Abstract
Background
Accurate assessment of aortic valve area (AVA) is important for clinical decision‐making in patients with aortic valve stenosis (AS). The role of three‐dimensional echocardiography (3D) in the quantitative assessment of AS has not been evaluated so far.
Objectives
To evaluate the reproducibility and accuracy of real‐time three‐dimensional echocardiography (RT3D) and 3D‐guided two‐dimensional planimetry (3D/2D) for assessment of AS, and compare these results with those of standard echocardiography and cardiac catheterisation (Cath).
Methods
AVA was estimated by transthoracic echo‐Doppler (TTE) and by direct planimetry using transoesophageal echocardiography (TEE) as well as RT3D and 3D/2D. 15 patients underwent assessment of AS by Cath.
Results
33 patients with AS were studied (20 men, mean (SD) age 70 (14) years). Bland–Altman analysis showed good agreement and small absolute differences in AVA between all planimetric methods (RT3D vs 3D/2D: −0.01 (0.15) cm2; 3D/2D vs TEE: 0.05 (0.22) cm2; RT3D vs TEE: 0.06 (0.26) cm2). The agreement between AVA assessment by 2D–TTE and planimetry was −0.01 (0.20) cm2 for 3D/2D; 0.00 (0.15) cm2 for RT3D; and −0.05 (0.30) cm2 for TEE. Correlation coefficient r for AVA assessment between each of 3D/2D, RT3D, TEE planimetry and Cath was 0.81, 0.86 and 0.71, respectively. The intraobserver variability was similar for all methods, but interobserver variability was better for 3D techniques than for TEE (p<0.05).
Conclusions
The 3D echo methods for planimetry of the AVA showed good agreement with the standard TEE technique and flow‐derived methods. Compared with AV planimetry by TEE, both 3D methods were at least as good as TEE and had better reproducibility. 3D aortic valve planimetry is a novel non‐invasive technique, which provides an accurate and reliable quantitative assessment of AS.
Degenerative aortic stenosis (AS) is one of the most common valvular heart diseases resulting in valve replacement.1,2 The indication for surgery is based on symptoms and the severity of AS.3 The severity of AS can be assessed by calculating the valve orifice using catheter‐based invasive measurements or echocardiography. Transthoracic echocardiography is currently used in most instances as the standard for AS quantification, based on the determination of flow‐dependent variables and the effective aortic valve area (AVA). Quantification of AS should include measurement by both techniques; the symptomatic status of the patient is also crucial in assessing the necessity of valve surgery. In selected cases, catheterisation may be used for quantification of the severity of AS.
Historically, cardiac catheterisation using the Gorlin equation has been the gold standard for effective AVA assessment.4 Currently, two‐dimensional transthoracic echocardiography using transvalvular Doppler (2D‐TTE) is considered to be a reliable and accurate method to assess the severity of AS.5,6,7 In some patients with AS who have a small aorta, subvalvular obstruction, significant aortic regurgitation or depressed left ventricular function, the accurate assessment of AVA may be difficult.5,6,7,8,9,10,11,12 2D‐TTE with harmonic imaging has been used with some success for aortic valve planimetry, but it is less feasible than transoesophageal echocardiography (TEE).13 The multiplane TEE technique provides additional important information regarding the anatomy of the aortic valve and allows direct planimetric quantification of the anatomic AVA. The accuracy of this semi‐invasive method may be limited by difficulties in obtaining the correct cross‐sectional view at the level of the edges of the aortic valve cusps.12,14,15,16 The use of reconstructive three‐dimensional TEE has provided better results than standard TEE for AVA planimetry. However, this has not been widely adopted, partly because of the time‐consuming off‐line analysis.17 Other non‐echocardiographic methods such as multislice CT and MRI have also been successfully used for evaluation of the severity of AS18,19,20,21,22; however, they are time consuming and have other known limitations compared with a simple bedside echo study. Recently, transthoracic real‐time three‐dimensional echocardiography (RT3D) has been introduced as a novel technique, which allows the spatial recognition of the anatomy and function of cardiac structures. A number of studies have demonstrated significant additional value for planimetric assessment of mitral valve orifice in patients with mitral stenosis.23,24,25,26,27
The purpose of this study was to evaluate the use of RT3D as an alternative additional non‐invasive method to estimate AVA in patients with AS.
Methods
Patient population
Our study group comprised 36 consecutive patients with an established diagnosis of AS, 24 of whom were candidates for aortic valve replacement (AVR). Informed consent for three‐dimensional (3D) echocardiography imaging was obtained and approved by the Cedars‐Sinai Medical Center Institutional Review Board.
