI Figs. 8A and 9A). As observed (23, 29, 37), the treatment regimen caused severe immune suppression in all 10 ponies (DTH results, SI Fig. 11), with some of the treated ponies experiencing a recrudescence of EIA disease after immune suppression (Table 1, SI Table 4, and SI Figs. 8A and 9A). Most importantly, diagnostic assays of plasma viral RNA demonstrated the presence of challenge strain in all 10 ponies after immune suppression (Table 1, SI Figs. 8A and 9A, and SI Table 4). Taken together, the results of the RT-PCR assays reveal challenge virus infection in all of the trial groups. However, the ease of detection of challenge virus was, in general, inversely related to the extent of Env divergence from the vaccine strain, apparently reflecting the extent of vaccine control of virus replication in the different challenge groups.
Discussion
Among the diverse AIDS vaccine strategies tested to date in animal lentivirus models, attenuated lentivirus vaccines have uniformly provided the highest levels of immunogenicity and protection from disease (25, 27, 38–48). Consequently, we chose to test directly the role of lentiviral envelope variation in vaccine efficacy using our well characterized attenuated EIAV vaccine. The results presented here demonstrate definitively that Env can, in fact, be a primary determinant of lentiviral vaccine efficacy and that antigenic variation can circumvent even robust vaccine immunity, posing a serious challenge to AIDS vaccine development.
The data reported in this study reveal that proviral challenge strains with as little as 6% amino acid diversity from the vaccine strain surface unit proteins displayed a 25% reduction in overall protection from EIA disease. When Env divergence from vaccine strain increased to 13%, the observed reduction in protection from disease decreased by 50% compared with homologous challenge strain protection. It should be noted here that the average divergence among Env quasispecies observed between HIV-1 M clades is ≈25%, and divergence within a single clade frequently reaches 10–15%. Linear regression analysis (Fig. 2) predicts that when y = 0 (i.e., protection from disease = 0%), the x-intercept = 22.6 (i.e., divergence from vaccine gp90 protein = 22.6%); thus, the linear relationship revealed in these studies predicts that when challenge strain divergence from vaccine strain reaches 23%, none of the animals would be protected from disease. Despite the fact that immune suppression resulted in the detection of challenge virus infection in all of the vaccinated ponies after challenge, there was an inverse linear correlation between the extent of challenge virus Env divergence and the detection of challenge virus in the plasma of challenged vaccinates. The latter data indicate an inverse correlation between the extent of challenge virus Env variation and the observed efficacy of vaccine immunity in controlling challenge virus infection.
These studies highlight the importance of engineering Env immunogens that elicit a broader and more effective recognition of variant Env species compared with that achieved with an Env immunogen from a single viral isolate. Currently, the use of engineered ancestral or consensus Env sequences are being evaluated as immunogens to elicit immune responses (humoral and cellular) that can recognize a broad spectrum of HIV-1 variants within and between clades (18, 49). An important aspect of the current experimental design is that the variant challenge virus envelopes reflected a valid ancestor relationship that is representative of the natural evolution observed in HIV-1 infections. In the current study, the EIAVD9 vaccine strain Env and the homologous EV0 Env are direct ancestors to the EV6 and EV13 challenge virus Env, thus representing the levels of divergence that would be expected in a contemporary population of HIV-1 Env quasispecies. We demonstrated here that isolates diverging by as little as 6% or 13% from their ancestral envelope show markedly lower levels of protection from vaccination with the ancestral envelope. In light of the ancestral relationship of the current vaccine and challenge virus Env species, the current data suggest that the extent of divergence among even relatively closely related Env strains may circumvent immunity to engineered ancestral Env sequences, as currently being evaluated for HIV-1 vaccines. The current EIAV model now offers a unique opportunity to evaluate the potential of consensus Env immunogens to provide protective immunity to diverse Env species and to define the specific Env determinants of vaccine efficacy.
The studies presented here in the EIAV system definitively demonstrate the marked effects of Env variation on vaccine efficacy. Although it is not possible with absolute confidence to extrapolate the results of vaccine studies in any single animal lentivirus system to other animal lentiviruses or to HIV-1, the data presented here certainly highlight the priority of ascertaining the effects of Env variation on HIV-1 vaccine efficacy, after a decade of primarily focusing on Gag-specific cellular immunity in AIDS vaccine development. However, it is important to note that the current studies indicating the importance of Env variation as a determinant of vaccine efficacy do not preclude a role for Gag-specific immunity in protective vaccine immunity. In this regard, recent studies using attenuated simian immunodeficiency virus (SIV) or simian/human immunodeficiency virus (SHIV) immunizations in monkeys, followed by SHIV or SIV challenges, respectively, have indicated various levels of protection that are apparently independent of the variant Env in the challenge virus (45–48). Combining the results of vaccine studies in the different animal lentivirus models, we propose that the lentiviral Env serves as the primary determinant of vaccine efficacy to virus exposure and that Gag-specific responses are necessary but insufficient to provide optimal vaccine protection. This hypothesis can and should be rigorously tested in animal lentivirus and human AIDS vaccine studies.
