Abstract
We describe a real-time PCR assay for the discrimination of azithromycin-resistant and -susceptible strains of Treponema pallidum. This assay is rapid and allows for as many as 30 clinical specimens to be analyzed simultaneously without the need for DNA sequencing.
Despite aggressive public health efforts and the long-standing availability of effective pharmacological treatments, syphilis infections persist worldwide. Strategies designed to eliminate Treponema pallidum infections include the facilitation of expanded testing and screening and the development of expanded treatment options. While the standard treatment for syphilis includes the intramuscular injection of penicillin G benzathine, investigations of treatment alternatives revealed that a single dose of oral azithromycin was as effective as both penicillin G and doxycycline for the treatment of syphilis in humans (1, 2, 7, 11, 13, 18, 22). Utilized in various locales throughout the world from 1994 to 2000, azithromycin (taken orally) is an attractive treatment option for syphilis due to its efficacy, ease of use, and relative lack of side effects; azithromycin has also been prescribed prophylactically for the treatment of incubating syphilis (14). Widespread use of azithromycin for the treatment of syphilis has resulted in the emergence of strains resistant to the antibiotic (12). Studies have shown that in San Francisco, the prevalence of azithromycin-resistant T. pallidum rose from 0% in the year 2000 to 56% in 2004 (12, 14).
The mutation shown to be associated with resistance of Treponema pallidum to macrolides, an A-to-G mutation at position 2058 in the 23S rRNA gene, alters the active site of macrolides on ribosomes (14). Comparable mutations have been seen in several other bacterial species in response to macrolide treatment (19, 23). Initial efforts to screen bacterial strains for macrolide resistance involved the cloning and DNA sequencing of the 23S rRNA genes of suspicious isolates. For certain bacterial species, several simplified molecular assays have since been developed (3, 6, 16, 20, 21). For the analysis of azithromycin resistance in T. pallidum, an assay for the simplified detection of the A2058G mutation through the use of PCR and subsequent restriction enzyme digestion was developed (12). We sought to improve incrementally the detection of the A2058G mutation in T. pallidum. To accomplish this, we have developed a real-time PCR assay that amplifies the relevant portion of the 23S rRNA gene of T. pallidum and, through the use of melting-curve-based analysis, allows for the discrimination of wild-type (2058A) and resistant (2058G) strains of T. pallidum. This assay possesses a sensitivity that is equivalent to that of the previously described PCR-based assay for azithromycin resistance detection but can be performed more rapidly and without the sometimes subjective process of agarose gel-based analysis.
Primers and probes were designed to amplify and detect the relevant portion of the T. pallidum 23S rRNA gene with the aid of LightCycler Probe Design software version 2.0 (Roche, Indianapolis, IN). A set of probes and primers recommended by the software was selected and analyzed by BLAST. The sense primer was confirmed to be 100% homologous to the relevant portion of the 23S rRNA gene of T. pallidum and was designed (and confirmed by BLAST) to have three base-pair mismatches with the corresponding 23S rRNA gene of