Abstract
Borna disease virus (BDV) is a highly neurotropic, noncytolytic virus. Experimentally infected B10.BR mice remain healthy unless specific antiviral T cells that infiltrate the infected brain are triggered by immunization. In contrast, infected MRL mice spontaneously mount an antiviral T-cell response that can result in meningoencephalitis and neurological disease. The antiviral T cells may, alternatively, eliminate the virus without inducing disease if they are present in sufficient numbers before the virus replicates to high titers. Since the immune response of H-2k mice is directed mainly against the epitope TELEISSI located in the viral nucleoprotein N, we generated BDV mutants that feature TQLEISSI in place of TELEISSI. We show that adoptive transfer of BDV N-specific CD8 T cells induced neurological disease in B10.BR mice persistently infected with wild-type BDV but not with the mutant virus expressing TQLEISSI. Surprisingly, the mutant virus replicated less well in adult MRL wild-type mice than in mutant mice lacking mature CD8 T cells. Furthermore, when MRL mice were infected with the TQLEISSI-expressing BDV mutant as newborns, neurological disease was observed, although at a lower rate and with slower kinetics than in mice infected with wild-type virus. These results confirm that TELEISSI is the major CD8 T-cell epitope in H-2k mice and suggest that unidentified minor epitopes are present in the BDV proteome which are recognized rather efficiently by antiviral T cells if the dominant epitope is absent.
Virus mutants escaping control by antiviral CD8 T cells were first shown to arise in lymphocytic choriomeningitis virus (LCMV)-infected T-cell receptor-transgenic mice (30). Similar results were later obtained with influenza A virus in T-cell receptor-transgenic mice (33). Virus variants with mutations affecting CD8 T-cell epitopes were reported to accumulate in monkeys infected with simian immunodeficiency virus (SIV) (6, 28) and in mice infected with mouse hepatitis virus (17, 26, 27). Mutation of CD8 T-cell epitopes can lead to increased virus titers in immune animals (6, 28) and may thus contribute to morbidity and mortality resulting from virus infection. Similarly, viruses escaping control by CD8 T cells were observed in humans infected with human immunodeficiency virus (8) and hepatitis C virus (10).
Borna disease virus (BDV) is an enveloped virus with a single-stranded RNA genome of negative polarity (3, 4, 40). It is a highly neurotropic virus that can establish noncytolytic persistent infections of the central nervous system (CNS) in a wide variety of vertebrate species (19, 38). The recovery of recombinant BDV from plasmid-encoded full-length viral cDNA was recently established (20, 41). Most tissue culture-adapted laboratory strains of BDV do not replicate efficiently in infected mice but can be adapted to replicate in the mouse CNS by serial passage in this organ (1, 11, 16, 24). Recent experiments showed that two mutations in the polymerase L (LRD) enable recombinant BDV strain He/80 to replicate in the CNS of mice. An additional mutation in the viral phosphoprotein P (PK) was required for vigorous virus replication and disease induction in H-2k mice (1).
Studies of rodents and naturally infected horses indicated that BDV-induced neurological disease represents a CD8 T-cell-mediated immunopathology that is dependent on CD4 T-cell help (2, 11, 25, 31, 36, 37, 42, 44; K. Baur, M. Rauer, K. Richter, J. Goetz, J. Hausmann, and P. Staeheli, submitted for publication). Besides inducing immunopathology, CD8 T cells restrict the propagation of BDV if present in sufficient amounts before the virus has massively spread throughout the CNS (12). MRL mice infected as newborns are highly susceptible to BDV-induced neurological disease (11). By contrast, BDV-infected B10.BR mice, which are of H-2k haplotype like MRL mice, develop a nonsymptomatic persistent infection due to immunological ignorance of BDV antigens (13). Neurological disease can be induced in persistently infected B10.BR mice by immunization with a vaccinia virus vector expressing the nucleoprotein N of BDV (13). The N protein of BDV is expressed in large amounts in the brains of infected animals (19). It represents the major target of antiviral CD8 T cells in mice (13, 39) and rats (32). The major CD8 T-cell epitope of H-2k mice was mapped to amino acids 129 to 136 of the N protein and has the amino acid sequence TELEISSI (39). The majority of CD8 T cells isolated from the brains of diseased mice specifically recognize the TELEISSI epitope (5, 39), indicating that CD8 T cells with this specificity also mediate immunopathology.
