Abstract
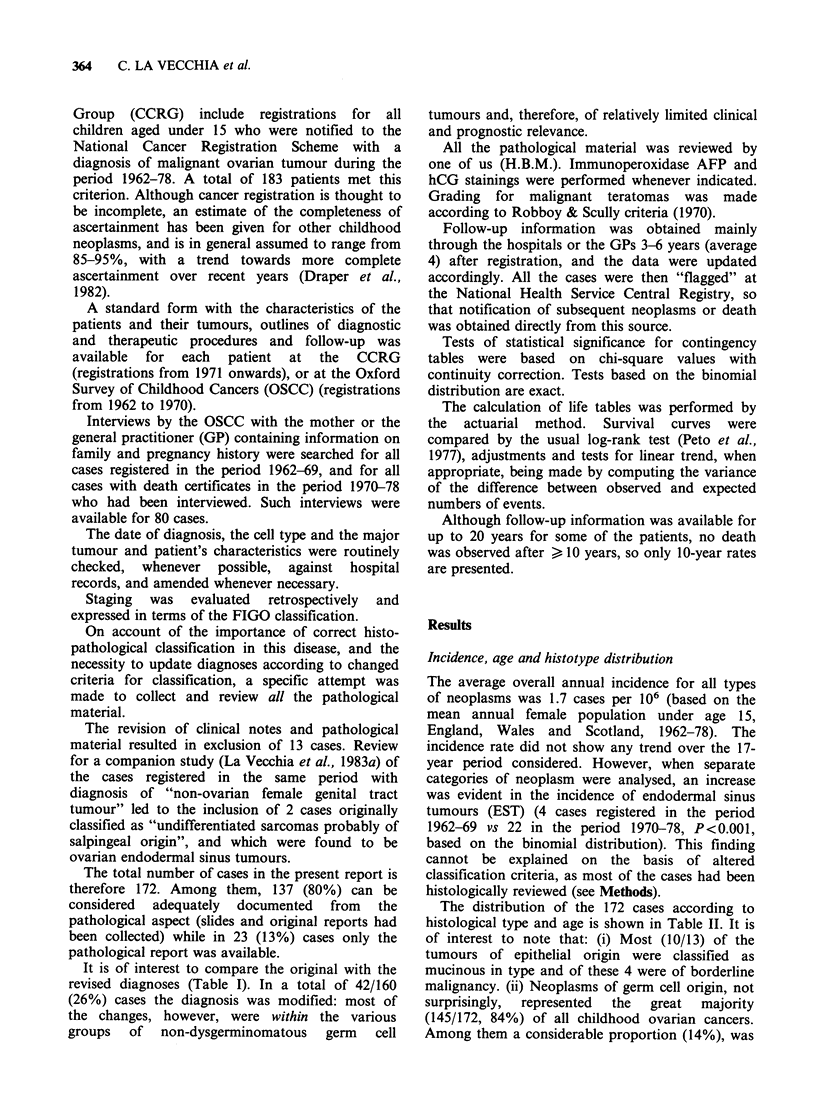
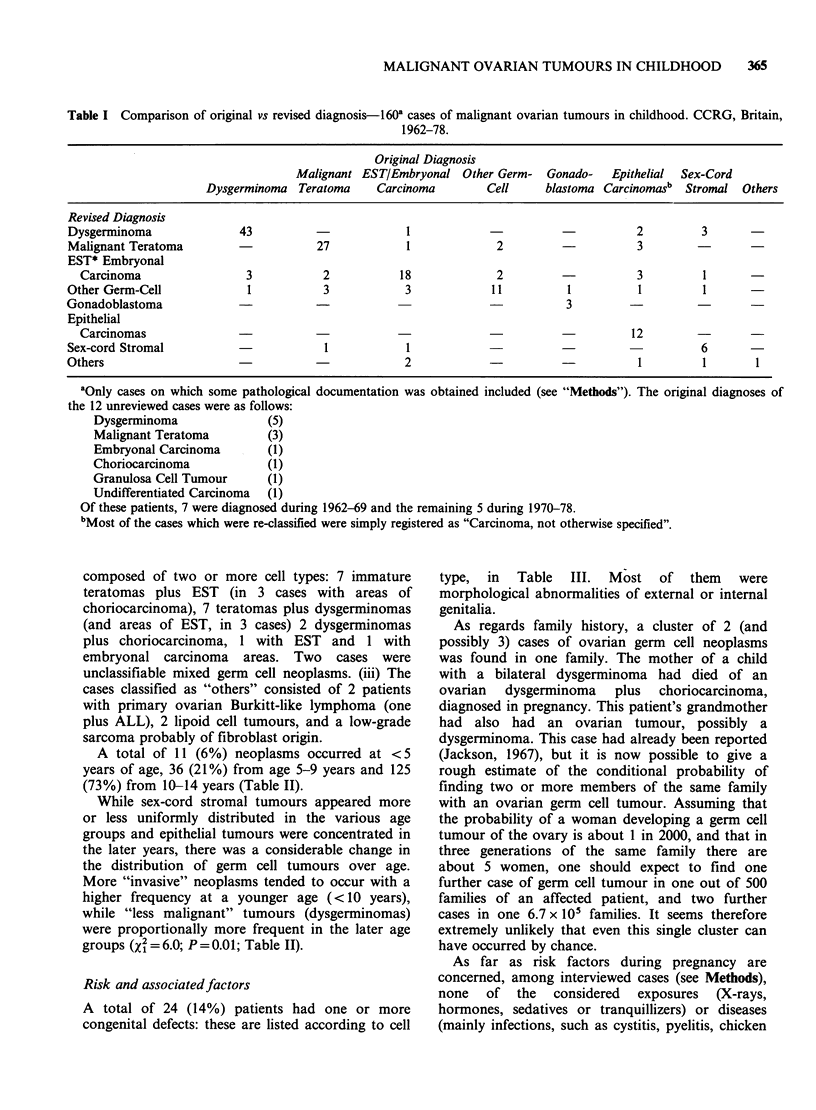
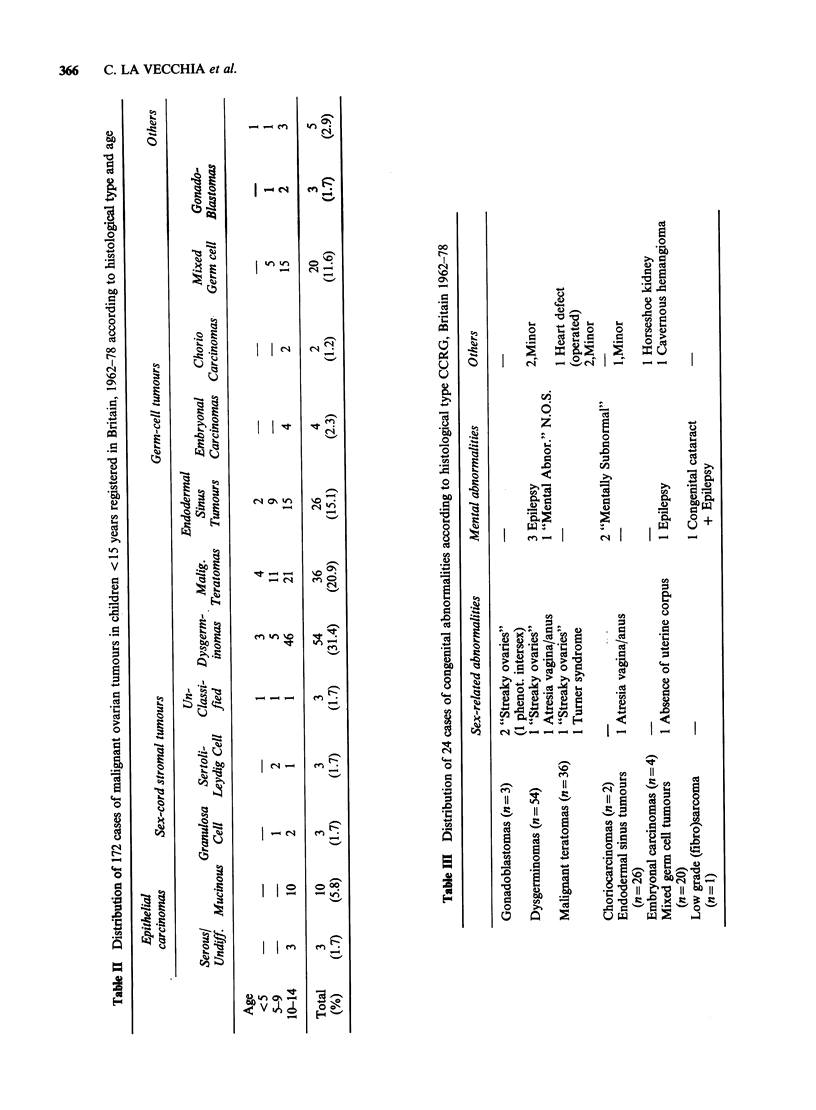
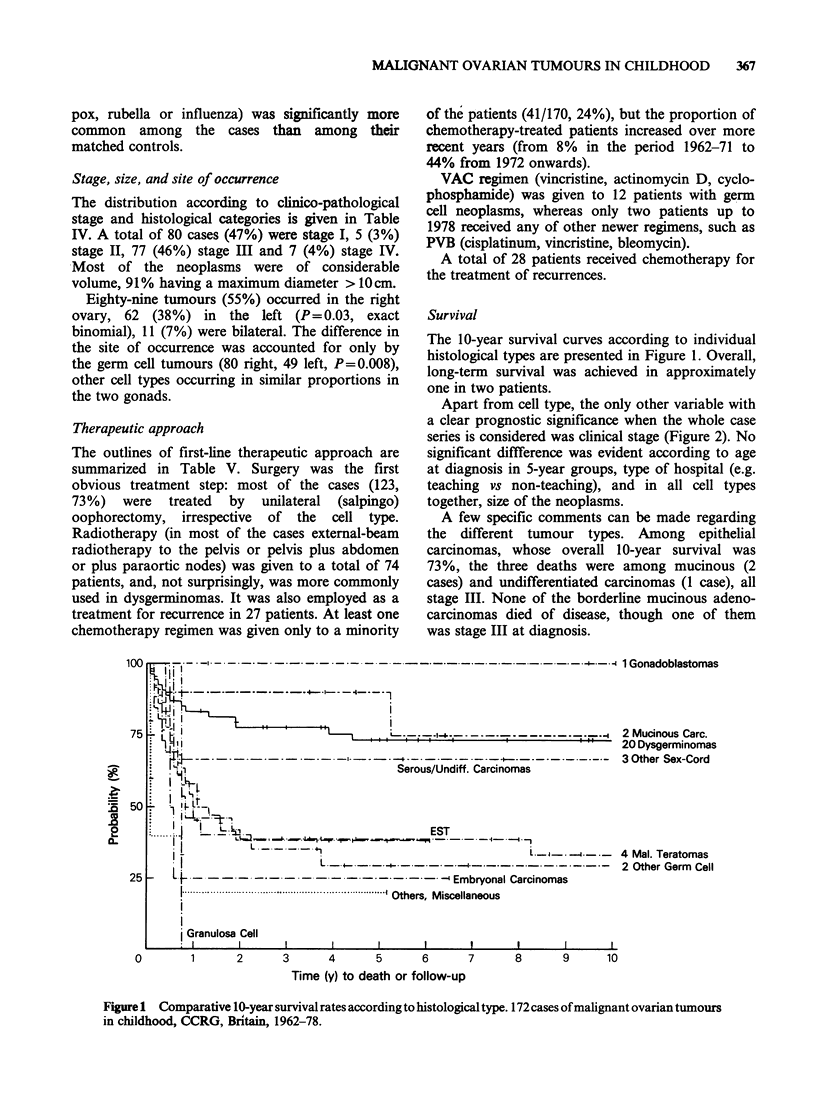
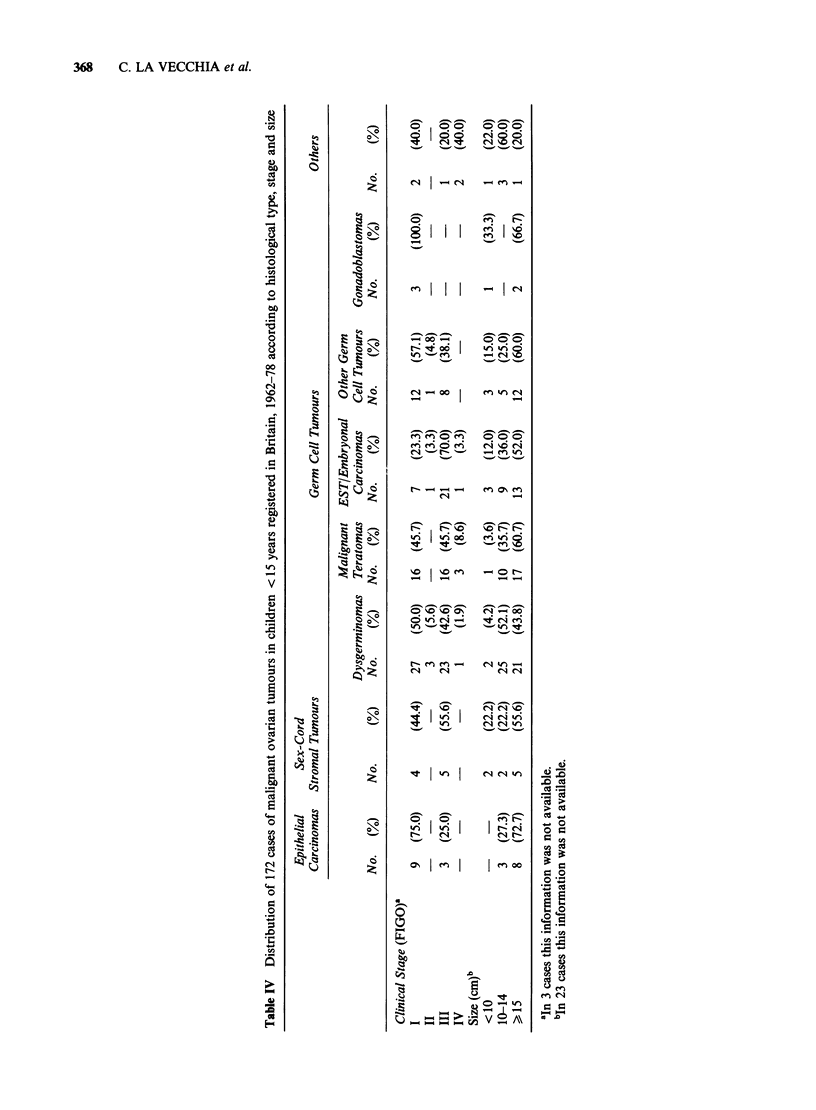
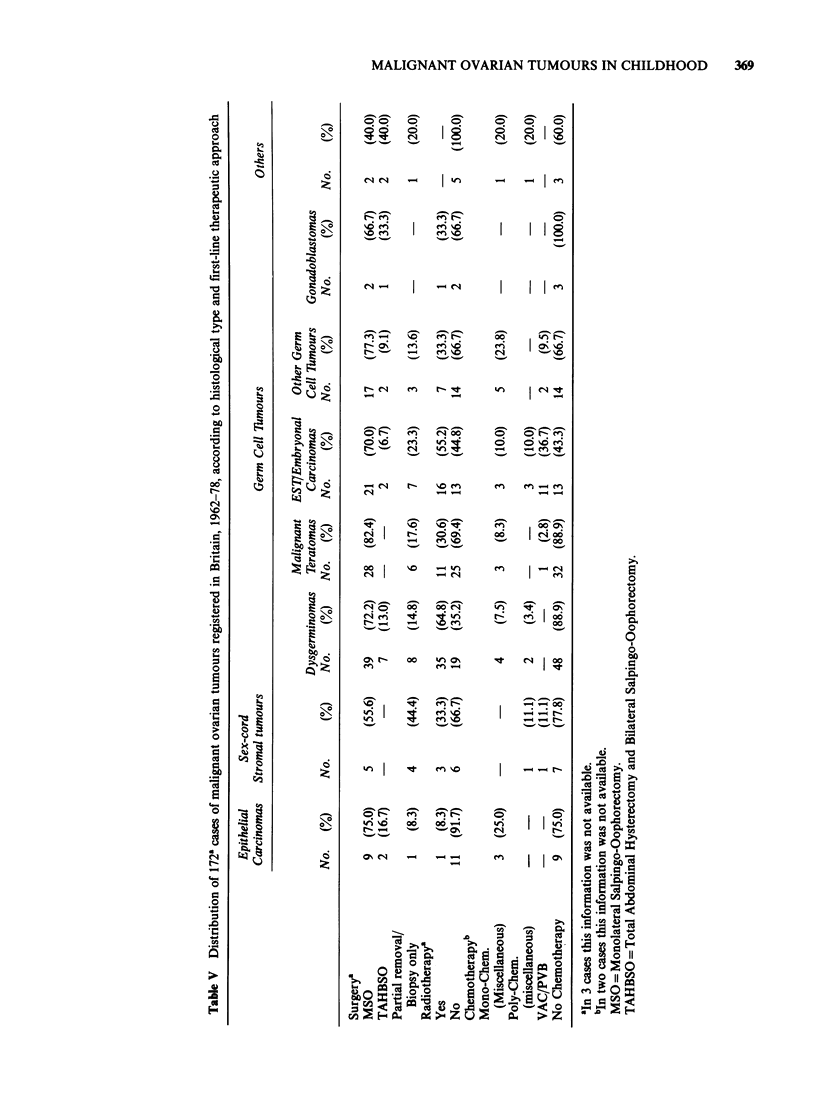
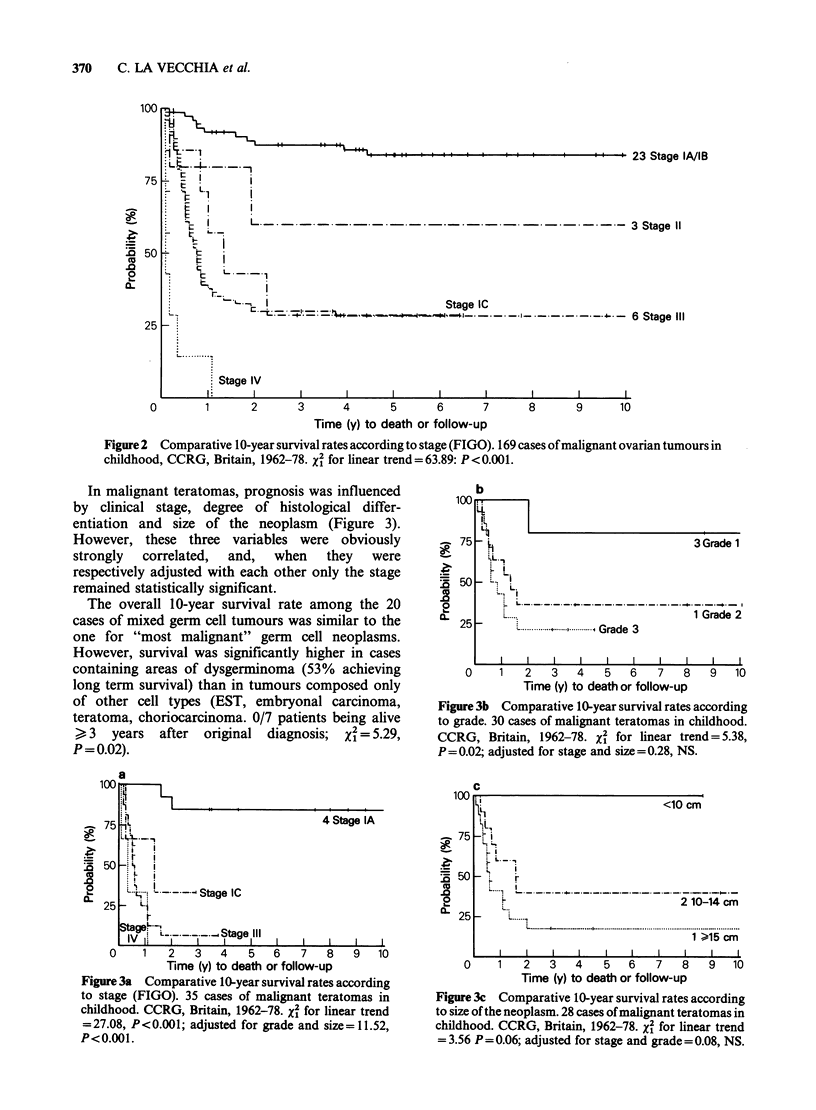
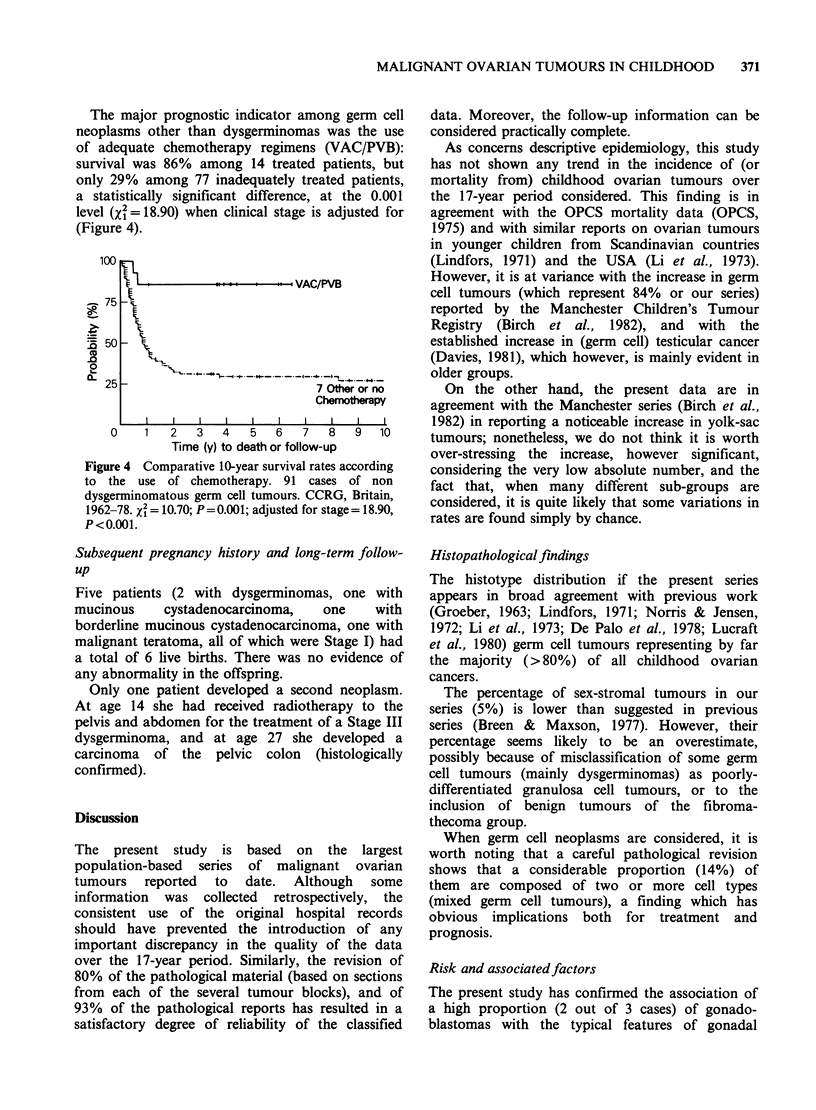
The files of the Childhood Cancer Research Group and of the Oxford Survey of Childhood Cancers were scrutinized for all the ovarian neoplasms registered in England, Scotland and Wales in children under age 15 years throughout the period 1962-78. Among 172 cases confirmed as malignant ovarian tumours, 145 (84%) were tumours of germ cell origin (54 dysgerminomas, 36 malignant teratomas, 26 endodermal sinus tumours, 4 embryonal carcinomas, 2 pure choriocarcinomas, 20 mixed germ cell neoplasms, 3 gonadoblastomas), 13 (8%) were epithelial carcinomas (3 serous or undifferentiated, 10 mucinous), 9 (5%) were sex-cord stromal tumours (3 granulosa cell, 3 Sertoli-Leydig, 3 unclassified) and 5 (3%) were other miscellaneous tumour types. Less than 10% of the neoplasms occurred at age less than 5 years, approximately 20% from 5-9, and greater than 70% from 10-14 years. Germ cell neoplasms of greater malignancy (immature teratomas, endodermal sinus tumours) occurred in a significantly higher proportion at younger age (less than 10 years) than dysgerminomas (P = 0.01). The overall incidence (approximately 1.7 cases per 10(6) per annum) did not show any noticeable trend over the 17-year period considered. The clustering of two confined cases and, possibly, a third case, of germ cell neoplasms in three generations of the same family pointed to a genetic component in the aetiology of some of these neoplasms. A large number of sex related and mental or neurological abnormalities was also reported in case children. The 10-year survival rates, determined by the life-table method were: epithelial carcinomas 73%, sex-cord stromal tumours 44%, dysgerminomas 73%, malignant teratomas 33%, endodermal sinus tumours 39%, embryonal carcinomas 25%, other germ cell neoplasms 30% and gonadoblastomas 100%. Apart from cell-type, factors associated with prognosis were clinical stage (in all types), size and degree of histological differentiation (in malignant teratomas, but only when stage was not allowed for). The adoption of efficacious polychemotherapy regimens completely changed the prognosis of germ cell tumours other than dysgerminomas (from 29% to greater than 85% disease-free survivors in the present series).
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Birch J. M., Marsden H. B., Swindell R. Pre-natal factors in the origin of germ cell tumours of childhood. Carcinogenesis. 1982;3(1):75–80. doi: 10.1093/carcin/3.1.75. [DOI] [PubMed] [Google Scholar]