Materials and Methods
Challenge Strains.
Viral stocks were prepared by harvesting the supernatant medium from equine dermal cells (CRL 6288; American Type Culture Collection, Manassas, VA) as described (31). Viral stock titers were determined by using our infectious center assay (cell-based ELISA) in fetal equine kidney cells, as described (50).
Experimental Subjects, Vaccination, and Challenge.
All equine procedures were conducted at the Gluck Equine Research Center of the University of Kentucky according to protocols approved by the University of Kentucky Institutional Animal Care and Use Committee (IACUC). Forty-two outbred ponies of mixed age and gender and serognegative for EIAV were used. Daily rectal temperatures and clinical status were recorded. Complete blood count analysis of whole blood was performed by using an IDEXX QBC Vet Autoreader. Hematocrit and platelet numbers were monitored weekly. The EIAVD9 stock was produced and vaccinations performed as described (23). Twenty-four vaccinated and 18 naïve ponies were challenged with 103 TCID50 of EV0, EV6, or EV13. The ponies were monitored daily for clinical symptoms of EIA, and blood was drawn at regular intervals (weekly, daily if febrile) for assays of platelets, viral replication, and virus-specific immune responses. During the course of these experiments, ponies that demonstrated severe disease-associated symptoms resulting in distress as outlined by the University of Kentucky IACUC were euthanized.
Immune Suppression and Delayed Type Hypersensitivity Analysis.
Dexamethasone (Phoenix Science, Kansas City, MO) was administered intramuscularly for 14 days at a dose of 0.11 mg/kg of body weight per day. The ponies were monitored daily by complete blood count and for physical signs of adverse reactions to drug treatment. Skin tests for delayed-type hypersensitivity (DTH) reactions were performed during the preimmune suppression and immune suppression periods. Skin test sites were prepared by shaving and cleaning small areas on the neck. The horses were intradermally administered (at different sites on the necks) both 50 μg of phytohemagglutinin (PHA) (Sigma, St. Louis, MO) in 1 ml of saline and 1 ml of saline alone. The net increase in skin thickness was determined from measurements made with constant tension calipers 24 h after injection of antigen. DTH ratios were calculated as the ratio of antigen (PHA) reaction to control (saline) reaction.
Quantitative and Qualitative RT-PCR Analysis of Plasma Virus RNA.
Plasma samples from all animals were analyzed for the levels of viral RNA per milliliter of plasma by using a previously described quantitative real-time multiplex RT-PCR assay based on gag-specific amplification primers (51). The standard RNA curve was linear in the range of 101 molecules as a lower limit and 108 molecules as an upper limit. To differentiate the virion genomic RNA of the EIAV vaccine strain from the challenge virus (EIAVPV), virion-associated genomic RNA was extracted from plasma samples and then characterized by a nested RT-PCR and restriction digestion analysis that differentiated parental and mutated S2 gene sequence. The nested RT-PCR is highly specific and provides detection levels down to 20 RNA copies of S2 (25). Analyses were confirmed by sequencing of the same PCR products. Diagnostic analyses were performed during all three periods of observation: before challenge, after challenge, and during immune suppression (if performed).
Quantitative Assays of Cellular Immune Responses.
Cryopreserved peripheral blood mononuclear cells (PBMCs) from the vaccinated animals were >80% viable upon thawing. Cell viability was maintained at >80% throughout the experiments. Assays are described in detail in Tagmyer et al. (52).
Lymphoproliferation.
PBMCs (2 × 105 cells per well) were assayed in six replicates by using pokeweed mitogen (PWM) and acetone-extracted EIAV (AE EIAV) as positive proliferative controls. The PBMCs were stimulated with Env peptide pools (20 μg/ml) for 6 days before labeling with 0.75uCi [3H]thymidine (1 Ci = 37 GBq). Cells were harvested and quantified for 3H incorporation by liquid scintillation counting. A positive response to the individual peptides was set at at least 2 times the naïve PBMC stimulation, SI >2.5.
Cytotoxic T lymphocyte-specific lysis.
