Abstract
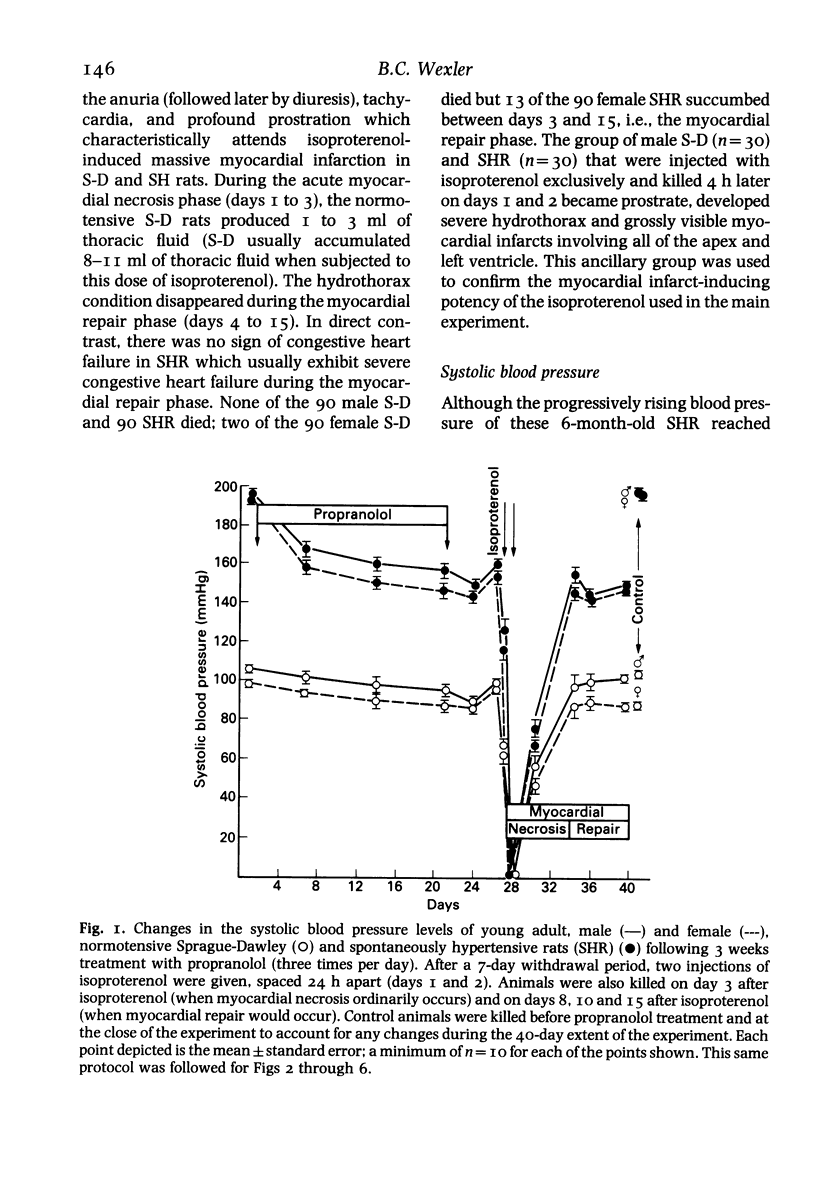
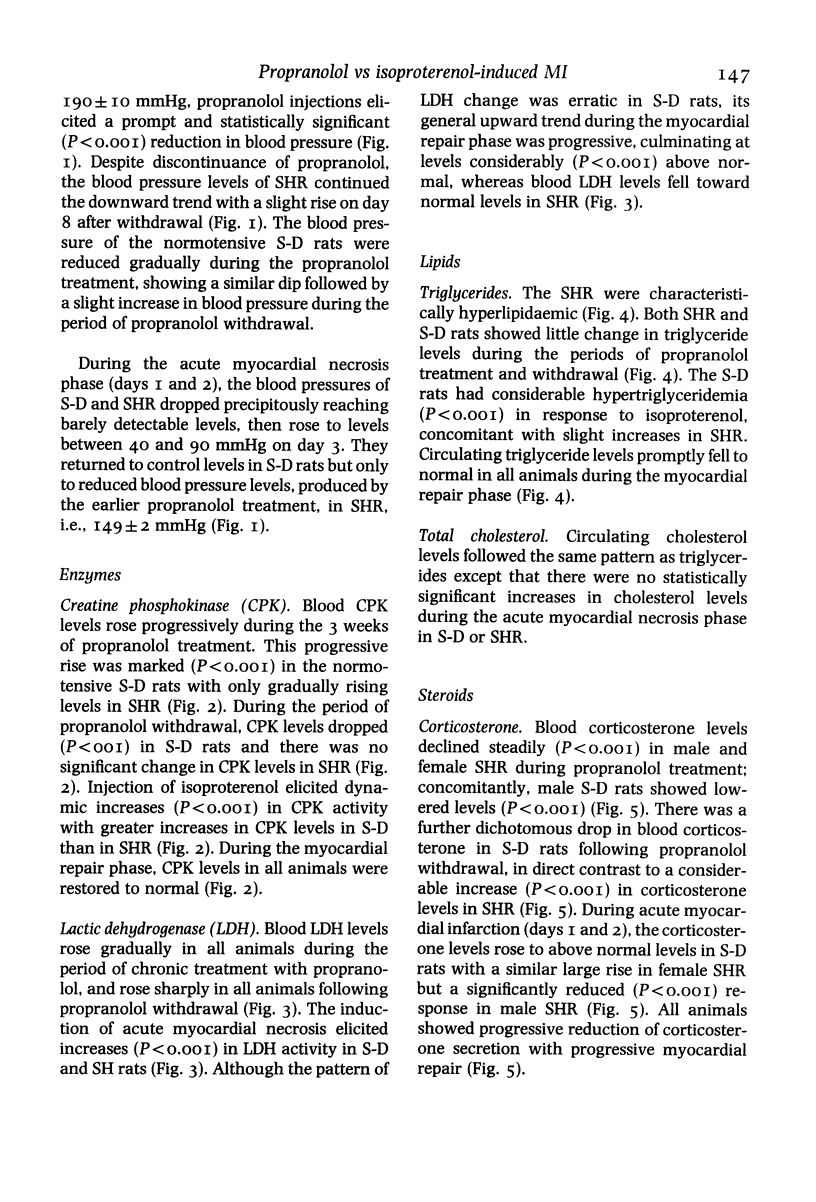
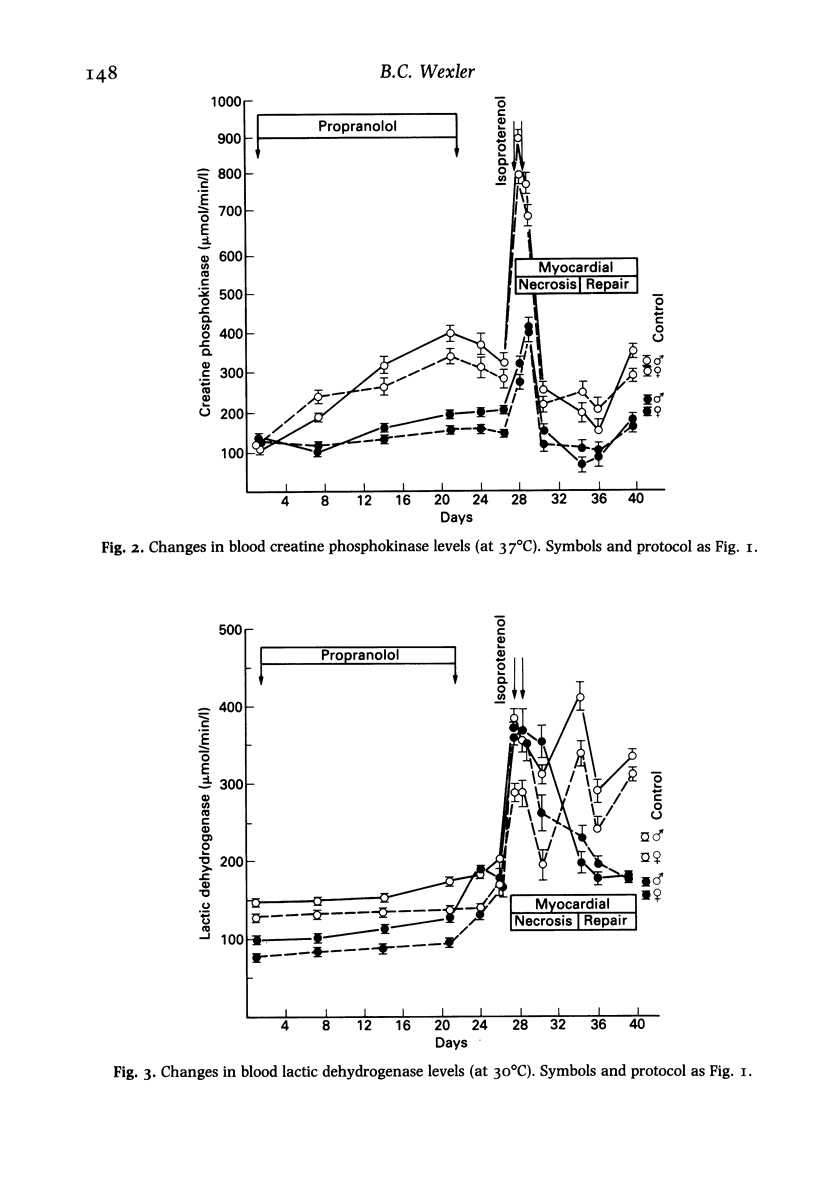
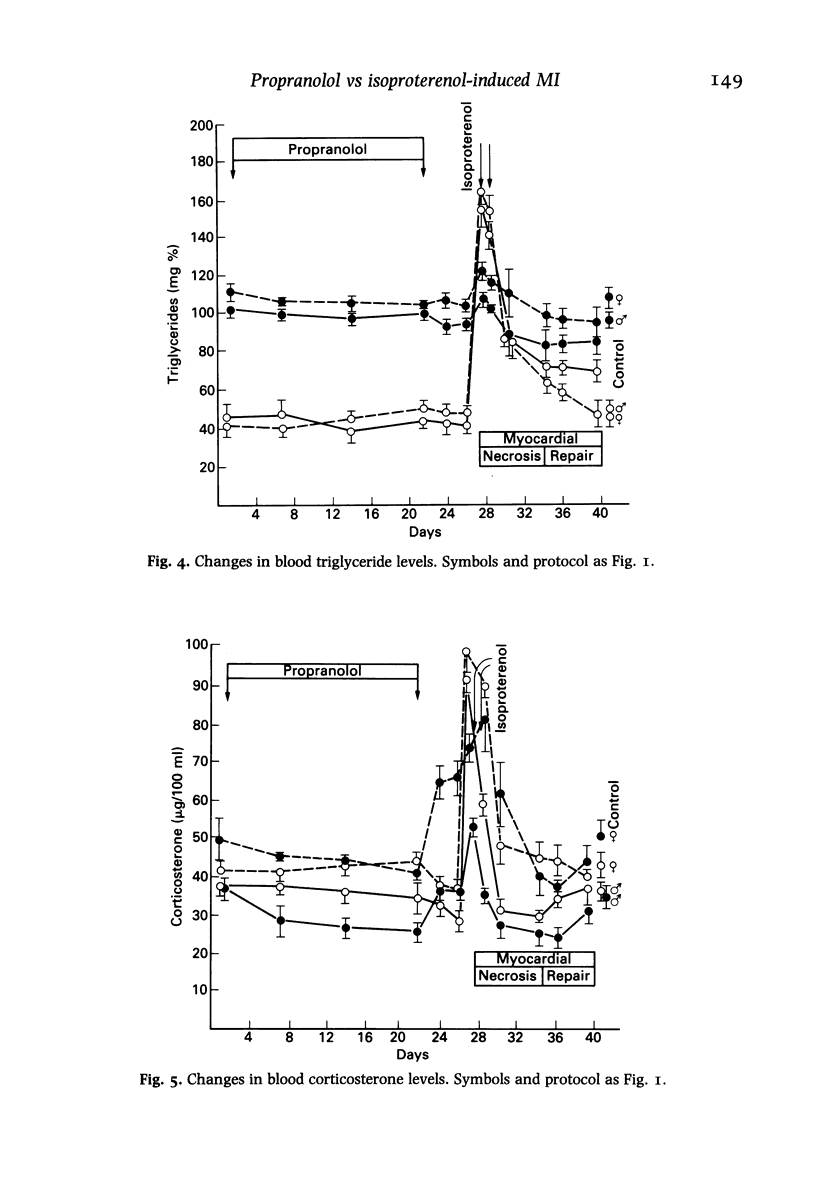
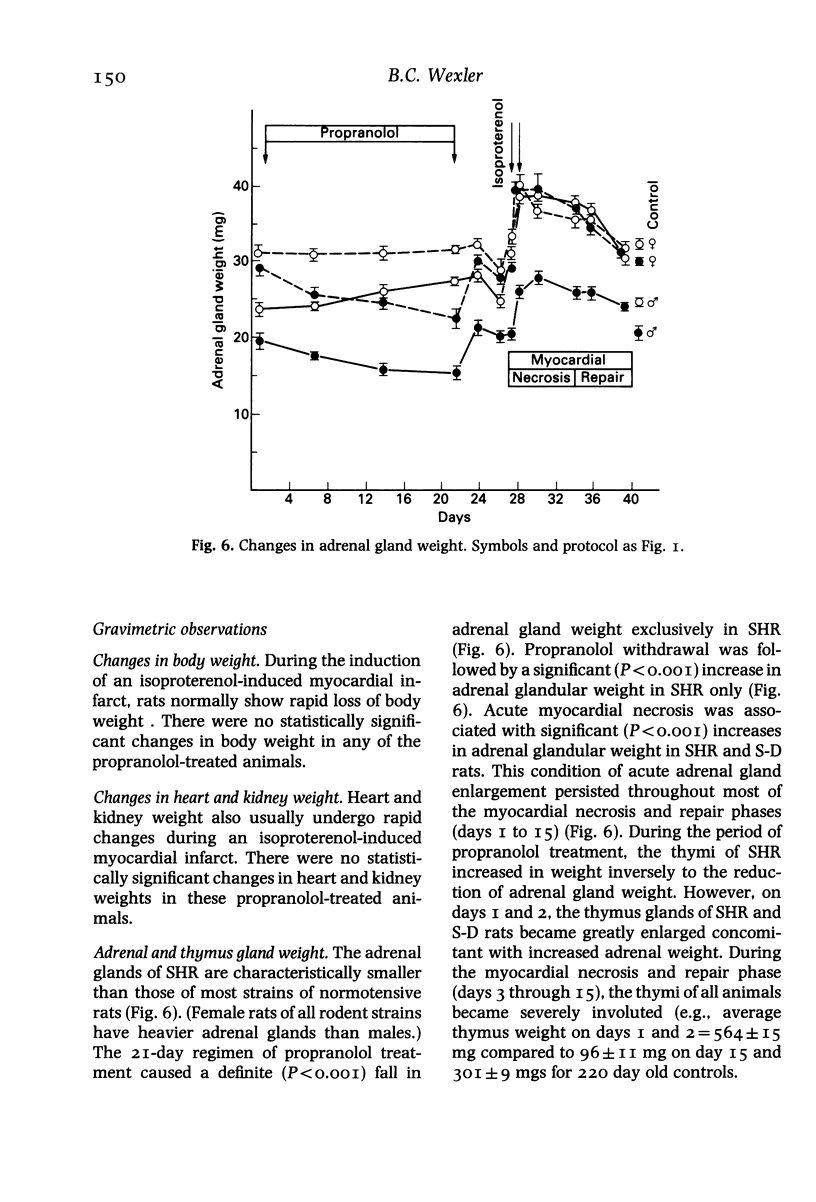
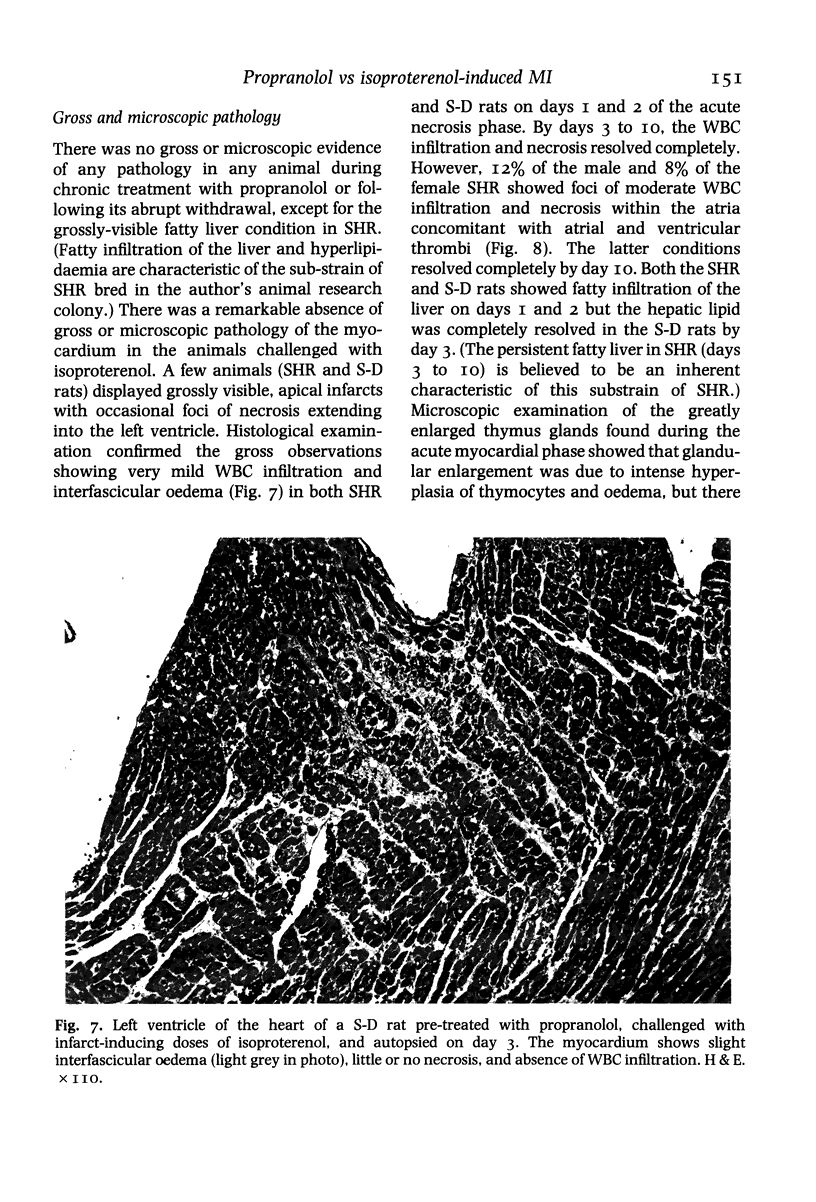
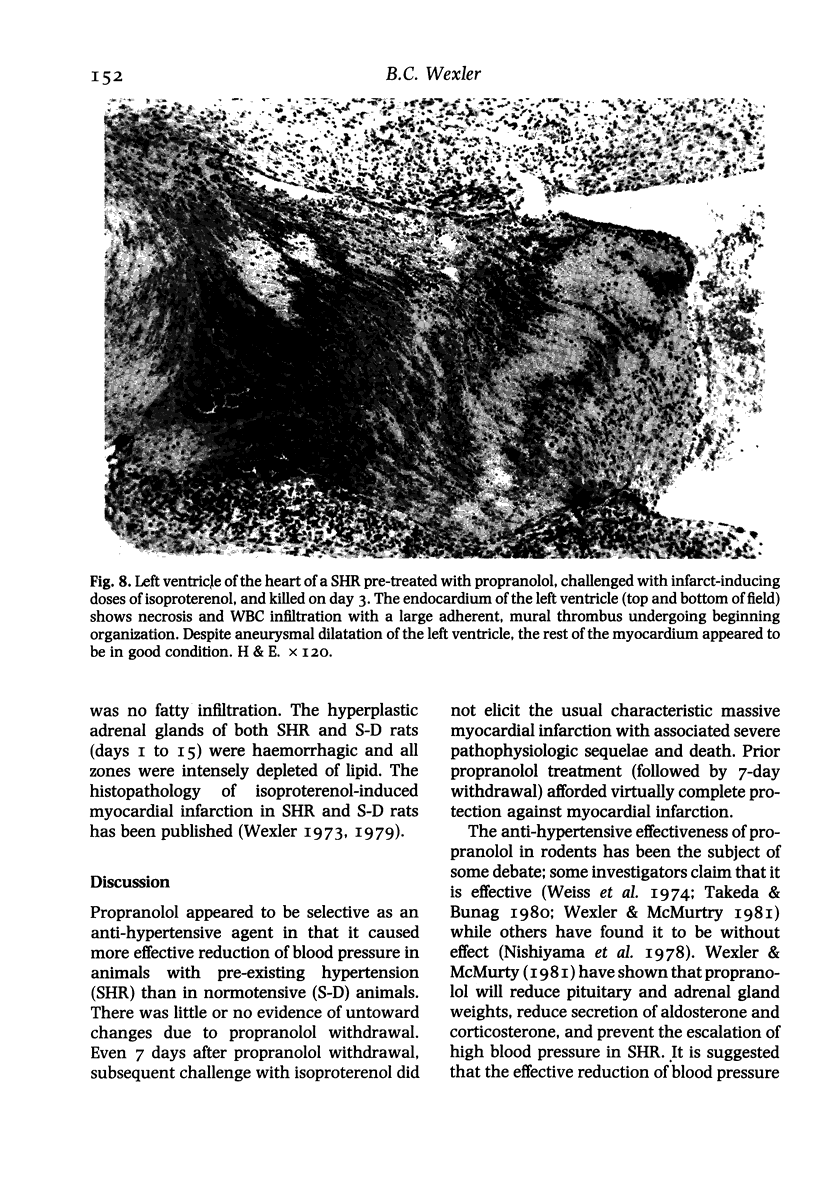
Young adult, male and female, normotensive Sprague-Dawley (S-D) and spontaneously hypertensive rats (SHR) were injected with propranolol three times daily for 3 weeks. None of the animals manifested signs of withdrawal when the injections were terminated. Seven days later, the animals were challenged with a dose of isoproterenol which would produce massive myocardial infarction and 50-60% mortality in non-treated animals. The propranolol pretreatment caused marked