Here we describe a mouse-adapted variant of BDV that lacks the TELEISSI epitope. This virus was no longer recognized by TELEISSI-specific CD8 T cells and showed reduced pathology compared to the parental BDV strain.
MATERIALS AND METHODS
Plasmid constructions.
The E130Q mutation in the N gene of constructs pBRPol II-HrBDVc-LRD and pBRPol II-HrBDVc-PKLRD (1) was generated by changing the codon GAG to CAA. Site-directed mutagenesis PCR was performed with proofreading Turbo Pfu DNA polymerase (Stratagene) and standard reaction conditions in a GeneAmp PCR cycler 9600 (Applied Biosystems). The integrity of all PCR-derived DNA fragments was verified by sequencing. All restriction digestions of plasmids and PCR fragments were performed using commercially available enzymes (New England Biolabs or Fermentas). Ligation reactions were done using 2.5 Weiss units of bacteriophage T4 DNA ligase (Fermentas) in a total volume of 5 μl. The ligation reaction mixtures were incubated at 16°C for at least 2 h and then used to transform 50 μl of competent Top10 bacteria (Invitrogen). Primer sequences and details of the cloning strategies are available upon request.
Generation of recombinant BDV.
The virus was recovered from cDNA as described previously (20, 41).
BDV stocks.
Virus stocks were prepared from persistently infected Vero cells as described previously (3). The stocks were dialyzed for 2 days against phosphate-buffered saline and then titrated on Vero cells.
RNA isolation and reverse transcription (RT)-PCR.
RNA was isolated from infected Vero cell cultures with peqGOLD TriFast (PeqLab Biotechnologie, Erlangen, Germany) as recommended by the manufacturer. Two micrograms of total RNA was reverse transcribed using random hexamer primers and an H-minus first-strand cDNA synthesis kit (Fermentas) according to the manufacturer's protocol. PCR primers 763- (5′-TAG TCA TCT GCG CAT AAC-3′) and 1+ (5′-TGT TGC GTT AAC AAC AAA C-3′) were used to amplify fragments carrying the introduced mutation.
For the detection of BDV by LightCycler PCR, a LightCycler RNA master hybridization probe kit (Roche), primers 5′-CAT GGT GAG ACT GCT ACA C-3′ and 5′-CTC AAA GTC TGT AGT TAG TAG-3′, and probe 5′-6FAM-ATC CAA TCT ATA GCC TCA TGT GGT-TAMRA-3′ were used.
Mice.
MRL/MpJ (MRL), MRL β2-microglobulin0/0 (β2 m0/0) and B10.BR mice were originally purchased from The Jackson Laboratory (Bar Harbor, ME). C57BL/6 mice lacking a functional type I interferon system (IFNAR10/0) (22) were originally provided by U. Kalinke, Langen, Germany. MRL mice deficient for gamma interferon were previously described (14). Breeding colonies were maintained in our local animal facility. All animal experiments were approved by the local authorities.
Viruses and animal infections.
MRL and B10.BR mice were infected by intracerebral injection into the thalamic region of the left brain hemisphere of 10-μl samples containing 104 focus-forming units (FFU) of recombinant BDV, using a Hamilton syringe. For immune priming, B10.BR mice were injected intramuscularly with 2 × 106 PFU of recombinant parapoxvirus ovis strain D1701-VrV-p40 expressing BDV N (15). N-specific immunity was boosted 1 week later by infecting the animals intraperitoneally with 2 × 107 PFU of recombinant vaccinia virus expressing BDV N (13). Two weeks after the booster immunization, mice were sacrificed and splenocytes were isolated for the restimulation of N-specific CD8 T cells.
Fluorescence microscopy.
Cells were fixed for 10 min in 3% paraformaldehyde and permeabilized for 5 min in phosphate-buffered saline containing 0.5% Triton X-100. The virus antigen was detected as described previously (43).
Western blot analysis.