Treponema denticola. The antisense amplification primer possesses 100% homology to the 23S rRNA gene of T. pallidum but possesses two base-pair mismatches with the corresponding sequence in T. denticola. One of these mismatches, a base mismatch at the 3′ end of the antisense primer, exists between this primer and the corresponding sequence in T. denticola, essentially eliminating the possibility of DNA extension of that primer when T. denticola is the target. The designed hybridization probes were found to have 100% homology only to the relevant portion of the T. pallidum 23S rRNA gene. The anchor and sensor hybridization probes possess perfect base-pair complementarities with the azithromycin-resistant (2058G) allele of the 23S rRNA gene of T. pallidum; however, the sensor probe possesses a 1-base-pair mismatch with the azithromycin-susceptible allele (2058A). The destabilization caused by the mismatch was predicted to be readily discernible by melting-curve analysis, allowing for discrimination between the 2058A and 2058G alleles. The primers and probes used were as follows (synthesized by Sigma-Proligo, The Woodlands, TX): forward primer, 5′-GACTCTGGACACTGTCTCG; reverse primer, 5′-GGGTGGTATTTCACTGTTG; sensor probe, 5′-LCRed 640-GTCTTCCCGTCTAACTATGGGTAAC-phosphate (underlining indicates the base that hybridizes at position 2058 of the 23S rRNA gene); and anchor probe, 5′-ATAGTAAGCTACGGTGAAGGTTCACG-fluorescein. They were designed with the following conditions considered during computational design: a 1.2 mM concentration of each deoxynucleoside triphosphate, 4 mM MgCl2, and a total monovalent cation concentration of 20 mM. These were the conditions that were ultimately utilized for real-time PCR and were established using LightCycler FastStart DNA Master HybProbe mix (Roche) per the manufacturer's recommendations for 20-μl reaction volumes in LightCycler capillaries (Roche). The primers were utilized at final concentrations of 0.5 μM and probes at 0.2 μM. Thermal cycling conditions were as follows: an initial denaturation step for 10 min at 95°C, followed by 10 “touchdown” amplification cycles whereupon cycling would occur at 95°C for 5 s, followed by annealing at 65°C for 20 s and extension at 72°C for 15 s. For each of the first five touchdown cycles, the annealing temperature was lowered by 1°C and the final five cycles were executed at 60°C annealing. After touchdown, 35 cycles were carried out under the following conditions: 95°C for 5 s, 55°C for 20 s, and 72°C for 15 s. A melting-curve step followed the amplification steps as follows: 95°C for 1 s, followed by cooling to 40°C, and constant monitoring of fluorescence as heating occurred to a peak of 80°C at the rate of 0.05°C/s. A final cooling step was included (30 s at 40°C). The touchdown cycles described above were designed to enrich for highly specific products in the early amplification steps (5).
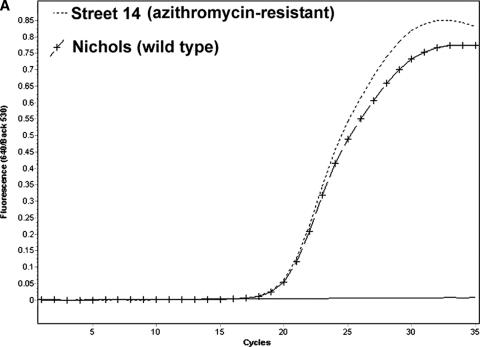
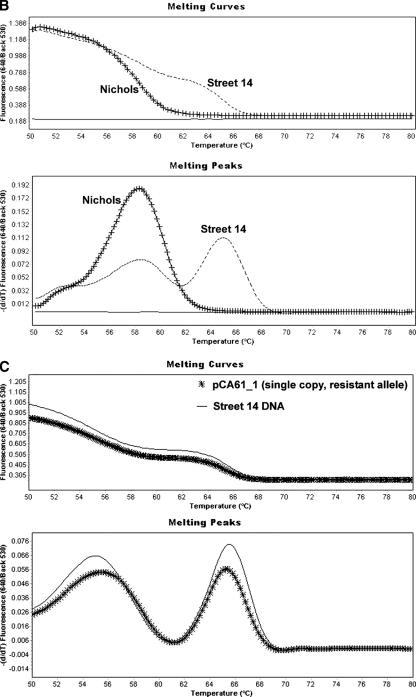
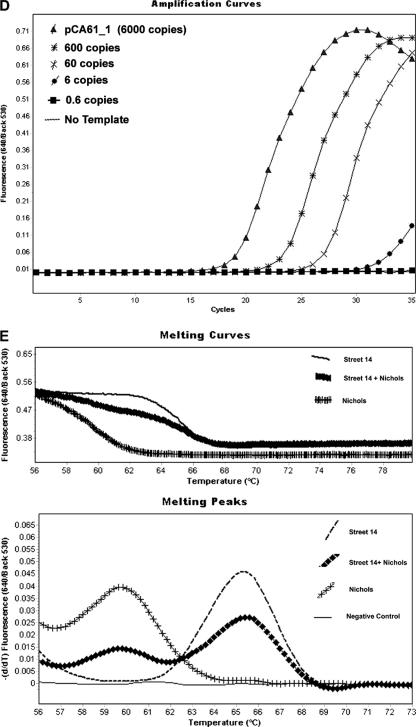