tranquilizing and blood pressure lowering effects in SHR exclusively. Despite the 7-day propranolol withdrawal period, very few animals died and myocardial damage was minimal. However, blood pressure levels dropped to shock-like levels, blood CPK and LDH levels showed dynamic increases, there was marked hypertriglyceridaemia, and plasma corticosterone rose to supranormal levels. Microscopically, the hearts of the propranolol pretreated animals showed little evidence of necrosis but the SHR hearts manifested large atrial and ventricular thrombi. It is suggested that in the rat, propranolol treatment causes positive myocardial protective effects mediated through hormonal and metabolic changes and propranolol withdrawal does not lead to hypersensitivity to catecholamines. In fact, the beta-blocking effects of propranolol remain effective for some time after withdrawal.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bolli P., Bühler F. R., Raeder E. A., Amann F. W., Meier M., Rogg H., Burckhardt D. Lack of beta-adrenoreceptor hypersensitivity after abrupt withdrawal of long-term therapy with oxprenolol. Circulation. 1981 Dec;64(6):1130–1134. doi: 10.1161/01.cir.64.6.1130. [DOI] [PubMed] [Google Scholar]
- Hayes A., Cooper R. G. Studies on the absorption, distribution and excretion of propranolol in rat, dog and monkey. J Pharmacol Exp Ther. 1971 Feb;176(2):302–311. [PubMed] [Google Scholar]
- Iams S. G., McMurthy J. P., Wexler B. C. Aldosterone, deoxycorticosterone, corticosterone, and prolactin changes during the lifespan of chronically and spontaneously hypertensive rats. Endocrinology. 