PBMC were expanded for 7–10 days with either 2.5 μg/ml PWM or 10 μg/ml gradient purified EIAV. After expansion, stimulated cells were labeled with 100 μCi of [51Cr](Na51CrO). Cells were washed and plated (3 × 104 cells per well) before peptide pulsing with Env peptide pools (20 μg/ml). EIAV-stimulated effector cells were used at a 20:1 effector/target ratio. After the effector cell addition, the cells were incubated 12–16 h before being harvested, when 25 μl of cell supernatant was added to 175 μl of OptiPhase SuperMix scintillation fluid (Wallac, Loughborough, Leicestershire, U.K.) and analyzed with a MicroBeta reader (PerkinElmer, Wellesley, MA). Maximum 51Cr release was determined by plating target cells with the nonionic detergent Nonidet P-40. Background spontaneous lysis was determined by plating 51Cr-labeled target cells with 0.1 ml of medium alone.
Quantitative and Qualitative Serological Analyses.
Serum IgG antibody reactivity to EIAV envelope glycoproteins was assayed quantitatively (end point titer) and qualitatively (avidity index, conformation ratio) by using our standard Con A ELISA procedures as described (30). Virus-neutralizing activity to the challenge virus strain EIAVPV mediated by immune sera was assessed in an indirect cell–ELISA-based infectious center assay using a constant amount of infectious EIAVPV and sequential 2-fold dilutions of serum (30).
Statistical Analyses.
Associations of envelope divergence with vaccine-induced protection from disease and detectable infection were determined by using linear regression analysis (best fit, goodness of fit, and significance of a nonzero slope) as implemented in Prism version 4.0 (GraphPad, San Diego, CA).
Supplementary Material
Acknowledgments
We thank Dr. Richard Day for statistical assistance, Timothy J. Sturgeon for technical assistance, and Jonathan D. Steckbeck for helpful discussions and manuscript editing. This work was supported by National Institutes of Health/National Institute of Allergy and Infectious Diseases Grant R01 AI25850 (to J.K.C., S.B., T.L.T., B.Z., and R.C.M.) and by funds from the Lucille P. Markey Charitable Trust, and the University of Kentucky Agricultural Experiment Station (S.J.C. and C.J.I.).
Abbreviations
- EIAV
equine infectious anemia virus
- PBMC
peripheral blood mononuclear cell.
Footnotes
The authors declare no conflict of interest.
This article contains supporting information online at www.pnas.org/cgi/content/full/0706449104/DC1.
References
- 1.Gaschen B, Taylor J, Yusim K, Foley B, Gao F, Lang D, Novitsky V, Haynes B, Hahn BH, Bhattacharya T, Korber B. Science. 2002;296:2354–2360. doi: 10.1126/science.1070441. [DOI] [PubMed] [Google Scholar]
- 2.Anastassopoulou CG, Kostrikis LG. Curr HIV Res. 2006;4:365–373. doi: 10.2174/157016206777709456. [DOI] [PubMed] [Google Scholar]
- 3.Brander C, Frahm N, Walker BD. Curr Opin Immunol. 2006;18:430–437. doi: 10.1016/j.coi.2006.05.012. [DOI] [PubMed] [Google Scholar]
- 4.Korber B, Gaschen B, Yusim K, Thakallapally R, Kesmir C, Detours V. Br Med Bull. 2001;58:19–42. doi: 10.1093/bmb/58.1.19. [DOI] [PubMed] [Google Scholar]
- 5.Mullins JI, Jensen MA. Curr Top Microbiol Immunol. 2006;299:171–192. doi: 10.1007/3-540-26397-7_6. [DOI] [PubMed] [Google Scholar]
- 6.Jones NA, Wei X, Flower DR, Wong M, Michor F, Saag MS, Hahn BH, Nowak MA, Shaw GM, Borrow P. J Exp Med. 2004;200:1243–1256. doi: 10.1084/jem.20040511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lue J, Hsu M, Yang D, Marx P, Chen Z, Cheng-Mayer C. J Virol. 2002;76:10299–10306. doi: 10.1128/JVI.76.20.10299-10306.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wei X, Decker JM, Wang S, Hui H, Kappes JC, Wu X, Salazar-Gonzalez JF, Salazar MG, Kilby JM, Saag MS, et al. Nature. 2003;422:307–312. doi: 10.1038/nature01470. [DOI] [PubMed] [Google Scholar]