Purified total DNA extracts of samples of the T. pallidum Nichols (azithromycin-susceptible) strain and the T. pallidum Street 14 (azithromycin resistant) strain propagated in rabbits were prepared either by automated nucleic acid extraction or by preparation methods previously described (12). As shown in Fig. 1A, the real-time PCR assay was capable of detecting nucleic acid from either the susceptible or resistant strains of T. pallidum. Analysis of each amplification product by melting-curve generation revealed that resistant and susceptible strain sequences could be readily discriminated. Azithromycin-resistant Street 14 DNA resulted in PCR products that possessed a probe melting-curve peak of approximately 65°C, whereas azithromycin-susceptible Nichols DNA resulted in a PCR product with a probe melting-curve peak at 58°C (Fig. 1B). The existence of an additional, lower-temperature peak for the resistant strain was not expected, and the temperature of this secondary peak varied from experiment to experiment. Given the similarity of the lower-temperature peaks to the peak associated with wild-type (azithromycin-susceptible) T. pallidum, it was considered either that contamination of resistant-strain DNA had somehow occurred during the extraction or that the diploid nature of the 23S rRNA gene in T. pallidum might have resulted in heterozygosity of the resistant strain. To explore both hypotheses, we performed the real-time PCR assay using dilutions of a target plasmid that contained a single copy of the azithromycin-resistant 23S rRNA allele from T. pallidum. When used as a target, this purified plasmid DNA also generated dual peaks (Fig. 1C) in the melting-curve phase (identical to that seen with Street 14 DNA) of the real-time assay. Hence, neither heterozygosity nor contamination of the wild-type sequence can explain the dual-peak phenomenon observed with azithromycin-resistant strains. This dual-peak phenomenon was not found to be present with a different lot number of probes synthesized and utilized at another laboratory site where the real-time assay was evaluated (data not shown). In that case, all other reaction conditions were identical to those described herein. We therefore conclude that this dual-peak phenomenon found in the melting-curve peaks of resistant strains in based upon the quality of the probe synthesis. Clearly, however, the assay as described herein has been found to consistently and easily discern between wild-type and azithromycin-resistant strains of T. pallidum. Real-time PCR using quantitated dilutions of the plasmid described above revealed that as few as 6 copies of the azithromycin-resistant 23S rRNA gene were detectable by this real-time PCR assay (Fig. 1D).
FIG. 1.
(A) Real-time PCR amplification using genomic DNA from azithromycin-susceptible (Nichols) and azithromycin-resistant (Street 14) strains of T. pallidum as targets. (B) Melting curves and melting-curve peaks of azithromycin-susceptible and -resistant strains of T. pallidum. The hybridization probes possess perfect complementarity with the azithromycin-resistant allele of the T. pallidum 23S rRNA gene, resulting in higher melting temperatures than when the probes are bound to the azithromycin-susceptible allele. (C) Melting curves and melting-curve peaks of whole DNA from T. pallidum Street 14 (an azithromycin-resistant strain) and of plasmid DNA containing a single copy of the azithromycin-resistant 23S rRNA allele from T. pallidum (pCA61_1). (D) Amplification curves using target nucleic acid which has been quantitated. Dilutions of a plasmid (pCA61_1) containing a single copy of the azithromycin-resistant 23S rRNA gene were used as reactants in the real-time PCR assay. (E) Melting curve and melting-curve peaks derived from amplification of an equimolar mixture of chromosomal DNA from the Street 14 and Nichols strains of T. pallidum.
