Abstract
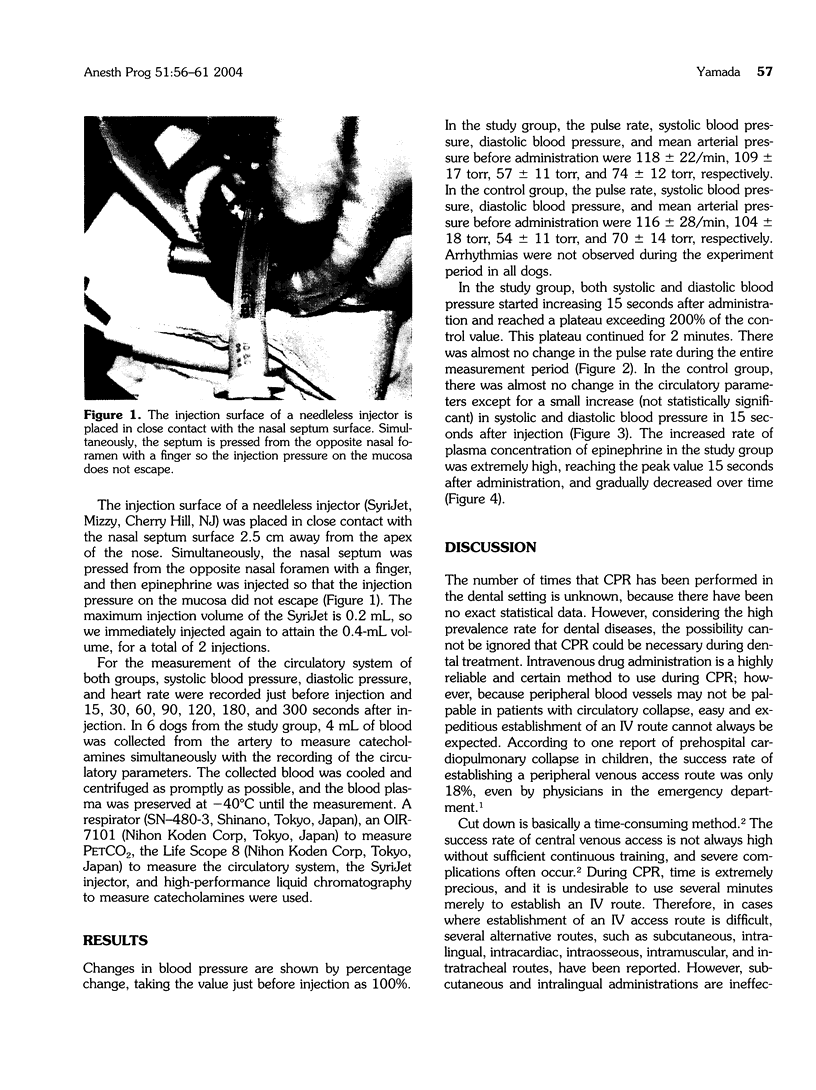
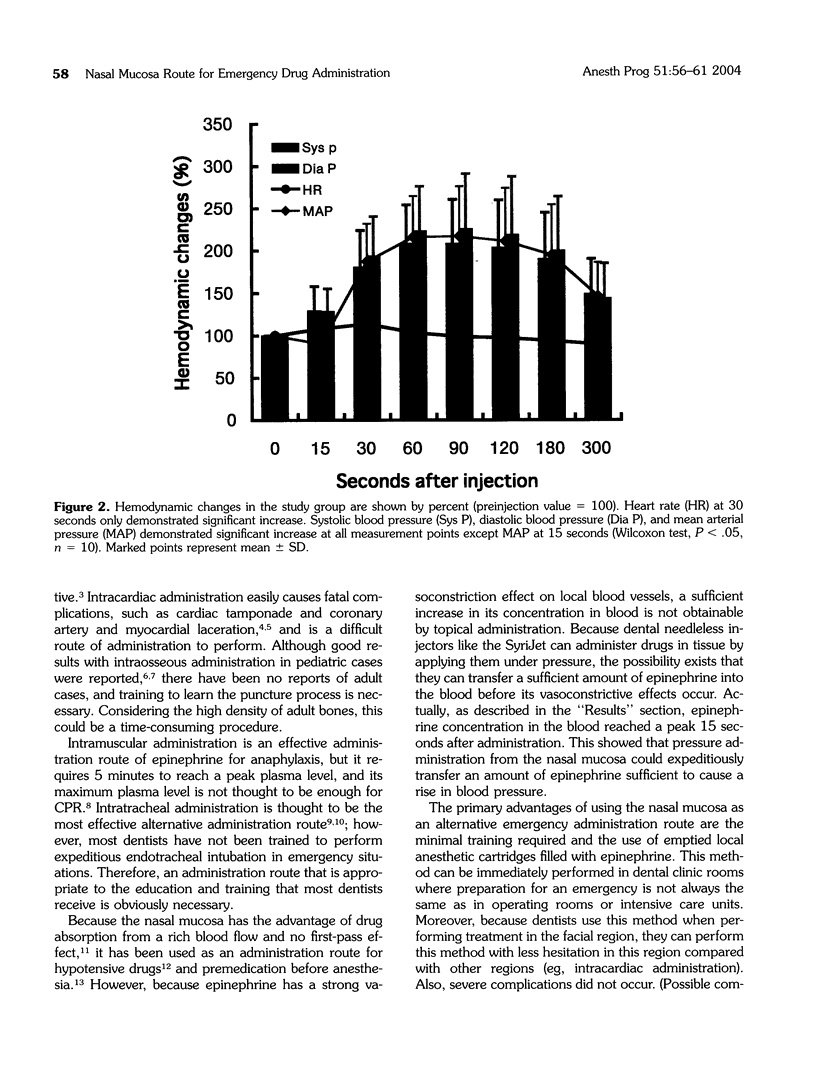
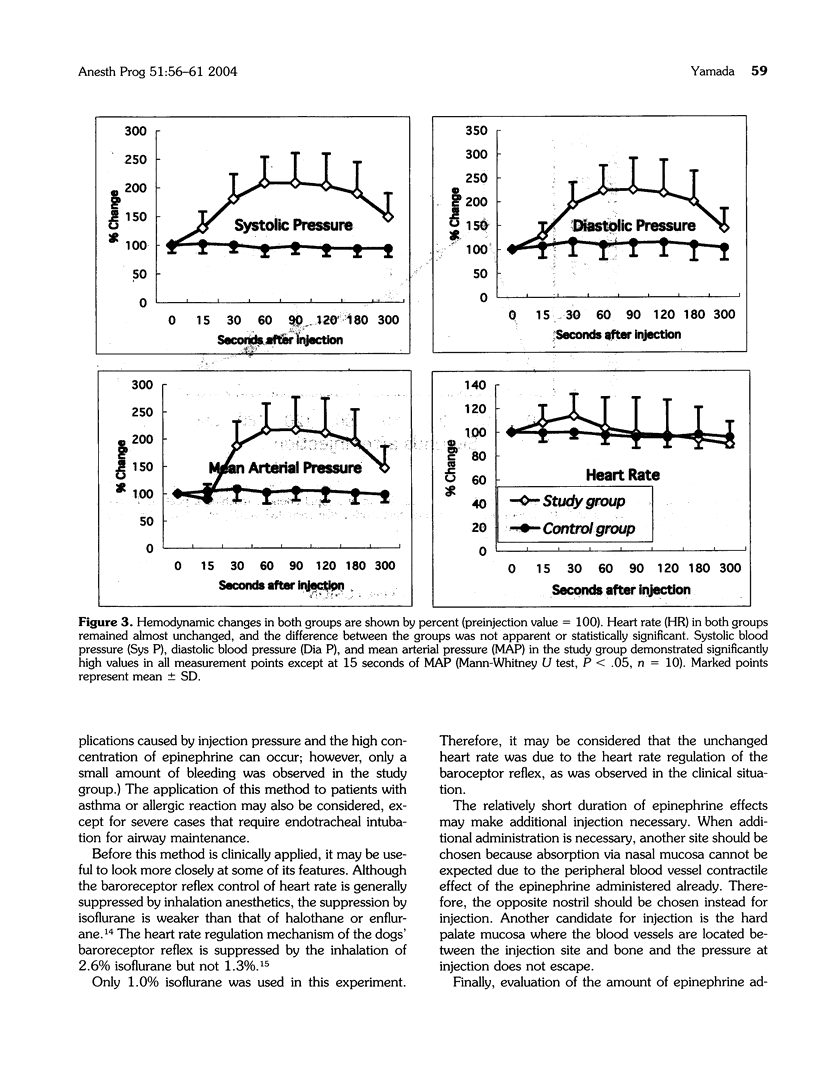
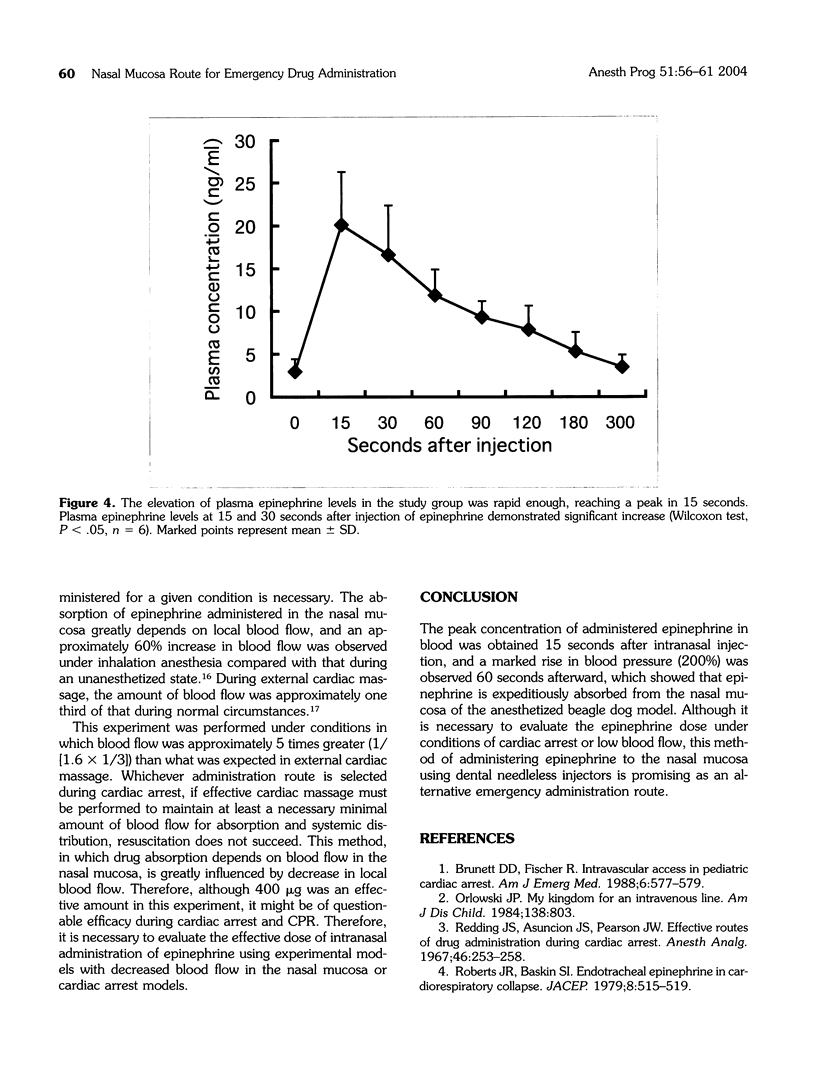
It is often difficult to expeditiously establish an intravenous (IV) route in a medical emergency, and alternatives to an IV route may also be difficult for many dentists to accomplish. The purpose of this article is to demonstrate that without the necessity of advanced training, the nasal mucosa route of administration is a promising alternative to the IV route in an emergency without complications, and will also show that epinephrine can be quickly absorbed into systemic circulation from the nasal mucosa. Ten beagle dogs were administered 400 microg of epinephrine in the nasal septal mucosa. The mean peak value of the plasma epinephrine (20.1 +/- 12.4 ng/mL) was obtained after 15 seconds, and the peak systolic pressure was 200% of the control value after 60 seconds. Although the dose of epinephrine must be considered because blood flow decreases during cardiopulmonary resuscitation, this method presents a promising alternative to the IV route.