- Blom G. P., Torkildsen E. M. Ovarian cystadenocarcinoma in a 4-year-old girl: report of a case and review of the literature. Gynecol Oncol. 1982 Apr;13(2):242–246. doi: 10.1016/0090-8258(82)90033-6. [DOI] [PubMed] [Google Scholar]
- Breen J. L., Maxson W. S. Ovarian tumors in children and adolescents. Clin Obstet Gynecol. 1977 Sep;20(3):607–623. doi: 10.1097/00003081-197709000-00010. [DOI] [PubMed] [Google Scholar]
- Davies J. M. Testicular cancer in England and Wales: some epidemiological aspects. Lancet. 1981 Apr 25;1(8226):928–932. doi: 10.1016/s0140-6736(81)91625-1. [DOI] [PubMed] [Google Scholar]
- De Palo G. M., Doci R., Gasparini M., Fossati-Bellani F. Malignant ovarian neoplasms in childhood. Tumori. 1978 Feb 28;64(1):33–43. doi: 10.1177/030089167806400104. [DOI] [PubMed] [Google Scholar]
- DeWolf W. C., Lange P. H., Einarson M. E., Yunis E. J. HLA and testicular cancer. Nature. 1979 Jan 18;277(5693):216–217. doi: 10.1038/277216a0. [DOI] [PubMed] [Google Scholar]