Since the 23S rRNA gene is diploid in Treponema pallidum, it is important to consider that certain strains that are heterozygous for resistance to azithromycin may exist. Therefore, we further assessed the real-time PCR assay for its ability to discern such heterozygous strains. Because we could not identify any source of such a heterozygous strain with which to test the real-time PCR assay, we simulated the existence of such a strain. This was achieved by combining equimolar proportions of chromosomal DNA from both the Nichols and Street 14 strains. The equimolar solution of DNA was then used as a target for the real-time PCR assay. The results of this experiment, shown in Fig. 1E, indicated that such heterozygotes may be discernible by this assay, as both the higher-temperature and lower-temperature peaks associated with Street 14 and Nichols, respectively, are visible on the same curve, which is a curve that is apparently distinct from the curves generated by either homozygote.
The goal of the development of this assay was to facilitate the screening of large numbers of known T. pallidum-containing specimens for their azithromycin susceptibility genotype. Hence we sought to evaluate the ability of the real-time assay to discern T. pallidum azithromycin susceptibility in 91 dark-field-microscopy-positive genital swab specimens (with their identities masked) collected from 2000 through 2005 in a San Francisco municipal sexually transmitted disease clinic. The azithromycin susceptibility genotypes of these clinical specimens was assessed by a previously verified assay method which involves PCR followed by restriction digestion analysis of the amplicon (12). Swabs from genital lesions were placed in lysis buffer (10 mM Tris [pH 8.0], 0.1 M EDTA, 0.5% sodium dodecyl sulfate [pH 8.0]) (500 μl) and were subjected to automated nucleic acid extraction (MagNAPure LC; Roche) prior to being analyzed by real-time PCR. The real-time PCR assay was capable of detecting T. pallidum DNA in the extracts from lysates of 79 of 91 (87%) dark-field-microscopy-positive specimens, while the reference assay was capable of detecting T. pallidum DNA in 72 of 91 specimens (80%). For the 72 specimens which reacted positively for T. pallidum by both assays, assessment of azithromycin susceptibility using real-time PCR and melting-curve generation agreed with the data generated by the reference assay in 72 out of 72 (100%) specimens. These data indicate that the real-time PCR method for assessment of azithromycin susceptibility in T. pallidum is as accurate as the previously described PCR-based method and is perhaps more sensitive. Moreover, the time required to perform the real-time PCR assay, requiring approximately 4 h for the complete analysis of 30 specimens, is much shorter than that of the reference assay.
The primary intent of this assay is to facilitate the screening of known-positive T. pallidum specimens with regard to their azithromycin susceptibility. Secondarily, this assay might be utilized to detect T. pallidum in cases where dark-field microscopy is unavailable. With this in mind, we sought to evaluate the specificity of the real-time PCR. To do this, we tested whether the flora associated with the rectum, mouth, and genitalia (male) of human specimens might be detectable by this real-time assay. The identities of 20 rectal swabs taken as part of a regional screening effort for Neisseria gonorrhea and Chlamydia trachomatis were masked, and the swabs were subjected to nucleic acid extraction and subsequent analysis by the real-time PCR assay. None of the 20 rectal specimens were found to be T. pallidum positive by the real-time PCR assay. To evaluate the potential for oral treponemal flora to be spuriously detected, we also performed the real-time PCR assay on extracts from 23 dental-gingival swabs. Of the 23 oral specimens, 2 specimens demonstrated some minor reactivity using the real-time PCR assay, but both specimens generated odd melting-curve signatures that did not overlap with that of either the Nichols strain or Street 14 strain DNA controls (data not shown). Purified total nucleic acid from both Treponema denticola (80 ng) and Treponema pectinovorum (265 ng) was used as a target for this real-time assay to discern whether the real-time assay described herein would react with them. Nucleic acid from neither organism demonstrated amplification with this real-time PCR assay. Additionally, 28 swabs of genital (male) ulcerations that were determined to be positive for herpes simplex virus type 1 or 2 and dark field negative for spirochetes were analyzed by this real-time assay. Of the 28 genital ulceration specimens, none were reactive by real-time PCR assay. While these assessments of specificity were by no means exhaustive, it should be emphasized that the primary functionality of this assay should be reserved for rapid assessment of azithromycin susceptibility in known-positive T. pallidum specimens and not as a primary means of detection or diagnosis. Other real-time assays, recently developed and described in the published literature, may be better suited for such duty (4, 8, 9, 10, 15, 17). We currently utilize the assay described herein in conjunction with the detection assay recently published by Leslie et al. (9).