Protein extracts were prepared from the homogenized brains of infected animals as described previously (35). The protein content was determined by Bradford analysis (Bio-Rad). Samples were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis on a 10% gel and blotted onto a polyvinylidene difluoride membrane (Millipore). BDV N was detected as described previously (35). To demonstrate correct loading of the gel, the blot was stained with a mouse monoclonal antibody against β-tubulin (Sigma-Aldrich) and developed with a peroxidase-coupled secondary antibody (Jackson ImmunoResearch).
Northern blot analysis.
Vero cells were infected with BDV at a dose of 0.25 FFU per cell for two hours at 37°C. The cells were washed with 1 ml of phosphate-buffered saline, and fresh medium was added. At the various time points, total RNA was extracted from the cultures and 10-μg samples were loaded per lane. Viral RNA was detected by using a radiolabeled probe corresponding to nucleotides 976 to 1749 of the BDV antigenome.
In vitro cytotoxicity assay.
The cytolytic activities of splenocytes were determined by standard 51chromium release assay, with slight modifications as described previously (39), using L929 (H-2k) cells as target cells pulsed with 10−6 M of TELEISSI, mutant peptide TQLEISSI, TILEISSI, TKLEISSI, or TNLEISSI, or the irrelevant H2-Kk-binding peptide FEANGNLI derived from the hemagglutinin protein of influenza virus A/PR/8/34. Peptides TILEISSI, TNLEISSI, TKLEISSI, and TQLEISSI (purity, >70%) were purchased from Genaxxon Bioscience GmbH (Biberach, Germany). Peptide TELEISSI (purity, >65%) was purchased from Neosystem (Strasbourg, France).
Generation of short-term CD8 T-cell cultures.
Splenic lymphocytes from immunized mice (responder cells) were obtained by gently pressing the organ through a metal grid (60 mesh; Sigma). Responder splenocytes were seeded in Iscove's modified Dulbecco's medium (IMDM; GIBCO-BRL) supplemented with 10% fetal calf serum, penicillin-streptomycin, and 1 mM β-mercaptoethanol (complete IMDM) into 24-well plates at 3 × 106 cells/well and mixed with 3 × 105 naive splenocytes pulsed with 10−6 M TELEISSI peptide (stimulator cells). After 5 days in culture, 25 units of recombinant murine interleukin-2 (IL-2) (Peprotech, London, England) was added per ml of medium. Two days later, all cells were harvested, pooled, and seeded again at 3 × 106 responders/well mixed with 3 × 105 TELEISSI-pulsed stimulator cells. The cells were then incubated with one-third conditioned medium from the first week of culture and two-thirds fresh complete IMDM medium. The cultures were again supplemented with 25 U/ml of IL-2, incubated for another 7 days, and analyzed by flow cytometry using TELEISSI/H2-Kk tetramer and anti-CD8α antibody. TELEISSI/H2-Kk tetrameric complexes labeled with phycoerythrin were kindly provided by the NIAID tetramer facility (Bethesda, MD). Tetramers (5 μg/ml for 105 to 106 lymphocytes in a volume of 50 μl) were used together with allophycocyanin-conjugated anti-CD8α antibodies (1 μg/ml, clone 53-6.7; BD PharMingen). Incubation was for 30 min at room temperature. The analysis of stained cells was performed on a FACSort flow cytometer (BD). Only cultures containing at least 50% TELEISSI-specific CD8 T cells were used for the adoptive-transfer experiments.
Adoptive transfer.
Short-term cultures containing at least 50% TELEISSI-specific CD8 T cells were washed, pelleted, resuspended in serum-free IMDM, and filtered through a plastic mesh with a 100-μm pore size. Filtered cells were counted, pelleted, and resuspended in serum-free IMDM at the desired concentration. For intracerebral transfer, a maximal volume of 20 μl was injected into the left brain hemisphere of anesthetized adult mice by using a Hamilton syringe.
Symptoms of neurological disease and scoring of brain mononuclear cell infiltration.