Echocardiographic methods
2D Imaging
A complete echo‐Doppler study was performed in all patients, using a Philips iE‐33 (Philips Medical System, Andover, Massachusetts, USA) machine and an S5‐1 probe. 2D‐TTE standard views were obtained. Doppler flow data were acquired from the left ventricular outflow tract (LVOT) region in the pulsed wave mode, and from the aortic valve in the continuous wave mode in the apical five‐chamber view. The LVOT diameter was measured in the parasternal long‐axis (LAX) view in proximity to the position of the pulse‐wave Doppler data. AVA was estimated using the continuity equation approach (AVA = LVOTarea(velocity time integralLVOT/velocity time integralvalve)). Three Doppler measurements were obtained, and calculations were based on the best representative heartbeats as selected independently, blinded to the 3D echocardiography, TEE and cardiac catheterisation data.
3D imaging
Volumetric RT3D and 3D‐guided image acquisition of the aortic valve was performed immediately after the 2D‐TTE, and within a week after the TEE and cardiac catheterisation. These images were acquired using a new X3‐1 matrix‐array transducer (frequency range of 1–3 MHz), with parallel processing to acquire a pyramidal volume dataset from a single window in real time and providing also 2D, Live xPlane and Live 3D performance. The live xPlane mode was used to acquire and display the 3D‐guided images.
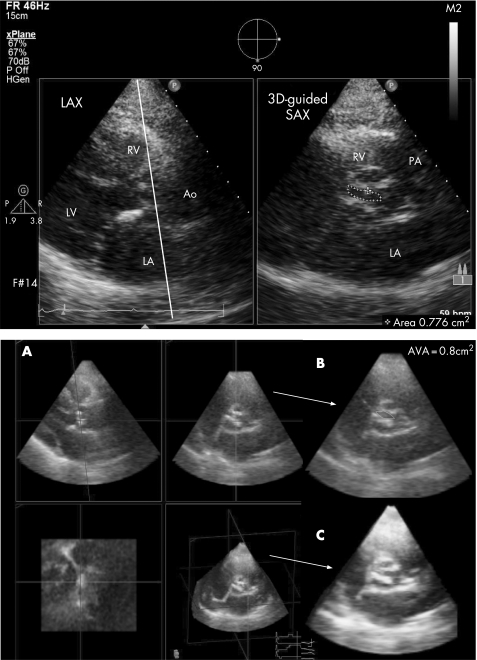
3D‐guided two‐dimensional imaging
The live xPlane mode was used to acquire and display the 3D‐guided two‐dimensional imaging (3D/2D) images simultaneously, side‐by‐side (biplane imaging; fig 1, upper panel). As described previously, this method provides accurate alignment of the limiting orifice and has been used for planimetry of the mitral valve.22 We applied the same technique for assessment of the AVA. The LAX view was used to guide the positioning of a manually placed cursor at the cusp edges of the aortic valve. Simultaneously, the valve orifice area on the short‐axis plane was obtained, and was traced on‐line when the cusps were maximally opened in systole.
Figure 1 Lower panel: Assessment of aortic valve anatomic area (AVA) by volumetric real‐time three‐dimensional echocardiography. The multiplanar reconstruction (MPR) mode is used for correct alignment and measurement of AVA. The pyramidal volume data (lower panel, A (bottom right) and C) were displayed in three different cross‐sections that could be modified interactively by use of colour‐coding convention. The parasternal long‐axis (LAX) view is displayed in the green quadrant (lower panel, A (top left)) and could be controlled by manually shifting and rotating a green line (planar slice) shown in the blue quadrant (lower panel, A (bottom left)) until the anatomically correct view of the aortic valve (AV) is achieved. The red line in the green quadrant (LAX) was manually shifted and rotated parallel to the alignment of the AV leaflets cross‐sectioning the edges of the cusps and resulting in the correct short‐axis (SAX) section of AV showed in the red quadrant (lower panel, A (top right)). When the optimal cross‐section of AV is achieved during its maximal systolic opening, the AVA is traced manually using the R (red quadrant) zoom mode (B). Upper panel: Aortic valve planimetry by using the Live xPlane mode. 3D‐guided two‐dimensional images (3D/2D) are displayed, simultaneously, side‐by‐side (biplane imaging). The parasternal LAX view is used to guide the positioning of a manually placed cursor at the edges of the aortic valve cusps. The simultaneous display of the two views showed a complete orifice visualised in the 3D‐guided SAX view, and aortic valve area is traced on‐line in midsystole when the leaflets were maximally opened. Ao, ascending aorta; LA, left atrium; LV, left ventricle; PA, pulmonary artery; RV, right ventricle.
Volumetric RT3D echocardiography
Initially, the aortic valve was aligned in the centre of the imaging plane, using the “Live 3D” function. Gain and compression controls, as well as the time gain compensation settings, were used to optimise the quality of the 3D images. Then, the full‐volume RT3D datasets were acquired from a single acoustic window (LAX), with the acquisition of four wedge‐shaped subvolumes (triggered to the ECG R‐wave) to form the “pyramid” (60°×60°) from four consecutive cardiac cycles during held respiration. A high‐density setting capable of fitting the entire aortic valve was used for better resolution. All volumetric images were analysed on‐line and also digitally stored on a compact disk and transferred into a personal computer for off‐line analysis using the commercial software (3D‐QLab, Philips Ultrasound, Andover, MA, USA). The multiplanar reconstruction mode has been used for correct alignment and measurement of AVA. The pyramidal volume data (fig 1, lower panel, A (bottom right) and C) were displayed in three different cross‐sections that could be modified interactively by the use of colour‐coding convention. When the optimal cross‐section of the aortic valve during its maximal systolic opening (the view with smallest aortic valve orifice) was achieved, the AVA was measured using the zoom mode (fig 1B). The AVA was manually traced and calculated as the mean of three measurements.