- FOX H., KAZZAZ B., LANGLEY F. A. ARGYROPHIL AND ARGENTAFFIN CELLS IN THE FEMALE GENITAL TRACT AND IN OVARIAN MUCINOUS CYSTS. J Pathol Bacteriol. 1964 Oct;88:479–488. doi: 10.1002/path.1700880211. [DOI] [PubMed] [Google Scholar]
- Fraumeni J. F., Jr, Li F. P., Dalager N. Teratomas in children: epidemiologic features. J Natl Cancer Inst. 1973 Nov;51(5):1425–1430. doi: 10.1093/jnci/51.5.1425. [DOI] [PubMed] [Google Scholar]
- GROEBER W. R. OVARIAN TUMORS DURING INFANCY AND CHILDHOOD. Am J Obstet Gynecol. 1963 Aug 15;86:1021–1035. [PubMed] [Google Scholar]
- Hecht F., McCaw B. K., Patil S. Ovarian teratomas and genetics of germ-cell formation. Lancet. 1976 Dec 11;2(7998):1311–1311. doi: 10.1016/s0140-6736(76)92084-5. [DOI] [PubMed] [Google Scholar]
- Hong S. J., Lurain J. R., Tsukada Y., Piver M. S., Humbert J. R., Freeman A. I. Cystadenocarcinoma of the ovary in a 4-year-old: benign transformation during therapy. Cancer. 1980 Apr 15;45(8):2227–2230. doi: 10.1002/1097-0142(19800415)45:8<2227::aid-cncr2820450837>3.0.co;2-#. [DOI] [PubMed] [Google Scholar]
- Jackson S. M. Ovarian dysgerminoma. Br J Radiol. 1967 Jun;40(474):459–462. doi: 10.1259/0007-1285-40-474-459. [DOI] [PubMed] [Google Scholar]
- Langley F. A., Cummins P. A., Fox H. An ultrastructural study of mucin secreting epithelia in ovarian neoplasms. Acta Pathol Microbiol Scand Suppl. 1972;233:76–86. [PubMed] [Google Scholar]
- Levey S., Grabstald H. Synchronous testicular tumors in identical twins. Urology. 1975 Dec;6(6):754–758. doi: 10.1016/0090-4295(75)90814-6. [DOI] [PubMed] [Google Scholar]
- Li F. P., Fraumeni J. F., Jr, Dalager N. Ovarian cancers in the young. Epidemiologic observations. Cancer. 