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Berg R. A. Emergency infusion of catecholamines into bone marrow. Am J Dis Child. 1984 Sep;138(9):810–811. doi: 10.1001/archpedi.1984.02140470010003. [DOI] [PubMed] [Google Scholar]
- Brunette D. D., Fischer R. Intravascular access in pediatric cardiac arrest. Am J Emerg Med. 1988 Nov;6(6):577–579. doi: 10.1016/0735-6757(88)90094-0. [DOI] [PubMed] [Google Scholar]
- Glaeser P. W., Losek J. D., Nelson D. B., Bonadio W. A., Smith D. S., Walsh-Kelly C., Hennes H. Pediatric intraosseous infusions: impact on vascular access time. Am J Emerg Med. 1988 Jul;6(4):330–332. doi: 10.1016/0735-6757(88)90149-0. [DOI] [PubMed] [Google Scholar]
- Gu X., Simons F. E., Simons K. J. Epinephrine absorption after different routes of administration in an animal model. Biopharm Drug Dispos. 1999 Nov;20(8):401–405. doi: 10.1002/1099-081x(199911)20:8<401::aid-bdd204>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- Kotrly K. J., Ebert T. J., Vucins E., Igler F. O., Barney J. A., Kampine J. P. Baroreceptor reflex control of heart rate during isoflurane anesthesia in humans. Anesthesiology. 1984 Mar;60(3):173–179. doi: 10.1097/00000542-198403000-00001. [DOI] [PubMed] [Google Scholar]
- Orlowski J. P. My kingdom for an intravenous line. Am J Dis Child. 1984 Sep;138(9):803–803. doi: 10.1001/archpedi.1984.02140470003001. [DOI] [PubMed] [Google Scholar]
- Peters J., Ihle P. Mechanics of the circulation during cardiopulmonary resuscitation. Pathophysiology and techniques (Part I). Intensive Care Med. 1990;16(1):11–19. doi: 10.1007/BF01706319. [DOI] [PubMed] [Google Scholar]
- Redding J. S., Asuncion J. S., Pearson J. W. Effective routes of drug administration during cardiac arrest. Anesth Analg. 1967 Mar-Apr;46(2):253–258. [PubMed] [Google Scholar]
- Roberts J. R., Greenberg M. I., Baskin S. I. Endotracheal epinephrine in cardiorespiratory collapse. JACEP. 1979 Dec;8(12):515–519. doi: 10.1016/s0361-1124(79)80298-1. [DOI] [PubMed] [Google Scholar]