To evaluate reproducibility of the 3D methods, we selected an orifice from a 3D dataset and did three manual traces of AVA of 10 patients, performed by each of two independent operators who were blinded to the patients' identities and other clinical information.
TEE imaging
TEE was performed using an HDI‐5000 ultrasound system (Phillips Ultrasound, Bothell, WA, USA) with a 5 MHz multiplane probe. Images were digitised, and off‐line measurements were performed with the VERICIS Echo Review application (Camtronics Medical Systems, Hartland, Wisconsin, USA). TEE was performed in 24 patients as part of a routine intraoperative TEE before and after AVR. The rest of the patients were referred for TEE by their cardiologists as part of the clinical examination of the patients' aortic valve disease.
As reported previously,16 after placing the probe to visualise the standard TEE long‐axis view of the aortic valve and the ascending aorta, we rotated the image plane from 0° to 180°, yielding the best short‐axis image of the aortic valve opening. The aortic valve orifice during maximum opening in systole was measured on a magnified image in zoom mode. Planimetry was repeated three times off‐line and values were averaged accordingly.
Cardiac catheterisation
Cardiac catheterisation was performed by the standard femoral approach. Left ventricular pressure measurements were obtained after retrograde placement of the catheters. Transvalvular pressure gradients were acquired by simultaneous pressure measurements in the aorta and in the left ventricle (13 patients), or during a pullback manoeuvre (2 patients). Cardiac output was calculated according to the thermodilution method, which was then used to determine AVA by applying the Gorlin equation.4
Statistical methods
Values were expressed as the mean (SD) for RT3D, 3D/2D, 2D‐TTE, TEE and cardiac catheterisation, and the results were compared by linear regression analysis. Correlation coefficients were expressed as r values. Limits of agreement and the mean absolute differences of planimetric methods with Doppler‐derived and cardiac catheterisation AVA were calculated using the method of Bland and Altman. One‐factor analysis of variance and post‐hoc test were used to compare the significance of the bias for each method, and for comparison of intraobserver and interobserver variabilities between planimetric methods. Interobserver and intraobserver variabilities were presented as coefficients of variation and were calculated by dividing the SD of values by the mean. The values were measured by two blinded readers for interobserver variability, and by one of them on the same dataset after a gap of 2–3 weeks for intraobserver variability.
Results
Initially, 36 consecutive patients with AS were enrolled in this study. Three patients were excluded from the study: two patients because of an inadequate acoustic window, and one patient because of extremely calcified aortic valve and aortic root that did not allow adequate planimetry of AVA either by TEE or by 3D echocardiography. Thus, 33 patients comprised our study group. The individual clinical characteristics of all patients are presented in table 1. There were 13 women, and the mean (SD) age for the entire group was 70.2 (13.3) years. The mean AVA by 2D‐TTE was 1.03 (0.48) cm2. As per the American College of Cardiology/American Heart Association guidelines,3 22 patients had severe (AVA <1.0 cm2), 4 patients had moderate (AVA 1.0–1.5 cm2) and 7 had mild (AVA >1.5 cm2) AS. Four patients had a bicuspid aortic valve. Concomitant aortic regurgitation was present in 19 patients: trace or mild in 12 and mild to moderate in 7 patients. The mean left ventricular ejection fraction was 57.1% (14.7)% (range 20–74). In all, 32 patients were in normal sinus rhythm and 1 was in atrial fibrillation. The mean (SD) time required for obtaining images and measuring the AVA using the 3D/2D was 55 (12) s, and that using the RT3D was 6.5 (2.1) min.
Table 1 Clinical characteristics and aortic valve values in patients with aortic stenosis.