- 9.O'Connor DH, Allen TM, Watkins DI. DNA Cell Biol. 2002;21:659–664. doi: 10.1089/104454902760330192. [DOI] [PubMed] [Google Scholar]
- 10.Kusumi K, Conway B, Cunningham S, Berson A, Evans C, Iversen AK, Colvin D, Gallo MV, Coutre S, Shpaer EG. J Virol. 1992;66:875–885. doi: 10.1128/jvi.66.2.875-885.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.O'Connor D, Friedrich T, Hughes A, Allen TM, Watkins D. Immunol Rev. 2001;183:115–126. doi: 10.1034/j.1600-065x.2001.1830110.x. [DOI] [PubMed] [Google Scholar]
- 12.Rong R, Gnanakaran S, Decker JM, Bibollet-Ruche F, Taylor J, Sfakianos JN, Mokili JL, Muldoon M, Mulenga J, Allen S, et al. J Virol. 2007;81:5658–5668. doi: 10.1128/JVI.00257-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Howe L, Craigo JK, Issel CJ, Montelaro RC. J Gen Virol. 2005;86:139–149. doi: 10.1099/vir.0.80374-0. [DOI] [PubMed] [Google Scholar]
- 14.Howe L, Leroux C, Issel CJ, Montelaro RC. J Virol. 2002;76:10588. doi: 10.1128/JVI.76.21.10588-10597.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kinsey NE, Anderson MG, Unangst TJ, Joag SV, Narayan O, Zink MC, Clements JE. Virology. 1996;221:14–21. doi: 10.1006/viro.1996.0348. [DOI] [PubMed] [Google Scholar]
- 16.Johnson WE, Lifson JD, Lang SM, Johnson RP, Desrosiers RC. J Virol. 2003;77:375–381. doi: 10.1128/JVI.77.1.375-381.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dey B, Pancera M, Svehla K, Shu Y, Xiang S-H., Vainshtein J, Li Y, Sodroski J, Kwong PD, Mascola JR, Wyatt R. J Virol. 2007;81:5579–5593. doi: 10.1128/JVI.02500-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Brander C, Self S, Korber B. Curr Opin in HIV AIDS. 2007;2:183–188. doi: 10.1097/COH.0b013e3280f3bfe2. [DOI] [PubMed] [Google Scholar]
- 19.Montelaro RC, Ball JM, Rushlow K, Levy JA. The Retroviridae. Vol 2. New York: Plenum; 1993. pp. 257–360. [Google Scholar]
- 20.Harrold SM, Cook SJ, Cook RF, Rushlow KE, Issel CJ, Montelaro RC. J Virol. 2000;74:3112–3121. doi: 10.1128/jvi.74.7.3112-3121.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hammond SA, Li F, McKeon BM, Sr, Cook SJ, Issel CJ, Montelaro RC. J Virol. 2000;74:5968–5981. doi: 10.1128/jvi.74.13.5968-5981.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kono Y, Hirasawa K, Fukunaga Y, Taniguchi T. Nat Inst Anim Health Quart. 1976;16:8–15. [PubMed] [Google Scholar]
- 23.Craigo JK, Durkin S, Sturgeon TJ, Tagmyer T, Cook SJ, Issel CJ, Montelaro RC. Vaccine. 2007;25:834–845. doi: 10.1016/j.vaccine.2006.09.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Craigo JK, Li F, Steckbeck JD, Durkin S, Howe L, Cook SJ, Issel C, Montelaro RC. J Virol. 2005;79:2666–2677. doi: 10.1128/JVI.79.5.2666-2677.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li F, Craigo JK, Howe L, Steckbeck JD, Cook S, Issel C, Montelaro RC. J Virol. 2003;77:7244–7253. doi: 10.1128/JVI.77.13.7244-7253.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Montelaro RC, Wigzell H. AIDS. 1995;9(Suppl A):S111–S112. [PubMed] [Google Scholar]
- 27.Mills J, Desrosiers RC, Rud E, Almond N. AIDS Res Hum Retroviruses. 2000;16:1453–1461. doi: 10.1089/088922200750005976. [DOI] [PubMed] [Google Scholar]
- 28.Leroux C, Craigo JK, Issel CJ, Montelaro RC. J Virol. 2001;75:4570–4583. doi: 10.1128/JVI.75.10.4570-4583.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Craigo JK, Sturgeon TJ, Cook SJ, Issel CJ, Leroux C, Montelaro RC. Virology. 2006;344:340–353. doi: 10.1016/j.virol.2005.09.006. [DOI] [PubMed] [Google Scholar]