Acknowledgments
We thank Jacques Izard for provision of treponemal chromosomal DNA and Sally Liska, Brian Louie, and Leah Rauch of the San Francisco Department of Public Health Laboratory for their support of this project.
Footnotes
Published ahead of print on 9 July 2007.
REFERENCES
- 1.Bowden, F. J., B. Farmer, J. Bullen, V. Chamberlain, and I. Bastian. 1995. Azithromycin and syphilis. Genitourin. Med. 71:196-197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Campos-Outcalt, D., S. Hurwitz, and T. Mickey. 2002. Use of directly observed azithromycin treatment for syphilis in a homeless woman. Sex. Transm. Dis. 29:372. [DOI] [PubMed] [Google Scholar]
- 3.Canu, A., A. Abbas, B. Malbruny, F. Sichel, and R. Leclercq. 2004. Denaturing high-performance liquid chromatography detection of ribosomal mutations conferring macrolide resistance in gram-positive cocci. Antimicrob. Agents Chemother. 48:297-304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chen, C. Y., K. H. Chi, R. W. George, D. L. Cox, A. Srivastava, M. R. Silva, F. Carneiro, G. Y. Lauwers, and R. C. Ballard. 2006. Diagnosis of gastric syphilis by direct immunofluorescence staining and real-time PCR testing. J. Clin. Microbiol. 44:3452-3456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Don, R. H., P. T. Cox, B. J. Wainwright, K. Baker, and J. S. Mattick. 1991. ‘Touchdown’ PCR to circumvent spurious priming during gene amplification. Nucleic Acids Res. 19:4008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haanpera, M., P. Huovinen, and J. Jalava. 2005. Detection and quantification of macrolide resistance mutations at positions 2058 and 2059 of the 23S rRNA gene by pyrosequencing. Antimicrob. Agents Chemother. 49:457-460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hook, E. W., III, D. H. Martin, J. Stephens, B. S. Smith, and K. Smith. 2002. A randomized, comparative pilot study of azithromycin versus benzathine penicillin G for treatment of early syphilis. Sex. Transm. Dis. 29:486-490. [DOI] [PubMed] [Google Scholar]
- 8.Koek, A. G., S. M. Bruisten, M. Dierdorop, A. P. van Dam, and K. Templeton. 2006. Specific and sensitive diagnosis of syphilis using a real-time PCR for Treponema pallidum. Clin. Microbiol. Infect. 12:1233-1236. [DOI] [PubMed] [Google Scholar]
- 9.Leslie, D. E., F. Azzato, T. Karapanagiotidis, J. Leydon, and J. Fyfe. 2007. Develpment of a real-time PCR assay to detect Treponema pallidum in clinical specimens and assessment of the assay's performance by comparison with serological testing. J. Clin. Microbiol. 45:93-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu, H., B. Rodes, C. Y. Chen, and B. Steiner. 2001. New tests for syphilis: rational design of a PCR method for detection of Treponema pallidum in clinical specimens using unique regions of the DNA polymerase I gene J. Clin. Microbiol. 39:1941-1946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lukehart, S. A., M. J. Fohn, and S. A. Baker-Zander. 1990. Efficacy of azithromycin for therapy of active syphilis in the rabbit model. J. Antimicrob. Chemother. 25(Suppl. A):91-99. [DOI] [PubMed] [Google Scholar]