| Number | Age in years | Sex | EF (%) | AR grade | MR grade | AV gradient (mmHg) | 2D‐TTE AVA (cm2) | 3D/2D AVA (cm2) | RT3D AVA (cm2) | TEE AVA (cm2) | Cath AVA (cm2) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 76 | M | 40 | 2 | 2 | 67 | 0.70 | 0.77 | 0.80 | 0.89 | 0.75 |
| 2 | 60 | M | 30 | 1 | 2 | 48 | 0.90 | 0.90 | 0.90 | 0.76 | 1.25 |
| 3* | 64 | M | 68 | 1 | 1 | 36 | 0.90 | 0.98 | 0.88 | 0.99 | 0.95 |
| 4 | 83 | M | 55 | 1 | 1 | 71 | 0.80 | 0.73 | 0.75 | 0.93 | 0.79 |
| 5* | 65 | M | 65 | 2 | 1 | 105 | 0.69 | 0.65 | 0.78 | 0.87 | 0.77 |
| 6 | 81 | F | 55 | 1 | 2 | 70 | 0.80 | 0.66 | 0.78 | 0.78 | 0.85 |
| 7 | 42 | F | 65 | 2 | 2 | 44 | 1.24 | 1.30 | 1.18 | 1.51 | |
| 8 | 88 | F | 74 | 1 | 1 | 63 | 0.73 | 0.74 | 0.83 | 0.83 | 0.80 |
| 9* | 38 | F | 38 | 2 | 1 | 41 | 0.70 | 0.74 | 0.64 | 0.80 | |
| 10 | 55 | M | 67 | 2 | 2 | 64 | 0.80 | 0.89 | 0.81 | 0.96 | |
| 11 | 70 | M | 28 | 0 | 3 | 56 | 0.75 | 0.70 | 0.63 | 0.72 | |
| 12 | 91 | M | 58 | 1 | 1 | 21 | 1.23 | 0.99 | 1.05 | 0.79 | 1.00 |
| 13 | 75 | F | 65 | 0 | 1 | 65 | 0.70 | 0.85 | 0.83 | 0.79 | 0.73 |
| 14 | 80 | F | 68 | 1 | 3 | 67 | 0.70 | 0.62 | 0.57 | 0.54 | 0.50 |
| 15 | 85 | M | 28 | 1 | 1 | 38 | 0.60 | 0.64 | 0.67 | 0.65 | 0.63 |
| 16 | 57 | F | 68 | 0 | 2 | 67 | 0.80 | 0.70 | 0.72 | 0.80 | 0.70 |
| 17 | 81 | M | 67 | 0 | 0 | 78 | 0.70 | 0.70 | 0.77 | 0.85 | |
| 18 | 70 | M | 65 | 0 | 2 | 69 | 0.80 | 0.74 | 0.83 | 0.51 | |
| 19 | 79 | F | 50 | 2 | 2 | 122 | 0.45 | 0.43 | 0.43 | 0.46 | 0.38 |
| 20 | 78 | M | 60 | 0 | 4 | 71 | 0.57 | 0.62 | 0.56 | 0.74 | |
| 21 | 67 | M | 68 | 0 | 2 | 90 | 0.82 | 0.87 | 0.80 | 0.88 | |
| 22 | 81 | M | 20 | 0 | 2 | 22 | 1.95 | 1.87 | 2.00 | 1.97 | |
| 23 | 75 | M | 65 | 0 | 2 | 22 | 1.95 | 1.92 | 1.87 | 1.98 | |
| 24 | 72 | F | 68 | 2 | 3 | 20 | 1.57 | 1.87 | 1.63 | 1.91 | 0.66 |
| 25 | 50 | M | 55 | 1 | 1 | 75 | 0.67 | 0.73 | 0.67 | 0.69 | 0.70 |
| 26* | 42 | M | 65 | 1 | 1 | 93 | 0.68 | 0.64 | 0.62 | 0.81 | |
| 27 | 71 | M | 63 | 0 | 1 | 63 | 0.90 | 1.04 | 0.97 | 0.98 | |
| 28 | 78 | F | 70 | 0 | 0 | 26 | 1.84 | 1.88 | 1.86 | 1.77 | |
| 29 | 70 | M | 65 | 0 | 0 | 18 | 1.92 | 2.08 | 2.05 | 2.17 | |
| 30 | 74 | F | 60 | 0 | 3 | 16 | 1.98 | 1.89 | 1.93 | 2.06 | |
| 31 | 80 | M | 55 | 1 | 1 | 40 | 1.40 | 1.43 | 1.43 | 1.52 | |
| 32 | 74 | F | 60 | 1 | 2 | 31 | 1.48 | 1.47 | 1.47 | 1.54 | |
| 33† | 58 | F | 55 | 0 | 1 | 12 | 1.42 | 1.45 | 1.43 | 1.59 |
AR, aortic regurgitation; AVA, aortic valve area; AV gradient, aortic valve peak gradient; Cath, cardiac catheterisation; 3D/2D, 3D‐guided two‐dimensional imaging; EF, ejection fraction; MR, mitral regurgitation; RT3D, volumetric real‐time three‐dimensional echocardiography; TEE, planimetry by transoesophageal echocardiography; 2D‐TTE, Doppler‐derived two‐dimensional transthoracic echocardiography.
*Patients with bicuspid aortic valve.
†Patient with concomitant moderate mitral stenosis.