- Roberts J. R., Greenberg M. I., Knaub M. A., Kendrick Z. V., Baskin S. I. Blood levels following intravenous and endotracheal epinephrine administration. JACEP. 1979 Feb;8(2):53–56. doi: 10.1016/s0361-1124(79)80036-2. [DOI] [PubMed] [Google Scholar]
- Roberts J. R., Greenburg M. I., Knaub M., Baskin S. I. Comparison of the pharmacological effects of epinephrine administered by the intravenous and endotracheal routes. JACEP. 1978 Jul;7(7):260–264. doi: 10.1016/s0361-1124(78)80335-9. [DOI] [PubMed] [Google Scholar]
- Seagard J. L., Elegbe E. O., Hopp F. A., Bosnjak Z. J., von Colditz J. H., Kalbfleisch J. H., Kampine J. P. Effects of isoflurane on the baroreceptor reflex. Anesthesiology. 1983 Dec;59(6):511–520. doi: 10.1097/00000542-198312000-00005. [DOI] [PubMed] [Google Scholar]
- Wilton N. C., Leigh J., Rosen D. R., Pandit U. A. Preanesthetic sedation of preschool children using intranasal midazolam. Anesthesiology. 1988 Dec;69(6):972–975. doi: 10.1097/00000542-198812000-00032. [DOI] [PubMed] [Google Scholar]