Mild symptoms included a low degree of ataxia and increased anxiety. Intermediate symptoms were clear ataxia, torticollis, unphysiological and uncontrolled movements of extremities when the animal was lifted by the tail, and rough fur or hunched posture. Strong symptoms were pronounced weight loss, severe ataxia, inward folding of hind limbs when the animal was lifted by the tail, torticollis, paraparesis, apathy, and a moribund state. Brain mononuclear cell infiltration was scored in a range from 0 to 3: 0, no infiltrates; 1, up to two perivascular infiltrates per brain section, with one or two layers of cells affected and some mononuclear cells in meninges; 2, three to five perivascular infiltrates per brain section, with multilayer appearance, spread into parenchyma, and intermediate meningitis; 3, six or more perivascular infiltrates per brain section, with multiple layers of cells affected, strong infiltration of parenchyma at multiple sites, and strong meningitis.
Histology and immunohistochemical analysis.
Brain sectioning and immunohistochemistry were done as described previously (7). The viral load in the CNS was assessed by immunohistological staining of 5-μm paraffin-embedded brain sections with monoclonal antibody Bo18 (9) directed against the viral nucleoprotein. Immunostained sections were counterstained with Mayer's hematoxylin.
RESULTS
Recombinant BDV lacking the major CD8 T-cell epitope of H-2k mice.
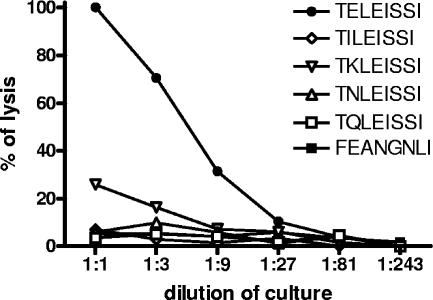
TELEISSI-specific CD8 T cells and L929 cells loaded with various synthetic peptides were used to identify minimal sequence alterations in the nucleoprotein N of BDV that destroy the major T-cell epitope TELEISSI of H-2k mice (39). In a 51chromium release assay, the T cells efficiently lysed L929 cells loaded with peptide TELEISSI (Fig. 1). Of the mutant peptides tested, TILEISSI, TNLEISSI, and TQLEISSI failed to sensitize target cells over background levels for CD8 T-cell-mediated lysis, whereas peptide TKLEISSI retained some residual activity (Fig. 1). These results suggested that BDV mutants in which glutamic acid 130 of the N protein is replaced by isoleucine, asparagine, or glutamine might escape detection by antiviral T cells.
FIG. 1.
TELEISSI mutants escape recognition by CD8 T cells. Short-term cultures of TELEISSI-specific CD8 T cells were used in a standard 51chromium release assay with L929 target cells loaded with 10−6 M of the mutant peptides TQLEISSI, TNLEISSI, TILEISSI, and TKLEISSI. L929 cells pulsed with TELEISSI served as positive control, while cells loaded with the irrelevant H2-Kk-binding influenza virus A/PR/8/34 hemagglutinin-derived peptide FEANGNLI were used as negative control.
Mouse-adapted BDV strains BDV-LRD and BDV-PKLRD replicate with different efficacies in mouse brains (1). Therefore, the epitope mutation replacing glutamic acid at position 130 (E130) of the N protein with glutamine (Q130) was introduced into full-length cDNAs of BDV-LRD and BDV-PKLRD. Replication-competent viruses with this mutation were successfully generated. Sequencing confirmed that the newly introduced mutation was stable during continued propagation of the viruses in Vero cells. These newly generated epitope mutant viruses were designated BDV-NQLRD and BDV- NQPKLRD, respectively.