Comparison with the non‐invasive methods
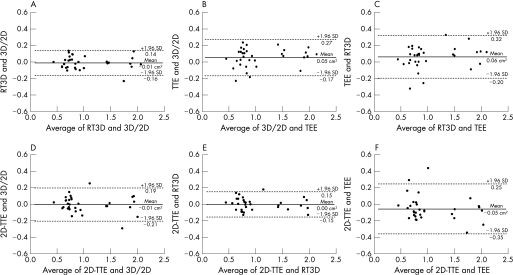
The mean (SD) AVA was 1.04 (0.49) cm2 for 3D/2D, 1.03 (0.48) cm2 for RT3D, 1.03 (0.48) cm2 for 2D‐TTE and 1.08 (0.51) cm2 for TEE. Table 2 shows good correlation between the non‐invasive methods. As presented in fig 2A–C, Bland–Altman analysis showed good agreement and small absolute differences in AVA between all planimetric methods (RT3D vs 3D/2D: −0.01 (0.15) cm2; 3D/2D vs TEE: 0.05 cm2 (0.22) cm2; RT3D vs TEE: 0.06 cm2 (0.26) cm2). As presented in fig 2D–F, when compared with TEE, there were smaller absolute differences in AVA and slightly better agreement between AVA derived from 2D‐TTE continuity equation and 3D methods (−0.01 (0.20) cm2 for 3D/2D; 0.00 (0.15) cm2 for RT3D and −0.05 (0.30) cm2 for TEE).
Table 2 Comparison of mean aortic valve area, correlation coefficient and mean absolute differences between different echo techniques.
| Mean (SD) AVA (cm2) | Correlation (r value, mean difference (cm2)) | |||
|---|---|---|---|---|
| vs RT3D | vs TEE | vs 2D‐TTE | ||
| 3D/2D | 1.04 (0.49) | r = 0.99, p<0.001, Δ = 0.008 | r = 0.98, p<0.001, Δ = 0.041 | r = 0.98, p<0.001, Δ = 0.009 |
| RT3D | 1.03 (0.48) | r = 0.97, p<0.001, Δ = 0.049 | r = 0.99, p<0.001, Δ = 0.001 | |
| TEE | 1.08 (0.51) | r = 0.96, p<0.001, Δ = 0.050 | ||
| 2D‐TTE | 1.03 (0.48) | |||
AVA, aortic valve area; 3D/2D, 3D‐guided two‐dimensional imaging; RT3D, volumetric real‐time three‐dimensional echocardiography; TEE, planimetry by transoesophageal echocardiography; 2D‐TTE, Doppler‐derived two‐dimensional transthoracic echocardiography; Δ, mean absolute differences.
Figure 2 Bland–Altman graphs (A–C) show the limits of agreement and mean absolute differences between planimetric methods: volumetric real‐time three‐dimensional echocardiography (RT3D) and 3D‐guided two‐dimensional imaging (3D/2D) (A), between 3D/2D and planimetry by transoesophageal echocardiography (TEE) (B) and between RT3D and TEE (C). Bland–Altman plots (D–F) show the limits of agreement and mean absolute differences between Doppler‐derived two‐dimensional transthoracic echocardiography (2D‐TTE) and 3D/2D (D); 2D‐TTE and RT3D (E); and 2D‐TTE and TEE (F).
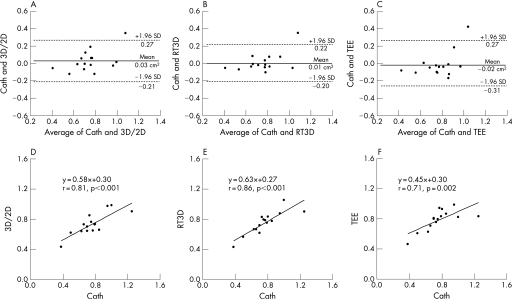
Comparison with invasive assessment
The mean (SD) values of AVA determined in the 15 patients who also underwent invasive assessment of AS were 0.73 (0.15) cm2 for 3D/2D, 0.75 (0.15) cm2 for RT3D, 0.78 (0.14) cm2 for TEE and 0.76 (0.21) cm2 for cardiac catheterisation. As demonstrated in fig 3, when comparing the invasively determined AVA by the Gorlin method with the planimetric AVA derived from 3D/2D, RT3D and TEE, the smallest mean absolute differences and narrower limits of agreement were obtained by RT3D (0.03 (0.24), 0.01 (0.21) and −0.02 (0.29) cm2). Figure 3 shows the acceptable correlation between the 3D methods and cardiac catheterisation (r = 0.81 and 0.86).
Figure 3 Bland–Altman plots (A–C) show the limits of agreement and mean absolute differences between AVA (aortic valve area) by Cath (cardiac catheterisation) and 2D/3D (3D‐guided two‐dimensional imaging; A), RT3D (volumetric real‐time three‐dimensional echocardiography; B) and TEE (planimetry by transoesophageal echocardiography; C). Linear regression graphs (D, E) show the correlation between Cath and planimetric techniques with regard to AVA estimation: 2D/3D (D), RT3D (F) and TEE (E).
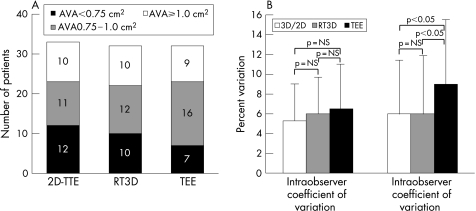
Comparison between methods to assess the grade of severity of AS
In view of the importance of an accurate AVA measurement in patients with severe AS, owing to the potential surgical treatment, we compared values of AVA by RT3D (the most accurate method that correlated well with flow‐derived methods) and TEE using cut‐offs of AVA measurements: AVA <0.75 cm2, AVA 0.75–1.0 cm2, AVA ⩾1.0 cm2. As validated by the 2D‐TTE assessment of AVA, clinically relevant underestimation of AS was observed among patients with severe or critical AS (fig 4A). Critical AS (AVA <0.75 cm2) was underestimated in 5 of 12 patients by TEE, but in only 2 of 12 by RT3D. When looking at the group with severe AS (AVA <1.0 cm2), the comparison yielded an overestimation in one patient by RT3D.
Figure 4 (A) The comparison between 2D‐TEE (Doppler‐derived two‐dimensional transthoracic echocardiography), RT3D (volumetric real‐time three‐dimensional echocardiography) and TEE (planimetry by transoesophageal echocardiography) to yield the clinical classification of the severity of AS (aortic stenosis). The numbers in the bars represent the actual number of patients according to the grade of AS. (B) Intraobserver and interobserver differences in aortic valve area (AVA) measurements by 3D/2D (3D‐guided two‐dimensional method), RT3D and TEE.
Intraobserver and interobserver variabilities
Figure 4B shows good intraobserver agreement for all planimetric methods. However, interobserver agreement was significantly better for the 3D techniques than for TEE.
Discussion
This is the first study to apply 3D‐guided and volumetric RT3D techniques for the assessment of AS. Measurement of the AVA by both techniques correlated well with TEE and 2D‐TTE Doppler‐derived results, and had an acceptable correlation with catheter‐derived AVA. Bland–Altman analysis demonstrated good agreement between all planimetric techniques (3D/2D, volumetric RT3D and TEE) and flow‐derived methods. Both 3D methods showed good reproducibility and were feasible in the majority (92%) of patients.
The indications for AVR are usually based on symptoms and the severity of AS, and are well defined.3 The accurate assessment of AVA may have a crucial role in decision‐making in patients with severe AS. Even selected asymptomatic patients with severe and progressive AS may benefit from early surgery.28 Transthoracic echocardiography is currently used in most instances, as the current standard for AS quantification is based on the determination of both flow‐dependent variables (transaortic velocities or gradients) and a flow‐independent variable (valve area determined by the continuity equation). Quantification of AS should include the information of both measurement techniques. Moreover, the symptomatic status of the patient is critical to the clinical decision‐making process. In selected cases, catheterisation might become necessary to verify the aortic valve area.
Both cardiac catheterisation and echocardiography are known to provide accurate assessment of AS. Although cardiac catheterisation has been used as a gold standard, there are a number of limitations related to catheter positioning and postvalvular pressure recovery in mild and moderate AS, as well as some potential inaccuracy in the measurement of cardiac output.11 The American College of Cardiology/American Heart Association guidelines suggest that cardiac catheterisation for the assessment of AS may be useful when there is a discrepancy between clinical and echocardiographic findings.3 Thus, the Doppler‐derived measurements of effective AVA are frequently used as the gold standard to assess the severity of AS in clinical practice. The Doppler method, however, has some limitations when used in patients with left ventricular dysfunction, increased LVOT gradients and an eccentric jet in bicuspid aortic valves, or when there is associated significant aortic regurgitation.5,6,7,8,9,10,11,12 Consequently, in many cases, an additional echocardiographic modality such as planimetry may be helpful.
The anatomical determination of aortic valve orifice can be assessed by AV planimetry. TEE is a semi‐invasive technique, which allows direct planimetric measurements of AVA and is independent of the acoustic window, compared with 2D‐TTE. Two prior studies found clinically important overestimation of effective valve area by TEE planimetry compared with flow‐derived methods.15,29 This finding was described primarily in smaller valve areas and can be partially explained by differences in aortic valve shape.29 The major limitation of TEE for direct planimetry of the AVA is due to the difficulty and the potential inability to correctly identify the right imaging plane. Consequently, reproducibility and accuracy vary among investigators.12,14,15 3D TEE may overcome the problem of optimal image plane orientation, but it still requires off‐line image reconstruction, which is time consuming.17
In this study, we found good agreement between the techniques on comparing the 3D‐guided and volumetric RT3D methods with TEE. However, both 3D methods had smaller bias and narrower limits of agreement with the 2D‐TTE continuity equation‐derived AVA. In the group of patients who also underwent cardiac catheterisation, catheter‐derived AVA correlated better with planimetric AVA by the 3D techniques than those by TEE. Moreover, although there is no clear gold standard for the severity of AS in our study, these two observations lead us to conclude that 3D‐derived AVA is probably more accurate than TEE planimetry. This method may therefore be used in patients in whom there is a discrepancy in AVA assessment. In this study, we found that when these measures were evaluated relative to commonly used AVA cut‐off criteria for significant and critical AS, the differences in AVA between 3D and TEE translated to clinically important underestimation of the severity of AS in 3 (10%) patients. The intraobserver variability was similar for TEE and 3D techniques. However, in our study, the 3D method significantly reduced the interobserver variability. As reported previously, heavy valvular calcification may make the assessment of the actual orifice area difficult to measure by planimetry.15 This limitation is relevant for either of the planimetric echo techniques—TEE or 3D echocardiography. In our study, we excluded only one patient in whom the AVA measurement was not adequate. In addition, echo‐derived methods overestimate the severity of AS in patients with low cardiac output.30 Similarly, 3D planimetry is affected by low cardiac output as the anatomic area of aortic valve opening is reduced, and will potentially result in an inaccurate measurement of AVA.
Recently, 3D echocardiography (3D‐guided and volumetric RT3D) was shown to be an accurate, feasible and reproducible method for assessment of mitral stenosis severity.23,24,25,26,27 The diminished resolution and off‐line 3D analysis have been the main limiting factors for routine use.23 However, the development of a matrix‐array transducer in the biplane mode resolves the issue of limited resolution; it still remains a problem for volumetric RT3D planimetry. Currently available off‐line analysis for 3D echo significantly shortens the time of planimetry compared with previous studies using off‐line analysis programmes.23,26 The determination of AVA in patients with AS by both 3D modalities is feasible and accurate, and can be performed at the same time as the standard 2D‐TTE. Compared with TEE, 3D techniques have the advantage of being non‐invasive, highly reproducible methods, which provide correct image plane orientation.
Conclusion
3D‐guided and volumetric RT3D echocardiographies provide an accurate and reproducible estimation of AVA in patients with AS. These techniques showed good agreement with TEE and flow‐derived methods. Determination of AVA by RT3D is non‐invasive, simple and can be performed at the bedside in a few minutes.
Acknowledgements
We thank Eric Guerra, David Barreto and Tina Yu for technical assistance, and James Mirocha for help with statistical analysis.
Abbreviations
AS - aortic stenosis
AVA - aortic valve area
AVR - aortic valve replacement
3D/2D - 3D‐guided two‐dimensional imaging
LAX - long axis
LVOT - left ventricular outflow tract
RT3D - transthoracic real‐time three‐dimensional echocardiography
TEE - transoesophageal echocardiography
2D‐TTE - transthoracic echocardiography using transvalvular Doppler
Footnotes
Competing interests: None declared.
References
- 1.Selzer A. Changing aspects of the natural history of valvular aortic stenosis. N Engl J Med 198731791–98. [DOI] [PubMed] [Google Scholar]
- 2.Stewart B F, Siscovick D, Lind B K.et al Clinical factors associated with calcific aortic valve disease. Cardiovascular Health Study. J Am Coll Cardiol 199729630–634. [DOI] [PubMed] [Google Scholar]
- 3.Bonow R O, Carabello B, Chatterjee K.et al ACC/AHA/ESC 2006 practice guidelines for the management of patients with valvular heart disease: executive summary. A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to revise the 1998 guidelines for the management of patients with valvular heart disease) developed in collaboration with the Society of Cardiovascular Anesthesiologists endorsed by the Society for Cardiovascular Angiography and Interventions and the Society of Thoracic Surgeons. J Am Coll Cardiol 200648598–675. [DOI] [PubMed] [Google Scholar]
- 4.Gorlin R, Gorlin S. Hydraulic formula for calculation of the area of the stenotic mitral valve, other cardiac valves, and central circulatory shunts. Am Heart J 1951411–18. [DOI] [PubMed] [Google Scholar]
- 5.Skjaerpe T, Hegrenaes L, Hatle L. Non‐invasive estimation of valve area in patients with aortic stenosis by Doppler ultrasound and two‐dimensional echocardiography. Circulation 198572810–818. [DOI] [PubMed] [Google Scholar]
- 6.Zoghbi W A, Farmer K L, Soto J G.et al Accurate noninvasive quantification of stenotic aortic valve area by Doppler echocardiography. Circulation 198673452–459. [DOI] [PubMed] [Google Scholar]
- 7.Fischer J L, Haberer T, Dickson D.et al Comparison of Doppler echocardiographic methods with heart catheterisation in assessing aortic valve area in 100 patients with aortic stenosis. Br Heart J 199573293–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bartunek J, De Bacquer D, Rodrigues A C.et al Accuracy of aortic stenosis severity assessment by Doppler echocardiography: importance of image quality. Int J Card Imaging 19951197–104. [DOI] [PubMed] [Google Scholar]
- 9.Rahimtoola S H. Severe aortic stenosis with low systolic gradient: the good and bad news. Circulation 20001011892–1894. [DOI] [PubMed] [Google Scholar]
- 10.Danielsen R, Nordrehaug J E, Vik‐Mo H. Factors affecting Doppler echocardiographic valve area assessment in aortic stenosis. Am J Cardiol 1989631107–1111. [DOI] [PubMed] [Google Scholar]
- 11.Segal J, Lerner D J, Miller D C.et al When should Doppler‐determined valve area be better than the Gorlin formula? Variation in hydraulic constants in low flow states. J Am Coll Cardiol 198791294–1305. [DOI] [PubMed] [Google Scholar]