- 30.Hammond SA, Cook SJ, Lichtenstein DL, Issel CJ, Montelaro RC. J Virol. 1997;71:3840–3852. doi: 10.1128/jvi.71.5.3840-3852.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Li F, Puffer BA, Montelaro RC. J Virol. 1998;72:8344–8348. doi: 10.1128/jvi.72.10.8344-8348.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leroux C, Issel C, Montelaro RC. J Virol. 1997;71:9627–9639. doi: 10.1128/jvi.71.12.9627-9639.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Cook RF, Cook SJ, Berger SL, Leroux C, Ghabrial NN, Gantz M, Bolin PS, Mousel MR, Montelaro RC, Issel CJ. Virology. 2003;313:588–603. doi: 10.1016/s0042-6822(03)00351-9. [DOI] [PubMed] [Google Scholar]
- 34.Lichtenstein DL, Issel CJ, Montelaro RC. J Virol. 1996;70:3346–3354. doi: 10.1128/jvi.70.6.3346-3354.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Issel CJ, Horohov DW, Lea DF, Adams WV, Jr, Hagius SD, McManus JM, Allison AC, Montelaro RC. J Virol. 1992;66:3398–3408. doi: 10.1128/jvi.66.6.3398-3408.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Montelaro RC, Cole KS, Hammond SA. AIDS Res Hum Retroviruses. 1998;14(Suppl 3):S255–S259. [PubMed] [Google Scholar]
- 37.Craigo JK, Leroux C, Howe L, Steckbeck JD, Cook SJ, Issel CJ, Montelaro RC. J Gen Virol. 2002;83:1353–1359. doi: 10.1099/0022-1317-83-6-1353. [DOI] [PubMed] [Google Scholar]
- 38.Bogers WM, Cheng-Mayer C, Montelaro RC. AIDS. 2000;14:S141–S145. [PubMed] [Google Scholar]
- 39.Johnson RP. Nat Med. 1999;5:154–155. doi: 10.1038/5515. [DOI] [PubMed] [Google Scholar]
- 40.Johnson RP, Desrosiers RC. Curr Opin Immunol. 1998;10:436–443. doi: 10.1016/s0952-7915(98)80118-0. [DOI] [PubMed] [Google Scholar]
- 41.Blower SM, Koelle K, Kirschner DE, Mills J. Proc Natl Acad Sci USA. 2001;98:3618–3623. doi: 10.1073/pnas.061029998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Almond N, Stott J. Immunol Lett. 1999;66:167–170. doi: 10.1016/s0165-2478(98)00153-9. [DOI] [PubMed] [Google Scholar]
- 43.Shen RX, Wang Z. EIAV: A National Review of Policies, Programs, and Future Objectives. Amarillo, TX: American Quarterhorse Association; 1985. [Google Scholar]
- 44.Johnson RP, Lifson JD, Czajak SC, Cole KS, Manson KH, Glickman R, Yang J, Montefiori DC, Montelaro R, Wyand MS, Desrosiers RC. J Virol. 1999;73:4952–4961. doi: 10.1128/jvi.73.6.4952-4961.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kumar A, Mukherjee S, Shen J, Buch S, Li Z, Adany I, Liu Z, Zhuge W, Piatak M, Lifson JD, et al. Virology. 2002;301:189–205. doi: 10.1006/viro.2002.1544. [DOI] [PubMed] [Google Scholar]
- 46.Amara RR, Patel K, Niedziela G, Nigam P, Sharma S, Staprans SI, Montefiori DC, Chenareddi L, Herndon JG, Robinson HL, et al. J Virol. 2005;79:15356–15367. doi: 10.1128/JVI.79.24.15356-15367.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Busch M, Abel K, Li J, Piatak M, Jr, Lifson JD, Miller CJ. Vaccine. 2005;23:4036–4047. doi: 10.1016/j.vaccine.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 48.Abel K, Compton L, Rourke T, Montefiori D, Lu D, Rothaeusler K, Fritts L, Bost K, Miller CJ. J Virol. 2003;77:3099–3118. doi: 10.1128/JVI.77.5.3099-3118.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nickle DC, Jensen MA, Gottlieb GS, Shriner D, Learn GH, Rodrigo AG, Mullins JI. Science. 2003;299:1515–1518. doi: 10.1126/science.299.5612.1515c. and author reply, pp 1515–1518. [DOI] [PubMed] [Google Scholar]
- 50.Grund CH, Lechman ER, Issel CJ, Montelaro RC, Rushlow KE. J Gen Virol. 1994;75(pt 3):657–662. doi: 10.1099/0022-1317-75-3-657. [DOI] [PubMed] [Google Scholar]
- 51.Cook RF, Cook SJ, Li FL, Montelaro RC, Issel CJ. J Virol Methods. 2002;105:171–179. doi: 10.1016/s0166-0934(02)00101-5. [DOI] [PubMed] [Google Scholar]
- 52.Tagmyer TL, Craigo JK, Cook SJ, Issel CJ, Montelaro RC. J Gen Virol. 2007;88:1324–1336. doi: 10.1099/vir.0.82391-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.