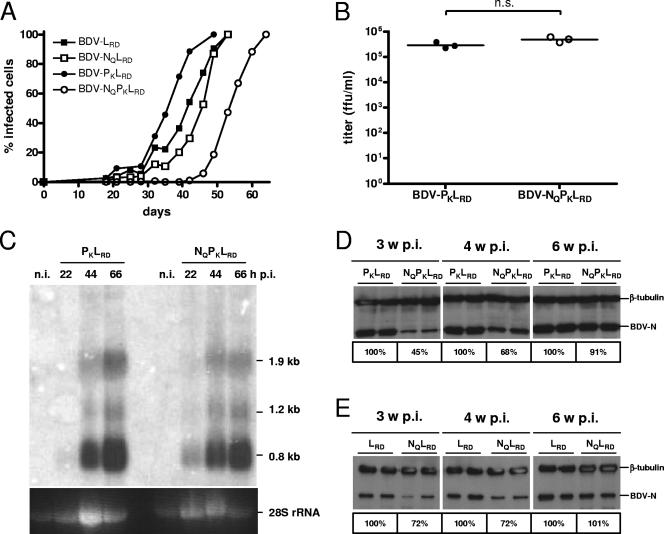
Virus replication analyses were performed in mouse embryo fibroblasts of mice with defective type I interferon receptors (IFNAR10/0). Such cells were previously shown to support the growth of mouse-adapted BDV strains (43). BDV-NQPKLRD and BDV-NQLRD multiplied slightly less well than their respective parental counterparts in this cell culture system (Fig. 2A). To compare the infectivity parameters, virus stocks were produced from persistently infected Vero cells, and the viral titers were determined. The titers of BDV-PKLRD and BDV-NQPKLRD were not significantly different (Fig. 2B). The viral transcripts were analyzed by Northern blotting after acute infection of Vero cells with stocks of BDV-PKLRD or BDV-NQPKLRD. No substantial difference in the kinetics of viral RNA synthesis was noted (Fig. 2C). To analyze virus replication in the mouse CNS in the absence of possible interference through antiviral T cells, we employed MRL β2 m0/0 mice that lack mature CD8 T cells. Newborn animals were infected intracerebrally with 104 FFU of BDV-LRD, BDV-NQLRD, BDV-PKLRD, or BDV-NQPKLRD. Two animals of each group were sacrificed at 3, 4, and 6 weeks postinfection. Protein extracts were prepared from the brains and examined for BDV N by Western blotting. BDV-NQPKLRD (Fig. 2D) and BDV-NQLRD (Fig. 2E) replicated at slightly slower rates than the parental viruses not carrying the Q130 mutation. The attenuated phenotype of the mutant viruses was most readily observed if brain analysis was performed at 3 or 4 weeks postinfection. At 6 weeks postinfection, both the wild-type and mutant viruses had infected most of the susceptible cells of the mouse CNS, and the differences in virus loads as assessed by Western blotting were minimal (Fig. 2D and E). This result was confirmed by staining sections of all brains with a BDV N-specific monoclonal antibody (data not shown).
FIG. 2.
Replication behavior in cell culture and in vivo of BDV carrying mutant epitope TQLEISSI. (A) C57BL/6 IFNAR10/0 mouse embryo fibroblasts were infected (multiplicity of infection, 0.1) with BDV-LRD, BDV-NQLRD, BDV-PKLRD, or BDV-NQPKLRD. Immunofluorescence analyses were performed with aliquots of the various cell cultures twice weekly. The percentage of infected cells was determined by calculating the ratio between BDV N-positive and 4′,6′-diamidino-2-phenylindole-positive cells. (B) Titers of three independent preparations of BDV-PKLRD and BDV-NQPKLRD (each derived from 7 × 107 persistently infected Vero cells) were compared. n.s., difference was statistically not significant. (C) Northern blot analysis of Vero cells infected with BDV-PKLRD or BDV-NQPKLRD for the indicated times. The identities of prominent viral RNAs are indicated. As a loading control, 28S rRNA was visualized by ethidium bromide staining. (D, E) Virus replication in animals was examined by infecting newborn MRL β2 m0/0 mice with 104 FFU of BDV-PKLRD, BDV-NQPKLRD (D), BDV-LRD, or BDV-NQLRD (E). Mice were sacrificed at the indicated times, and brain lysates of two mice per group were analyzed by Western blotting for expression of BDV N. Quantity One software (Bio-Rad) was used for quantification. The amount of BDV N in the CNS of mice infected with wild-type virus was set to 100% for each time point. Staining with a β-tubulin-specific antibody served as loading control. n.i., noninfected; p.i., postinfection; w, weeks.
BDV with E130Q mutation is not recognized by TELEISSI-specific CD8 T cells.