- 12.Donal E, Novaro G M, Deserrano D.et al Planimetric assessment of anatomic valve area overestimates effective orifice area in bicuspid aortic stenosis. J Am Soc Echocardiogr 2005181392–1398. [DOI] [PubMed] [Google Scholar]
- 13.Brasch A V, Luo H, Khan S S.et al Effect of harmonic imaging for planimetry on transthoracic echocardiography on visualization of the aortic valve. Am J Cardiol 2001881047–1049. [DOI] [PubMed] [Google Scholar]
- 14.Cormier B, Iung B, Porte J M.et al Value of multiplane transesophageal echocardiography in determining aortic valve area in aortic stenosis. Am J Cardiol 199677882–885. [DOI] [PubMed] [Google Scholar]
- 15.Bernard Y, Meneveau N, Vuillemenot A.et al Planimetry of aortic valve area using multiplane transoesophageal echocardiography is not a reliable method for assessing severity of aortic stenosis. Heart 19977868–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim C J, Berglund H, Nishioka T.et al Correspondence of aortic valve area determination from transesophageal echocardiography, transthoracic echocardiography, and cardiac catheterization. Am Heart J 19961321163–1172. [DOI] [PubMed] [Google Scholar]
- 17.Ge S, Warner J G, Jr, Abraham T P.et al Three‐dimensional surface area of the aortic valve orifice by three‐dimensional echocardiography: clinical validation of a novel index for assessment of aortic stenosis. Am Heart J 19981361042–1050. [DOI] [PubMed] [Google Scholar]
- 18.Messika‐Zeitoun D, Aubry M C, Detaint D.et al Evaluation and clinical implications of aortic valve calcification measured by electron‐beam computed tomography. Circulation 2004110356–362. [DOI] [PubMed] [Google Scholar]
- 19.Feuchtner G M, Dichtl W, Friedrich G J.et al Multislice computed tomography for detection of patients with aortic valve stenosis and quantification of severity. J Am Coll Cardiol 2006471410–1417. [DOI] [PubMed] [Google Scholar]
- 20.John A S, Dill T, Brandt R R.et al Magnetic resonance to assess the aortic valve area in aortic stenosis: how does it compare to current diagnostic standards? J Am Coll Cardiol 200342519–526. [DOI] [PubMed] [Google Scholar]
- 21.Caruthers S D, Lin S J, Brown P.et al Practical value of cardiac magnetic resonance imaging for clinical quantification of aortic valve stenosis: comparison with echocardiography. Circulation 20031082236–2243. [DOI] [PubMed] [Google Scholar]
- 22.Kupfahl C, Honold M, Meinhardt G.et al Evaluation of aortic stenosis by cardiovascular magnetic resonance imaging: comparison with established routine clinical techniques. Heart 200490893–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sebag I A, Morgan J G, Handschumacher M D.et al Usefulness of three‐dimensionally guided assessment of mitral stenosis using matrix‐array ultrasound. Am J Cardiol 2005961151–1156. [DOI] [PubMed] [Google Scholar]
- 24.Sugeng L, Weinert L, Lammertin G.et al Accuracy of mitral valve area measurements using transthoracic rapid freehand 3‐dimensional scanning: comparison with non‐invasive and invasive methods. J Am Soc Echocardiogr 2003161292–1300. [DOI] [PubMed] [Google Scholar]
- 25.Zamorano J, Perez de Isla L, Sugeng L.et al Non‐invasive assessment of mitral valve area during percutaneous balloon mitral valvuloplasty: role of real‐time 3D echocardiography. Eur Heart J 2004252086–2091. [DOI] [PubMed] [Google Scholar]
- 26.Zamorano J, Cordeiro P, Sugeng L.et al Real‐time three‐dimensional echocardiography for rheumatic mitral valve stenosis evaluation: an accurate and novel approach. J Am Coll Cardiol 2004432091–2096. [DOI] [PubMed] [Google Scholar]
- 27.Binder T M, Rosenhek R, Porenta G.et al Improved assessment of mitral valve stenosis by volumetric real‐time three‐dimensional echocardiography. J Am Coll Cardiol 2000361355–1361. [DOI] [PubMed] [Google Scholar]
- 28.Rosenhek R, Binder T, Porenta G.et al Predictors of outcome in severe, asymptomatic aortic stenosis. N Engl J Med 2000343611–617. [DOI] [PubMed] [Google Scholar]
- 29.Gilon D, Cape E G, Handschumacher M D.et al Effect of three‐dimensional valve shape on the hemodynamics of aortic stenosis: three‐dimensional echocardiographic stereolithography and patient studies. J Am Coll Cardiol 2002401479–1486. [DOI] [PubMed] [Google Scholar]
- 30.Rahimtoola S H. Severe aortic stenosis with low systolic gradient: the good and bad news. Circulation. 2000 25 1011892–1894. [DOI] [PubMed] [Google Scholar]