1979 May;104(5):1357–1363. doi: 10.1210/endo-104-5-1357. [DOI] [PubMed] [Google Scholar]
- Lindenfeld J., Crawford M. H., O'Rourke R. A., Levine S. P., Montiel M. M., Horwitz L. D. Adrenergic responsiveness after abrupt propranolol withdrawal in normal subjects and in patients with angina pectoris. Circulation. 1980 Oct;62(4):704–711. doi: 10.1161/01.cir.62.4.704. [DOI] [PubMed] [Google Scholar]
- Lipson M. J., Naimi S., Proger S. Synergistic effect of propranolol and nicotinic acid on the inhibition of plasma free fatty acid release in the dog. Circ Res. 1971 Feb;28(2):270–276. doi: 10.1161/01.res.28.2.270. [DOI] [PubMed] [Google Scholar]
- Nattel S., Rangno R. E., Van Loon G. Mechanism of propranolol withdrawal phenomena. Circulation. 1979 Jun;59(6):1158–1164. doi: 10.1161/01.cir.59.6.1158. [DOI] [PubMed] [Google Scholar]
- Nishiyama K., Nishiyama A., Pfeffer M. A., Frohlich E. D. Systemic and regional flow distribution in normotensive and spontaneously hypertensive young rats subjected to lifetime beta-adrenergic receptor blockade. Blood Vessels. 1978;15(6):333–347. doi: 10.1159/000158180. [DOI] [PubMed] [Google Scholar]
- OKAMOTO K., AOKI K. Development of a strain of spontaneously hypertensive rats. Jpn Circ J. 1963 Mar;27:282–293. doi: 10.1253/jcj.27.282. [DOI] [PubMed] [Google Scholar]
- Shand D. G. Drug therapy: Propranolol. N Engl J Med. 1975 Aug 7;293(6):280–285. doi: 10.1056/NEJM197508072930606. [DOI] [PubMed] [Google Scholar]