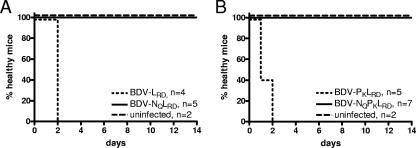
To determine whether BDV-NQPKLRD and BDV-NQLRD might escape detection by adoptively transferred TELEISSI-specific CD8 T cells in the brains of persistently infected B10.BR mice, the animals were given intracerebral injections of 2 × 106 TELEISSI-specific CD8 T cells. All control mice persistently infected with the parental strains BDV-PKLRD and BDV-LRD quickly developed severe neurological symptoms under these conditions and had to be killed within 1 or 2 days post-T-cell transfer (Fig. 3A and B). In contrast, mice infected with either BDV-NQPKLRD or BDV-NQLRD stayed healthy over the complete observation period of 14 days, like the noninfected control mice.
FIG. 3.
Mice persistently infected with BDV carrying mutant epitope TQLEISSI remain healthy after intracerebral transfer of TELEISSI-specific CD8 T cells. Amounts of 2 × 106 TELEISSI-specific CD8 T cells were adoptively transferred by intracerebral injection into uninfected control mice or B10.BR mice persistently infected with BDV-LRD, BDV-NQLRD (A), BDV-PKLRD, or BDV-NQPKLRD (B). Uninfected mice served as negative controls. Animals were analyzed for neurological symptoms for at least 14 days.
BDV with E130Q mutation is not recognized by T cells induced upon vaccination against BDV N.
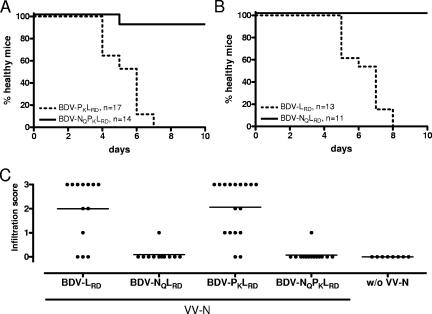
We previously showed that immunopathology resulting in neurological disease can be induced in healthy, persistently infected B10.BR mice by infection with a vaccinia virus vector expressing BDV N (13). Therefore, we designed similar experiments with B10.BR mice persistently infected with the epitope mutant viruses BDV-NQPKLRD and BDV-NQLRD. B10.BR mice persistently infected with the parental viruses BDV-PKLRD and BDV-LRD served as positive controls. Animals infected with BDV for more than 6 weeks, which ensures complete virus infection of the CNS (Fig. 2D and E), were immunized with recombinant vaccinia virus expressing BDV N. As expected, immunization induced neurological disease in all 17 mice infected with BDV-PKLRD and in all 13 animals infected with BDV-LRD (Fig. 4A and B). Symptoms in these animals were nonuniform and ranged from mild and transient to very severe neurological disease. In contrast, only 1 of the 14 animals infected with BDV-NQPKLRD and none of the 11 animals infected with BDV-NQLRD developed neurological symptoms under these experimental conditions (Fig. 4A and B).
FIG. 4.
Mice infected with BDV carrying mutant epitope TQLEISSI remain healthy after immunization with a vaccinia virus vector expressing BDV N. B10.BR mice persistently infected with BDV-PKLRD, BDV-NQPKLRD (A), BDV-LRD, or BDV-NQLRD (B) were challenged intraperitoneally with 2 × 107 PFU of the vaccinia virus vector, and animals were monitored for neurological disease. Mice were sacrificed if moribund or else at day 10 postinfection. (C) To determine the degree of cellular infiltration, hematoxylin and eosin-stained brain sections were scored on an arbitrary scale from 0 to 3 as described in Materials and Methods. A group of BDV-infected mice that was not infected with the vaccinia virus vector (w/o VV-N) served as negative control. Horizontal lines indicate the arithmetic means of scores from each group of animals. Note that disease was relatively mild in some mice, and that most of these animals showed no obvious brain infiltration when sacrificed at the end of the experiment.
In the brains of healthy B10.BR mice persistently infected with mouse-adapted BDV, cellular infiltration is usually undetectable (13). This was also the case in B10.BR animals persistently infected with the recombinant BDVs, provided the animals were not immunized with vaccinia virus expressing BDV N (Fig. 4C). In the brains of most mice infected with BDV-PKLRD or BDV-LRD that developed strong neurological disease after challenge with vaccinia virus, massive mononuclear cell infiltrates were observed (Fig. 4C). Infiltration was particularly prominent in the thalamus and in the hippocampus region, and it correlated well with the intensity of the clinical symptoms (data not shown). