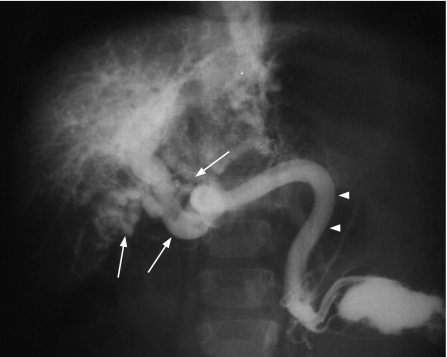
Extrahepatic portal venous obstruction (EHPVO) is a common cause of portal hypertension in the developing countries, and constitutes up to 40% of all patients with portal hypertension.1,2 EHPVO is a common cause of major upper‐gastrointestinal bleeding among children.2,3,4 The most common presentation in children is well‐tolerated variceal bleeding and splenomegaly. In adults, EHPVO is often recognised when evaluating for other disorders or with uncommon presentations such as jaundice, pruritus, acute cholecystitis‐like syndrome, ascites and so on, resulting from prolonged portal hypertension.5,6,7 The portal vein in EHPVO is transformed into a cavernoma, which is a bunch of multiple collateral veins around the obstructed portion of portal vein (fig 1). Marked improvements in the management of variceal bleeding in patients with EHPVO have resulted in an improved survival, thus presenting with unusual symptoms in adulthood.
Figure 1 Splenoportovenogram showing multiple collaterals (portal cavernoma) replacing the portal vein (arrows) in a patient with extrahepatic portal venous obstruction. The splenic vein is normal (arrowheads).
The reasons for EHPVO are obscure in approximately half of the patients. Omphalitis and intra‐abdominal sepsis are the common causes in neonates and children. Adults develop EHPVO due to increased blood coagulability, local inflammation, intra‐abdominal sepsis, myeloproliferative disorders, underlying cirrhosis, or tumours in the liver, bile ducts or pancreas.7,8,9,10
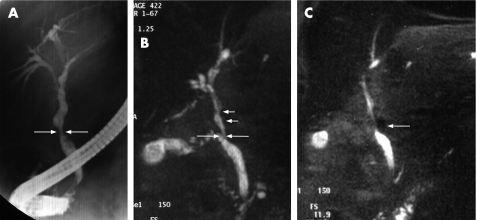
Gibson et al11 first reported the relationship between EHPVO and jaundice in 1965. Since then, several cases of obstructive jaundice due to common bile duct (CBD) obstruction caused by cavernomatous transformation of portal vein (portal cavernoma) have been described. Williams et al12 were the first to report cholangiographic changes caused by choledochal varices. We, for the first time, describe abnormalities on endoscopic retrograde cholangiography (ERC) in a prospective study.13 These abnormalities were similar to those of primary sclerosing cholangitis and the term “pseudosclerosing cholangitis” was then coined to describe them. However, unlike primary sclerosing cholangitis, biliary strictures in patients with EHPVO were smooth rather than irregular (figs 2, 3A). Since then, several case series have described biliary abnormalities among patients with portal hypertension on ERC.14,15,16,17,18,19,20,21,22
Figure 2 Endoscopic retrograde cholangiogram in a patient with extrahepatic portal venous obstruction showing irregular intrahepatic ducts and indentations of common hepatic and bile duct (arrows) arising due to compression by veins of the portal cavernoma.
Figure 3 (A) Endoscopic retrograde cholangiogram in a patient with extrahepatic portal venous obstruction showing irregular common hepatic and intrahepatic bile ducts with smooth narrowing of middle common bile duct (CBD; arrows). (B) Magnetic resonance (MR) cholangiography of the same patient showing narrowing of middle CBD (long arrows) with indentations above it (small arrows). (C) MR cholangiography also shows the close association between narrowing of CBD and a collateral vein (arrow) with dilatation of intrahepatic ducts.
Definition, nomenclature and frequency
The term “portal hypertensive biliopathy” (PHB) refers to abnormalities of the entire biliary tract including intrahepatic and extrahepatic bile ducts, cystic duct and gallbladder in patients with portal hypertension. Rarely, the cholangiographic appearances mimic bile duct cancer, with the cavernoma appearing as a solid tumour, the so‐called “pseudocholangiocarcinoma” sign.16 The same entity has also been variously termed as “portal biliopathy”,14 “cholangiopathy associated with portal hypertension”,18 and “portal cavernoma‐associated cholangiopathy”.20 As the entire or part of the biliary tract is involved in these patients, and most of these abnormalities are due to portal hypertension, we suggest renaming this entity as “portal hypertensive biliopathy”.22
Prospective studies have shown that between 81% and 100% of patients with EHPVO have PHB on ERC; however, only a small proportion of these individuals are with symptoms (table 1).13,14,15,16,17,18,19,20,21,22 PHB is not confined to patients with EHPVO, it has also been reported in patients with portal hypertension due to other causes such as cirrhosis of liver and idiopathic portal hypertension or non‐cirrhotic portal fibrosis, albeit with a lesser frequency.23 The frequency of PHB in patients with EHPVO (81–100%)13,14,15,16,17,18,19,20,21,22 is much greater than among patients with cirrhosis of liver (0–33%)17,18,24 or idiopathic portal hypertension (9–40%).18,24 This is most probably related to longstanding portal hypertension that results in the development of large collaterals in the biliary region with the formation of a typical portal cavernoma. This observation is further supported by a significantly higher frequency of anorectal varices, large oesophageal varices and variceal bleeding in patients with EHPVO compared with those having cirrhosis.25
Table 1 Frequency of biliary changes in patients with extrahepatic portal venous obstruction.
| Study | Year | n | Mean (SD) and/ or range age | M/F | Frequency of biliary changes (%)* | Patients with symptoms (%) |
|---|---|---|---|---|---|---|
| Dilawari and Chawla13 | 1992 | 20 | 22 (13–38) | 16/4 | 100 | 5 |
| Sarin et al14 | 1992 | 20 | 9–32 | 16/4 | 90 | 15 |
| Khuroo et al15 | 1993 | 21 | 14 (8.8) | 13/8 | 81 | 38 |
| Bayraktar et al16 | 1995 | 44 | 31.5 (9–67) | 24/20 | 94 | 30 |
| Malkan et al18 | 1999 | 20 | 23 | 12/8 | 85 | 10 |
| Nagi et al19 | 2000 | 43 | 14–45 | 25/18 | 100 | 19 |
| Condat et al20 | 2003 | 25 | 49.5 | 15/1 | 84 | 28 |
| Sezgin et al21 | 2003 | 36 | NA | NA | 94 | 10 |
| Dhiman et al22 | 2006 | 53 | 24.5 (13–56) | 36/17 | 100 | 24.5 |
| Total, median (range) | 262 | 94 (81–100) | 19 (5–38) |
F, female; M, male; NA, not available.
*Frequency reported on magnetic resonance cholangiography.
Aetiopathogenesis
The pathogenesis of PHB is not well known. It has been postulated that external pressure of portal cavernoma and/or ischaemia may play a role.15,20,26
There are two venous plexuses of bile ducts and gallbladder—namely, epicholedochal venous plexus of Saint27 and paracholedochal veins of Petren.28 The epicholedochal venous plexus of Saint, which is a fine reticular web on the outer surface of the CBD and hepatic ducts, becomes dilated and causes fine irregularities in the biliary tract.26,27 The paracholedochal venous plexus of Petren runs parallel to the CBD and is connected with the gastric, pancreaticoduodenal and portal veins, and to the liver directly; its dilatation causes extrinsic compression over CBD.26,28 The external pressure and protrusion of these venous collaterals over a thin and pliable CBD and common hepatic duct results in changes in PHB (figs 2, 3A–C).17,20,26,29 A recent magnetic resonance (MR) cholangiographic study coupled with MR portography demonstrated that the cholangiographic abnormalities resulted from impingement on the bile duct lumen by the veins comprising the cavernoma.20 Partial or complete resolution of these nodular extrinsic defects, narrowing, undulation and irregularity along the CBD on ERC have been reported among patients with portal hypertension after transjugular intrahepatic portosystemic shunt,30,31 and after shunt surgery.32,33
Histological and morphological studies have shown that cavernous transformation is not only dilatation of periportal collaterals but also neogenesis of vessels and formation of connective tissue occurring with increasing duration of thrombosis,34 which results in porous, tumour‐like solid tissue that does not disappear after shunt surgery.20,26,32 Biliary strictures resulting in biliary obstruction may be caused by ischaemia,26 or by encasement within a solid tumour‐like cavernoma.20 The mechanism of ischaemia resulting in bile duct damage in patients with EHPVO remains obscure. Venous damage, at the time of portal vein thrombosis, could predispose to ischaemic necrosis of bile ducts by compromising the vascular supply at the level of capillaries and the arterioles, which results in biliary stricture and cholangiectasis.35 The intrahepatic and extrahepatic segmental strictures and dilatations seen cholangiographically are similar to those seen in ischaemic cholangiography after liver transplantation.36 The rigidity of strictures observed by us, and also by others, also supports the ischaemic aetiology.37
In a prospective study, we evaluated the relationship of biliary changes with portal cavernoma using MR cholangiography coupled with MR portography in 18 patients with EHPVO.29 Dominant stricture of the bile duct was seen in nine patients; only five (55%) of them were caused by compression from adjacent collaterals and no such relationship was seen in the remaining four (44%); and hence, ischaemic aetiology was presumed.
Thus, with whatever limited data that are available to date, PHB is caused due to pressure on the bile ducts from collaterals and ischaemic injury to bile ducts during portal vein thrombosis; the two mechanisms are not mutually exclusive.26
Clinical features
Although biliary abnormalities are seen in most of patients with EHPVO, a majority of them are asymptomatic and a few present with symptoms such as jaundice, pruritus, fever or pain in abdomen. There are two types of clinical features: (1) those related to chronic cholestasis, probably explained by strictures caused by either compression of the biliary lumen by the enlarged collaterals or by ischaemia and (2) those related to biliary stones, which are probably responsible for biliary pain and cholangitis. This condition is rarely recognised at laparotomy and usually requires management of biliary obstruction, which is indeed challenging.
Clinical presentation
Asymptomatic
No biliary symptoms despite the presence of biliary abnormalities on endoscopic retrograde cholangiography or magnetic resonance cholangiography.
With symptoms
Chronic cholestasis, likely to be caused by biliary stricture.
Biliary pain or acute cholangitis, likely to be caused by biliary stones.
Dilawari and Chawla13 noted biliary colic in only one (5%) of the 20 patients with PHB due to a CBD stone. Sarin et al14 reported jaundice in three (15%) of the 20 patients; six (30%) patients had elevated serum alkaline phosphatase and four (20%) had CBD stones. Khuroo et al15 found symptoms of PHB in 8 of 21 (38%) patients, seven of whom had jaundice and one had recurrent cholangitis. All patients with symptoms were adults. Malkan et al18 noted obstructive jaundice in two of 20 (10%) patients with PHB, whereas Nagi et al19 reported it in eight of 43 (18.6%) patients. Condat et al20 reported symptoms of PHB in seven of 25 (28%) adult patients with EHPVO, which included biliary colic in two (8%), jaundice in four (16%), cholangitis in two (8%), acalculous cholecystitis in one (4%), CBD stones in two (8%) and cholelithiasis in one (4%) patient. Sezgin et al21 found that 10% of their patients with PHB had symptoms (table 1).
Our recent study on 53 patients with EHPVO showed that 13 (24.5%) of them had biliary symptoms that included abdominal pain in 10 (18.9%), jaundice in 9 (17%), fever in two (15%) and cholangitis in three (23%).22 Symptoms of PHB were associated with higher age, longer duration of disease, higher frequency of CBD and gallbladder stones, and abnormal liver function tests when compared with asymptomatic patients (table 2).22 Sezgin et al21 showed a median age of 39 years in patients with EHPVO who presented with biliary symptoms. This is in contrast with the usual presentation of such patients with variceal bleeding in the first two decades of life.1,2,3
Table 2 Asymptomatic versus symptomatic portal hypertensive biliopathy22.
| Asymptomatic | Symptomatic | p Value | |
|---|---|---|---|
| n (%) | 40 (75.5%) | 13 (24.5%) | — |
| Median (range) age (years) | 21 (13–34) | 35 (17–56) | <0.001 |
| Male: female | 29:11 | 7:6 | NS |
| Median (range) duration of EHPVO since diagnosis (years) | 4 (1–19) | 11 (1–23) | <0.022 |
| Median (range) duration of symptom (months) | — | 11 (0.5–96) | — |
| Gallstones | 0 (0%) | 7 (54%) | <0.001 |
| Median (range) bilirubin level (mg/dl) | 0.8 (0.4–3.9) | 2.7 (0.7–16) | <0.001 |
| Median (range) alkaline phosphatase level (IU/l)* | 94 (70–194) | 398 (97–1080) | <0.001 |
| ERC | |||
| Biliary stricture | 14 (35%) | 6 (46%) | NS |
| Biliary dilatation | 8 (20%) | 6 (46%) | 0.08 |
| Indentations | 20 (50%) | 5 (39%) | NS |
| CBD stones | 1 (2.5%) | 3 (23%) | 0.042 |
| Choledochal varices | 3 (7.5%) | 1 (7.7%) | NS |
CBD, common bile duct; EHPVO, extrahepatic portal venous obstruction; ERC, endoscopic retrograde cholangiography; NS, nonsignificant.
*Normal value, 70–140 IU/l.
Choledocholithiasis could result from biliary stasis due to biliary strictures. However, not all patients with PHB develop choledocholithiasis because of normal and pliable CBD walls or a relatively mild degree of luminal narrowing causing little stasis.38 Moreover, biliary abnormalities are patchy, which may allow the bile to flow through unaffected biliary ducts. Thus patients with asymptomatic or non‐obstructive PHB may not have a critical level of extrahepatic biliary obstruction resulting in abnormal emptying of gallbladder and bile lithogenicity.39
Hepatic dysfunction in the form of ascites, low serum albumin and prolonged prothrombin time have been reported in patients with EHPVO and, more so, in patients with prolonged portal hypertension.5,6 Development of ascites and derangements in liver function tests occurred with increasing age and increasing duration of disease. Symptoms of PHB therefore seem to be a late complication of EHPVO and is progressive in nature leading to clinical and biochemical evidence of liver dysfunction.
Imaging
Endoscopic retrograde cholangiography
ERC has been the most important investigation, which has helped in recognising this entity (figs 2, 3A). Typical cholangiographic findings are well described, and biliary intervention can be attempted to relieve biliary obstruction (table 3). Biliary abnormalities include smooth strictures of various lengths and degrees, calibre irregularity, segmental upstream dilatation, ectasia, indentations, displacement and angulations of ducts, clustering of intrahepatic ducts and pruning of intrahepatic ducts. Left hepatic duct abnormalities are common and could be seen in 55–100% of patients. Right hepatic duct is involved in 40–56% of patients with less severe abnormalities than those with left hepatic duct involvement (table 3). The reasons why left hepatic duct is more commonly involved are unclear, but it could be related to the formation of prominent collateral veins where the umbilical vein joins the left branch of the portal vein or may be related to suboptimal filling of right hepatic duct by the contrast during ERC.40 Patients with cirrhosis and idiopathic portal hypertension predominantly have intrahepatic abnormalities, whereas those with EHPVO have both intrahepatic and extrahepatic abnormalities.18
Table 3 Biliary abnormalities on endoscopic retrograde cholangiography.
| Dilawari and Chawla13 (n = 20) | Sarin et al14 (n = 20) | Khuroo et al15 (n = 21) | Malkan et al18 (n = 20) | Nagi et al19 (n = 43) | Dhiman et al22 (n = 53) | |
|---|---|---|---|---|---|---|
| Abnormal cholangraphy | 20 (100) | 18 (90) | 17 (81) | 17 (85) | 40 (93) | 53 (100) |
| Extrahepatic duct | 18 (90) | 18 (90) | 14 (66.7) | 12 (60) | 40 (93) | 51 (96) |
| Left hepatic duct | 20 (100) | 16 (80) | 8 (38.1) | 11 (55) | 23 (53.5) | 41 (77) |
| Right hepatic duct | 11 (56) | 10 (50) | 8 (40) | 23 (43) | ||
| Extrahepatic strictures | 5 (25) | 5 (25) | 11 (52.4) | 9 (45) | + | 20 (38) |
| Intrahepatic biliary radicle dilatation | 0 (0) | 0 (0) | 9 (42.8) | 5 (25) | 2 | 14 (26) |
| Indentations | 13 (65 ) | 6 (30) | 3 (14.3) | + | 24 (55.8) | 31 (58) |
| Calibre irregularities | + | 12 (60) | 5 (23.8) | + | 23 (70)* | |
| Angulations | — | — | 1 (4.7) | 1 (5) | + | 2 (6)†* |
| Ectasias | — | — | 2 (9.5) | + | — | 10 (30)* |
| CBD stones | 1 (5) | 3 (15) | 0 (0) | 2 (10) | – | 3 (6) |
| Multiple filling defects in extrahepatic and/or intrahepatic ducts (choledochal varices) | — | — | — | — | + | 4 (8) |
CBD, common bile duct.
All values are given as n (%).
*n = 30.
+ present.
− not reported.
Irregular cystic duct and gall bladder margins may be seen in a few patients. Multiple filling defects may be seen within the CBD or within the intrahepatic ducts. These are due to stones or choledochal varices.19,22,40
MR cholangiography and portography
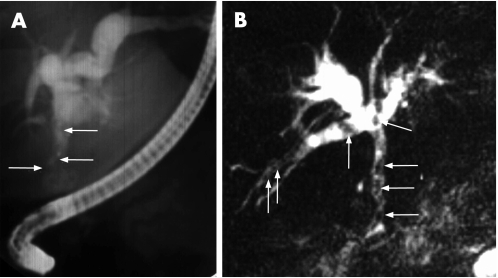
MR cholangiography and portography is non‐invasive and can demonstrate bile duct changes and portal collaterals simultaneously (figs 3 and 4). In our experience, MR cholangiography is as useful as ERC in detecting biliary abnormalities in patients with EHPVO, but MR cholangiography with MR portography is superior to ERC in delineating changes in intrahepatic biliary ducts and in differentiating choledochal varices from CBD stones (fig 4).40 In addition, MR portography also delineates the entire splenoportovenous axis and portal collaterals, which helps to assess the possibility of shunt surgery. Condat et al20 have also demonstrated that the findings of MR cholangiography are similar to those seen on ERC. The latter, is a semi‐invasive procedure and could lead to complications, and its use should be restricted to patients with symptoms of PHB necessitating therapeutic intervention. Therefore, MR cholangiography with MR portography should be the initial investigation of choice in the evaluation of PHB.
Figure 4 (A) Endoscopic retrograde cholangiogram showing filling defects in the common bile duct suggestive of stones along with dilatation of intrahepatic biliary ducts. (B) Magnetic resonance cholangiography in the same patient revealed multiple circular or oval and longitudinal filling defects, owing to choledochal varices in both the intrahepatic and extrahepatic biliary system (arrows), with dilatation of intrahepatic hepatic biliary ducts.
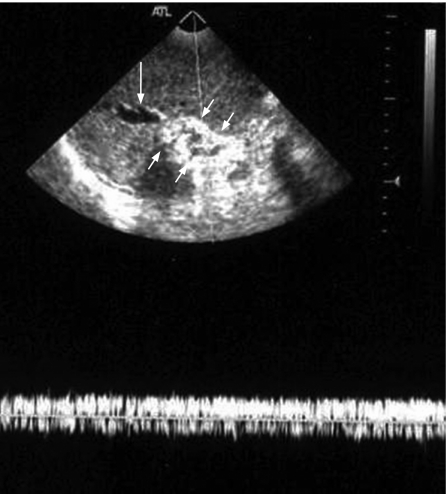
Ultrasonography
Ultrasonography plays a minor role as the CBD could be obscured by high‐level echoes in the porta hepatis and multiple collaterals (anechoic tubular structures) may conceal the bile duct. However, it is reliable in showing the dilated intrahepatic biliary system (fig 5). Although ERC delineates the biliary ductal changes, ultrasonography provides additional information related to the presence of gallbladder varices. Gallbladder varices were observed in 30–55% of patients with EHPVO, which appear as tortuous, dilated vessels in or around the wall of the gallbladder or in the bed of the gallbladder fossa.18,41 Gallbladder varices reduce distensibilty of the gallbladder, thus resulting in reduced fasting gallbladder volume, although they do not cause alteration in the emptying of gallbladder and bile lithogenicity.39
Figure 5 Ultrasonography of liver showing portal cavernoma formed by collateral veins (as shown by positive Doppler signal for blood flow) encased in fibrous tissue (small arrows) and dilated intrahepatic biliary ducts (long arrow).
Radiodiagnostic examination
-
Endoscopic retrograde cholangiography (ERC)
-
-
Key investigation for delineating biliary changes; endotherapy is possible
-
-
-
Magnetic resonance (MR) cholangiography and MR portovenograpy
-
-
Initial investigation of choice, as accurate as ERC in delineating biliary changes, demonstrates relationship of biliary changes with collaterals and the presence of shuntable vein; helps distinguish between bile duct varices and common bile duct stones
-
-
-
Ultrasonography
-
-
Minor role; may demonstrate the level of biliary obstruction
-
-
-
Endoscopic ultrasonography
-
-
Useful when other imaging modalities are unrevealing or inconclusive in delineating the cause of biliary obstruction
-
-
Endoscopic ultrasonography
Endoscopic ultrasonography (EUS) could also be useful in identifying CBD varices and/or bile duct stones. Palazzo et al42 described endosonographic features of biliary varices in 21 patients with EHPVO. EUS identified biliary varices in the wall of CBD in 16 (76%) patients, surrounding it in 11 (52%) and in the gallbladder in nine (43%). These varices resulted in obstructive jaundice in three of the 21 (14%) patients, but only when located in the wall of the CBD. Umphress et al43 have described a patient with obstructive jaundice related to portal vein thrombosis in whom the diagnosis was made by EUS and Doppler that demonstrated venous collaterals surrounding the bile duct. These vessels may be too small to be detected by other imaging modalities.
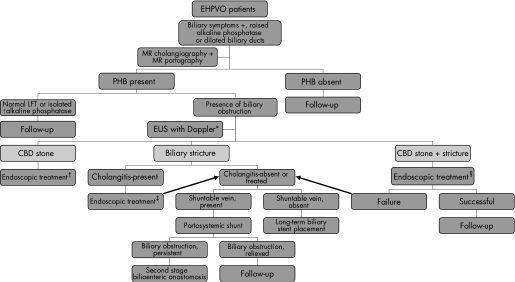
EUS with Doppler should, therefore, be incorporated in the diagnostic scheme of these patients as it may provide additional useful extrahepatic bile duct information, especially the cause of biliary obstruction—that is, bile duct varices, stones, sludge, strictures or a tumour, when other imaging modalities are unrevealing (fig 6).
Figure 6 Algorithm for the management of a patient with portal hypertensive biliopathy. CBD, common bile duct; EHPVO, extrahepatic portal venous obstruction; EUS, endoscopic ultrasonography LFT, liver function tests; MR, magnetic resonance; PHB, portal hypertensive biliopathy. *EUS with Doppler for evaluation of biliary obstruction when other imaging modalities are unrevealing; †endoscopic treatment includes endoscopic sphincterotomy, stone extraction with or without the help of mechanical lithotripsy; ‡endoscopic treatment includes nasobiliary drain or biliary stent placement; §endoscopic treatment includes endoscopic sphincterotomy and stricture dilatation, followed by stone extraction with or without the help of mechanical lithotripsy.
Treatment
There is no consensus regarding optimal treatment of this condition, as data regarding various forms of therapy are inconclusive. Asymptomatic patients with PHB do not require any treatment. Treatment of symptoms of PHB should be determined by the individual patient's characteristics. It should be focused on the management of portal hypertension and relief of obstructive jaundice.
The data regarding management in this review are based on the short series and personal experience.
Endoscopic treatment
Endoscopic treatment includes endoscopic sphincterotomy, stone extraction, mechanical lithotripsy and biliary stricture dilatation with or without stent or nasobiliary drain placement. Endoscopic sphincterotomy with extraction of CBD stones is the treatment of choice in patients with CBD stones.33,38,44 Temporary or permanent endoscopic biliary stenting has been used in such patients to alleviate biliary symptoms.45,46,47,48 Stents or nasobiliary drains relieve the biliary obstruction and cholangitis, but are likely to be blocked frequently.21,45,48 Management of patients with CBD stones and coexistent stricture is challenging and could require an aggressive approach.26,44 Most of these patients can be successfully treated by endoscopic sphincterotomy and stricture dilatation followed by stone extraction; some of them may also require mechanical lithotripsy for breaking the stones into smaller pieces.44 Bleeding from bile duct varices (haemobilia) during biliary dilatation may also occur.49,50 A cautious approach when performing sphincterotomy has to be advocated, as venous collaterals in ampullary and juxtapapillary region could be present, which may result in an increased risk of bleeding during the procedure. Filling defects within the biliary system could be due to stones or choledochal varices; the latter needs to be identified so as to avoid severe bleeding after the use of Dormia basket for a mistaken stone.21,40 The filling defects caused by choledochal varices do not move with the balloon catheter or with open Dormia basket during ERC and may appear as longitudinal filling defects on MR cholangiography (fig 4).22,40 We prefer to use balloon catheter over Dormia basket for removing CBD stones after the endoscopic sphincterotomy to minimise the risk of haemobilia.
Sezgin et al21 reported 10 patients with CBD stricture with or without CBD stones (n = 4) or cholangitis (n = 5). The strictures were 1–5 cm long with smooth margins. Endoscopic treatment included endoscopic sphincterotomy and nasobiliary drain or stent in all (7 Fr or 10 Fr), balloon dilatation in four patients and stone extraction in four patients. On a median follow‐up of 2.75 (range 1–7) years, one death occurred after 2.5 years from secondary biliary cirrhosis. The rest of the patients were asymptomatic with or without stent in situ. Long‐term biliary drainage with significant improvement in the cholangiographic appearance of stricture was achieved in three (30%) patients. In the other seven (70%) patients, stents had to be left in place as the biliary drainage was inadequate. These patients had undergone a scheduled stent exchange every 6 months, unless stent occlusion or cholangitis warranted an early stent replacement. Dumortier et al51 described failure of prolonged endoscopic treatment in four patients, second‐line portosystemic shunt surgery allowed removal of the biliary stent and no recurrence of disease was reported.
Surgical treatment
Bilioenteric anastomosis of biliary obstruction is associated with a high morbidity and mortality as the collateral vessels around the bile ducts make the surgical dissection difficult, which if injured may result in excess haemorrhage and death.33,34,37 Thus, these patients should undergo portosystemic shunt surgery before any bilioenteric anastomosis is planned. A large proportion of these individuals improve with shunt surgery and may not require further surgical intervention.5,26,32,52,53,54 Chaudhary et al32 treated eight patients with EHPVO with symptoms of PHB. Portosystemic shunting relieved jaundice in five of seven patients, whereas in two patients a second‐stage hepaticojejunostomy was required. Thus, symptoms of biliary obstruction in patients with extrahepatic portal hypertension may be relieved by a portosystemic shunt; rarely, biliary bypass may be required. Shunt surgery may also be indicated if these patients have bled and have evidence of hypersplenism resulting in significant anaemia and/or thrombocytopenia. Transjugular intrahepatic portosystemic shunt also reverses the biliary changes in these patients, thus, it may be useful in select patients.30,31 In patients with an intractable disease, liver transplantation could be the only option when both endoscopic and surgical treatments have either failed or are not feasible.55
We treated 12 patients with EHPVO (6 men, median age 34 years) and biliary obstruction over a period of 10 years.44 ERC revealed dominant biliary strictures in seven patients, CBD stones in five (with strictures in three), choledochal varices in two and Mirizzi's syndrome in one. Among the patients with dominant biliary structures, we performed portosystemic shunt surgery, mesocaval in four and side to side leinorenal in one; the remaining two patients and two patients with choledochal varices without a shuntable vein underwent long‐term repeated endoscopic biliary stent placements. CBD stones were safely removed after endoscopic sphincterotomy with or without biliary stricture dilatation. Mirizzi's syndrome was managed by biliary stenting followed by surgical removal of stone; CBD wall was repaired with a flap from gallbladder. These patients remained asymptomatic after median (range) follow‐up of 19 (range 6–132) months.
Endoscopic treatment should be the preferred treatment for patients with CBD stones, cholangitis or for patients with dominant biliary stricture, but without a shuntable vein. Patients with CBD stones and coexistent stricture should be treated with endoscopic sphincterotomy, stricture dilatation and stone extraction with or without the help of mechanical lithotripsy.
We prefer surgical treatment to the endoscopic treatment for dominant biliary strictures with a shuntable vein as it is a proven treatment that provides long‐lasting relief of symptoms in a young patient with an otherwise normal life expectancy. In patients who undergo endoscopic stent placement, there is also a risk of development of secondary biliary cirrhosis because of incomplete relief of biliary obstruction due to recurrent stent blockage with or without cholangitis.21 Endoscopic treatment in these patients requires scheduled biliary stent exchange every 4–6 months or earlier, if the stents get blocked or the patient develops cholangitis. Surgical treatment is also preferable in patients who live at far‐off places and do not have access to tertiary care centre for endoscopic treatment.
Patients with symptomatic gallstones in an otherwise asymptomatic PHB should be managed preferably by portosystemic shunt surgery followed by cholecystectomy. However, if no shuntable vein is available, minimum surgical intervention should be done to avoid severe bleeding. Vasoactive agents such as somatostatin, octreotide or terlipressin are known to reduce portal pressure in patients with portal hypertension; their infusion during biliary surgery in patients without prior shunt surgery may be useful to decrease blood loss.56,57
An algorithmic approach for the detection and management of PHB is presented (fig 6).
Key points
Portal hypertensive biliopathy (PHB) is the late complication of portal hypertension and is more commonly seen in patients with extrahepatic portal venous obstruction than in patients with cirrhosis or idiopathic portal hypertension.
External pressure over the bile ducts from biliary collaterals and/or ischaemic injury of bile ducts during portal vein thrombosis seems to be the main mechanism responsible for the development of PHB.
Approximately 20% of patients are with symptoms, which is associated with higher age, longer duration of disease, higher frequency of common bile duct (CBD) stones and gallbladder stones, and abnormal liver function tests.
Magnetic resonance (MR) cholangiography and MR portovenography is the initial investigation of choice.
Treatment of symptoms of PHB should be aimed at the management of portal hypertension and relief of obstructive jaundice.
Endotherapy is the preferred treatment for patients with CBD stones, cholangitis or patients with dominant biliary stricture, but without a shuntable vein.
Portosystemic shunt should be performed in patients with dominant biliary strictures with a shuntable vein. Rarely, second stage biliary bypass may be required.
Liver transplantation may be required for intractable and advanced disease.
Summary
PHB refers to the biliary abnormalities observed among patients with portal hypertension on ERC or MR cholangiography. The changes are more common and pronounced in patients with EHPVO than in patients with idiopathic portal hypertension or cirrhosis of liver. Although majority of patients are asymptomatic, approximately one‐fifth of these patients are with symptoms and present with biliary symptoms, such as pain in upper abdomen pain, jaundice, fever and so on. The aetiopathogenesis of PHB is not well known and it has been postulated that external pressure by dilated veins of portal cavernoma and/or ischaemic strictures of the bile duct may play a role. MR cholangiography with MR portography should be the initial investigation of choice in the evaluation of PHB. EUS with Doppler is evolving and could provide, additional, useful extrahepatic bile duct information, especially on the cause of biliary obstruction. Therefore, it may be incorporated in the diagnostic examination of these patients. Asymptomatic patients with PHB do not require any treatment. The treatment of PHB is either endoscopic (CBD stone extraction, biliary stenting or nasobiliary drainage) or surgical (definitive decompressive shunt surgery followed by bilioenteric anastomosis, if necessary). Both forms of treatment are not mutually exclusive but, at times, are complementary.
Footnotes
Competing interests: None.
References
- 1.Dilawari J B, Chawla Y K. Extrahepatic portal venous obstruction. Gut 198829554–555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Anand C S, Tandon B N, Nundy S. The causes, management and outcome of upper gastrointestinal hemorrhage in an Indian hospital. Br J Surg 198370209–211. [DOI] [PubMed] [Google Scholar]
- 3.Chawla Y K, Dilawari J B, Ramesh G N.et al Sclerotherapy in extrahepatic portal venous obstruction. Gut 199031213–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitra S K, Kumar V, Dutta D V.et al Extrahepatic portal hypertension: a review of 70 cases. J Pediatr Surg 19781351–57. [DOI] [PubMed] [Google Scholar]
- 5.Webb L J, Sherlock S. The aetiology, presentation and natural history of extra hepatic portal venous obstruction. Q J Med 197948627–639. [PubMed] [Google Scholar]
- 6.Rangari M, Gupta R, Jain M.et al Hepatic dysfunction in patients with extrahepatic portal vein obstruction. Liver Int 200323434–437. [DOI] [PubMed] [Google Scholar]
- 7.Sarin S K, Agarwal S R. Extrahepatic portal vein obstruction. Semin Liver Dis 20022243–58. [DOI] [PubMed] [Google Scholar]
- 8.Amitrano L, Brancaccio V, Guardascione M A.et al Inherited coagulation disorders in cirrhotic patients with portal vein thrombosis. Hepatology 200031345–348. [DOI] [PubMed] [Google Scholar]
- 9.Condat B, Pessione F, Denninger M H.et al Recent portal or mesenteric venous thrombosis: increased recognition and frequent recannalization on anticoagulation therapy. Hepatology 200032466–470. [DOI] [PubMed] [Google Scholar]
- 10.Valla D ‐ C, Condat B, Lebrec D. Spectrum of portal vein thrombosis in the West. J Gastroenterol Hepatol 200217S224–S227. [DOI] [PubMed] [Google Scholar]
- 11.Gibson J B, Johnston G W, Fulton T T.et al Extrahepatic portal venous obstruction. Br J Surg 196552129–139. [DOI] [PubMed] [Google Scholar]
- 12.Williams S M, Burnett D A, Mazer M U. Radiographic demonstration of common bile duct varices. Gastrointest Radiol 1982769–70. [DOI] [PubMed] [Google Scholar]
- 13.Dilawari J B, Chawla Y K. Pseudosclerosing cholangitis in extrahepatic portal venous obstruction. Gut 199233272–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sarin S K, Bhatia V, Makwana U. Poratal biliopathy in extrahepatic portal venous obstruction [abstract]. Indian J Gastroenterol 199211(Suppl 1)A82 [Google Scholar]
- 15.Khuroo M S, Yatoo G N, Zargar S A.et al Biliary abnormalities associated with extrahepatic portal venous obstruction. Hepatology 199317807–813. [PubMed] [Google Scholar]
- 16.Bayraktar Y, Balkanci F, Kayhan B.et al Bile duct varices or “pseudo‐cholangiocarcinoma sign” in portal hypertension due to cavernous transformation of the portal vein. Am J Gastroenterol 1992871801–1806. [PubMed] [Google Scholar]
- 17.Bayraktar Y, Balkanci F, Ozenc A.et al The “pseudo‐cholangiocarcinoma sign” in patients with cavernous transformation of the portal vein and its effect on the serum alkaline phosphatase and bilirubin levels. Am J Gastroenterol 1995902015–2019. [PubMed] [Google Scholar]
- 18.Malkan G H, Bhatia S J, Bashir K.et al Cholangiopathy associated with portal hypertension: diagnostic evaluation and clinical implications. Gastrointest Endosc 199949344–348. [DOI] [PubMed] [Google Scholar]
- 19.Nagi B, Kochhar R, Bhasin D.et al Cholangiopathy in extrahepatic portal venous obstruction. Radiological appearances. Acta Radiol 200041612–615. [DOI] [PubMed] [Google Scholar]
- 20.Condat B, Vilgrain V, Asselah T.et al Portal cavernoma associated cholangiopathy: a clinical and MR cholangiography coupled with MR portography imaging study. Hepatology 2003371302–1308. [DOI] [PubMed] [Google Scholar]
- 21.Sezgin O, Oguz D, Attintas E.et al Endoscopic management of biliary obstruction caused by cavernous transformation of the portal vein. Gastrointest Endosc 200368602–608. [DOI] [PubMed] [Google Scholar]
- 22.Dhiman R K, Chawla Y, Duseja A.et al Portal hypertensive biliopathy (PHB) in patients with extrahepatic portal venous obstruction (EHPVO) [abstract]. J Gastroenterol Hepatol 200621A504 [Google Scholar]
- 23.Dhiman R K, Chawla Y, Vasishta R K.et al Non‐cirrhotic portal fibrosis (idiopathic portal hypertension): experience with 151 patients and a review of the literature. J Gastroenterol Hepatol 2002176–16. [DOI] [PubMed] [Google Scholar]
- 24.Chandra R, Kapoor D, Tharakan A.et al Portal biliopathy. J Gastroenterol Hepatol 2001161086–1092. [DOI] [PubMed] [Google Scholar]
- 25.Chawla Y, Dilawari J B. Anorectal varices: their frequency in cirrhotic and noncirrhotic portal hypertension. Gut 199132309–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dhiman R K, Puri P, Chawla Y.et al Biliary changes in extrahepatic portal venous obstruction: compression by collaterals or ischemic. Gastrointest Endosc 199950646–652. [DOI] [PubMed] [Google Scholar]
- 27.Saint O A. The epicholedochal venous plexus and its importance as a mean of identifying the common bile duct during operations on extrahepatic biliary tract. Br J Surg 197146489–498. [DOI] [PubMed] [Google Scholar]
- 28.Petren T. Die extrahepatischen Gallenwegsvenen and ihre. Pathologischanatomische Bedeutum. Verh Anat Ges 193241139–143. [Google Scholar]
- 29.Dhiman R K, Singh P, Duseja A.et al Pathogenesis of portal hypertensive biliopathy (PHB): is it compression by collaterals or ischemia? [abstract] J Gastroenterol Hepatol200621A506 [Google Scholar]
- 30.Gorgul A, Kayhan B, Dogan I.et al Disappearance of pseudocholangiocarcinoma sign after TIPSS. Am J Gastroenterol 199691150–154. [PubMed] [Google Scholar]
- 31.Bayraktar Y, Ozturk M A, Egesel T.et al Disappearance of “pseudocholangiocarcinoma sign” in a patient with portal hypertension due to complete thrombosis of left portal vein and main portal vein web after web dilatation and transjugular and intrahepatic portosystemic shunt. J Clin Gastroenterol 200031328–332. [DOI] [PubMed] [Google Scholar]
- 32.Chaudhary A, Dhar P, Sachdev A.et al Bile duct obstruction due to portal biliopathy in extrahepatic portal hypertension: surgical management. Br J Surg 199885326–329. [DOI] [PubMed] [Google Scholar]
- 33.Khare R, Sikora S S, Srikanth G.et al Exrahepatic portal venous obstruction and obstructive jaundice: approach to management. J Gastroenterol Hepatol 20052056–61. [DOI] [PubMed] [Google Scholar]
- 34.Bechtelsheimer H, Conrad A. Morphologisches Bild der Kavernosen Transformation der Pfortader. Leber Magen Darm 1980299–106. [PubMed] [Google Scholar]
- 35.Batts K P. Ischemic cholangitis. Mayo Clin Proc 199873380–385. [DOI] [PubMed] [Google Scholar]
- 36.Cameron A M, Busuttil R W. Ischemic cholangiopathy after liver transplantation. Hepatobiliary Pancreat Dis Int 20054495–501. [PubMed] [Google Scholar]
- 37.Mork H, Weber P, Schmidt H, Goerig R M.et al Cavernomatous transformation of the portal vein associated with common bile duct strictures: report of two cases. Gastrointest Endosc 19984779–83. [DOI] [PubMed] [Google Scholar]
- 38.Bhatia V, Jain A K, Sarin S K. Choledocholithiasis associated with portal biliopathy in patients with extrahepatic portal vein obstruction. Management with endoscopic sphincterotomy. Gastrointest Endosc 199542178–181. [DOI] [PubMed] [Google Scholar]
- 39.Dhiman R K, Lawrence A, Sharma A.et al Effect of portal biliopathy and gallbladder varices on gallbladder motility and bile lithogenicity in patients with extrahepatic portal venous obstruction [abstract]. J Gastroenterol Hepatol 200419A736 [Google Scholar]
- 40.Dhiman R K, Singh P, Behera A.et al Diagnosis of portal hypertensive biliopathy (PHB) in patients with extrahepatic portal venous obstruction (EHPVO): endoscopic retrograde cholangiography versus MR cholangiography [abstract]. J Gastroenterol Hepatol 200621A507 [Google Scholar]
- 41.Chawla Y, Dilawari J B, Kataria S. Gallbladder varices in portal vein thrombosis. Am J Roentgenol 1994162643–645. [DOI] [PubMed] [Google Scholar]
- 42.Palazzo L, Hochain P, Helmer C.et al Biliary varices on endoscopic ultrasonography. Endoscopy 200032520–524. [DOI] [PubMed] [Google Scholar]
- 43.Umphress J L, Pecha R E, Urayama S. Biliary stricture caused by portal biliopathy: diagnosis by EUS with Doppler US. Gastrointest Endosc 2004601021–1024. [DOI] [PubMed] [Google Scholar]
- 44.Dhiman R K, Chhetri D, Behera A.et al Management of biliary obstruction in patients with portal hypertensive biliopathy (PHB) [abstract]. J Gastroenterol Hepatol 200621A505 [Google Scholar]
- 45.Lohr J M, Kuchenreuter S, Grebmeier H.et al Compression of the common bile duct due to portal vein thrombosis in polycythemia vera. Hepatology 199317586–592. [DOI] [PubMed] [Google Scholar]
- 46.Thervet L, Faulques B, Pissas A.et al Endoscopic management of obstructive jaundice due to portal cavernoma. Endoscopy 199325423–425. [DOI] [PubMed] [Google Scholar]
- 47.Mercado‐Diaz M A, Hinojosa C A, Chan C.et al Portal biliopathy. Rev Gastroenterol Mex 20046937–41. [PubMed] [Google Scholar]
- 48.Solmi L, Rossi A, Conigliaro R.et al Endoscopic treatment of a case of obstructive jaundice secondary to portal cavernoma. Ital J Gastroenterol Hepatol 199830202–204. [PubMed] [Google Scholar]
- 49.Tighe M, Jacobson I. Bleeding from bile duct varices as unexpected hazard during therapeutic ERCP. Gastrointest Endosc 199643250–252. [DOI] [PubMed] [Google Scholar]
- 50.Mutignani M, Shah S K, Bruni A.et al Endoscopic treatment of extrahepatic bile duct strictures in patients with portal biliopathy carries a high risk of hemobilia: report of 3 cases. Dig Liver Dis 200234587–591. [DOI] [PubMed] [Google Scholar]
- 51.Dumortier J, Vaillant E, Boillot O.et al Diagnosis and treatment of biliary obstruction caused by portal cavernoma. Endoscopy 200335446–450. [DOI] [PubMed] [Google Scholar]
- 52.Choudhuri G, Tandon R K, Nundy S.et al Common bile duct obstruction by portal cavernoma. Dig Dis Sci 1988331626–1628. [DOI] [PubMed] [Google Scholar]
- 53.Ouchi K, Tominaga T, Unno M.et al Obstructive jaundice associated with extrahepatic portal vein obstruction: report of two cases. Surg Today 199323737–741. [DOI] [PubMed] [Google Scholar]
- 54.Benjanin H, Baumann R, Choury A.et al Portal cavernoma compressing the bile duct. Apropos of three cases (in French). Gastroenterol Clin Biol 199317134–138. [PubMed] [Google Scholar]
- 55.Filipponi F, Urbani L, Catalano G.et al Portal biliopathy treated by liver transplantation. Transplantation 200477326–327. [DOI] [PubMed] [Google Scholar]
- 56.Yang J F, Wu X J, Li J S.et al Effect of somatostatin versus octreotide on portal haemodynamics in patients with cirrhosis and portal hypertension. Eur J Gastroenterol Hepatol 20051753–57. [DOI] [PubMed] [Google Scholar]
- 57.Escorsell A, Bandi J C, Moitinho E.et al Time profile of the hemodynamic effects of terlipressin in portal hypertension. J Hepatol 199726621–627. [DOI] [PubMed] [Google Scholar]