- Takeda K., Buñag R. D. Chronic propranolol treatment inhibits sympathetic nerve activity and keeps blood pressure from rising in spontaneously hypertensive rats. Hypertension. 1980 Mar-Apr;2(2):228–235. doi: 10.1161/01.hyp.2.2.228. [DOI] [PubMed] [Google Scholar]
- Weiss L., Lundgren Y., Folkow B. Effects of prolonged treatment with adrenergic beta-receptor antagonists on blood pressure, cardiovascular design and reactivity in spontaneously hypertensive rats (SHR). Acta Physiol Scand. 1974 Aug;91(4):447–457. doi: 10.1111/j.1748-1716.1974.tb05701.x. [DOI] [PubMed] [Google Scholar]
- Wexler B. C. Isoprenaline-induced myocardial infarction in spontaneously hypertensive rats. Cardiovasc Res. 1979 Aug;13(8):450–458. doi: 10.1093/cvr/13.8.450. [DOI] [PubMed] [Google Scholar]
- Wexler B. C., McMurtry J. P. Propranolol-induced alterations in the pathophysiology of spontaneously hypertensive rats. Life Sci. 1981 Oct 5;29(14):1409–1416. doi: 10.1016/0024-3205(81)90003-5. [DOI] [PubMed] [Google Scholar]
- Wexler B. C. Pathophysiologic effects of pre-existing hypertension on isoproterenol-induced myocardial infarction in arteriosclerotic and non-arteriosclerotic rats. Atherosclerosis. 1974 Mar-Apr;19(2):161–184. doi: 10.1016/0021-9150(74)90052-5. [DOI] [PubMed] [Google Scholar]
- Wexler B. C. Protective effects of propranolol on isoproterenol-induced myocardial infarction in arteriosclerotic and non-arteriosclerotic rats. Atherosclerosis. 1973 Jul-Aug;18(1):11–42. doi: 10.1016/0021-9150(73)90114-7. [DOI] [PubMed] [Google Scholar]