- 12.Lukehart, S. A., C. Gordones, B. J. Molini, P. Sonnett, S. Hopkins, F. Mulcahy, J. Engelman, S. J. Mitchell, A. M. Rompalo, C. M. Marra, and J. D. Klausner. 2004. Macrolide resistance in Treponema pallidum in the United States and Ireland. N. Engl. J. Med. 351:154-158. [DOI] [PubMed] [Google Scholar]
- 13.Mashkilleyson, A. L., M. A. Gemberg, N. Mashkilleyson, and S. A. Kutin. 1996. Treatment of syphilis with azithromycin. Int. J. STD AIDS 7(Suppl. 1):13-15. [DOI] [PubMed] [Google Scholar]
- 14.Mitchell, S. J., J. Engelman, C. K. Kent, S. A. Lukehart, C. Gordones, and J. D. Klausner. 2006. Azithromycin-resistant syphilis infection: San Francisco, California, 2000-2004. Clin. Infect. Dis. 42:337-345. [DOI] [PubMed] [Google Scholar]
- 15.Muller, M., I. Ewert, F. Hansmann, C. Tiemann, H. J. Hagedorn, W. Solbach, J. Roider, B. Nolle, H. Lagua, and H. Hoerauf. 15 November 2006. Detection of Treponema pallidum in the vitreous by PCR. Br. J. Ophthalmol. [Epub] doi: 10.1136/bjo.2006.110288. [DOI] [PMC free article] [PubMed]
- 16.Niwa, H., T. Chuma, K. Okamoto, and K. Itoh. 2003. Simultaneous detection of mutations associated with resistance to macrolides and quinolones in Camplylobacter jejuni and C. coli using a PCR-line probe assay. Int. J. Antimicrob. Agents 22:374-379. [DOI] [PubMed] [Google Scholar]
- 17.Rajan, M. S., P. Pantelidis, C. Y. Tong, G. L. French, E. M. Graham, and M. R. Stanford. 2006. Diagnosis of Treponema pallidum in vitreous samples using real time polymerase chain reaction. Br. J. Ophthalmol. 90:647-648. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Riedner, G., M. Rusizoka, J. Todd, L. Maboko, M. Hoelscher, D. Mmbando, E. Samky, E. Lyamuya, D. Mabey, H. Grosskurth, and R. Hayes. 2005. Single-dose azithromycin versus penicillin G benzathine for the treatment of early syphilis. N. Engl. J. Med. 353:1236-1244. [DOI] [PubMed] [Google Scholar]
- 19.Stamm, L. V., and H. L. Bergen. 2000. A point mutation associated with bacterial macrolide resistance is present in both 23S rRNA genes of an erythromycin-resistant Treponema pallidum clinical isolate. Antimicrob. Agents Chemother. 44:806-807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vacher, S., A. Menard, E. Bernard, A. Santos, and F. Megraud. 2005. Detection of mutations associated with macrolide resistance in thermophilic Camplylobacter spp. by real-time PCR. Microb. Drug Resist. 11:40-47. [DOI] [PubMed] [Google Scholar]
- 21.van Doorn, L.-J., Y. J. Debets-Ossenkopp, A. Marais, R. Sanna, F. Mégraud, J. G. Kusters, and W. G. V. Quint. 1999. Rapid detection, by PCR and reverse hybridization, of mutations in the Helicobacter pylori 23S rRNA gene, associated with macrolide resistance. Antimicrob. Agents Chemother. 43:1779-1782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Verdon, M. S., H. H. Handsfield, and R. B. Johnson. 1994. Pilot study of azithromycin for treatment primary and secondary syphilis. Clin. Infect. Dis. 19:486-488. [DOI] [PubMed] [Google Scholar]
- 23.Vester, B., and S. Douthwaite. 2001. Macrolide resistance conferred by base substitutions in 23S rRNA. Antimicrob. Agents Chemother. 45:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]