1973 Oct;32(4):969–972. doi: 10.1002/1097-0142(197310)32:4<969::aid-cncr2820320431>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- Lindfors O. Primary ovarian neoplasms in infants and children. A study of 81 cases diagnosed in Finland and Sweden. Ann Chir Gynaecol Fenn Suppl. 1971;177:1–66. [PubMed] [Google Scholar]
- Norris H. J., Jensen R. D. Relative frequency of ovarian neoplasms in children and adolescents. Cancer. 1972 Sep;30(3):713–719. doi: 10.1002/1097-0142(197209)30:3<713::aid-cncr2820300319>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- Norris H. J., Zirkin H. J., Benson W. L. Immature (malignant) teratoma of the ovary: a clinical and pathologic study of 58 cases. Cancer. 1976 May;37(5):2359–2372. doi: 10.1002/1097-0142(197605)37:5<2359::aid-cncr2820370528>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Robboy S. J., Scully R. E. Ovarian teratoma with glial implants on the peritoneum. An analysis of 12 cases. Hum Pathol. 1970 Dec;1(4):643–653. doi: 10.1016/s0046-8177(70)80062-4. [DOI] [PubMed] [Google Scholar]
- Roth L. M., Nicholas T. R., Ehrlich C. E. Juvenile granulosa cell tumor: a clinicopathologic study of three cases with ultrastructural observations. Cancer. 1979 Dec;44(6):2194–2205. doi: 10.1002/1097-0142(197912)44:6<2194::aid-cncr2820440632>3.0.co;2-q. [DOI] [PubMed] [Google Scholar]
- Scully R. E. Ovarian tumors. A review. Am J Pathol. 1977 Jun;87(3):686–720. [PMC free article] [PubMed] [Google Scholar]
- Siiteri P. K. Steroid hormones and endometrial cancer. Cancer Res. 1978 Nov;38(11 Pt 2):4360–4366. [PubMed] [Google Scholar]
- Smith J. P., Rutledge F. Advances in chemotherapy for gynecologic cancer. Cancer. 1975 Aug;36(2):669–674. doi: 10.1002/1097-0142(197508)36:2+<669::aid-cncr2820360809>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- Young R. H., Scully R. E. Ovarian sex cord-stromal tumors: recent progress. Int J Gynecol Pathol. 1982;1(1):101–123. doi: 10.1097/00004347-198201000-00011. [DOI] [PubMed] [Google Scholar]


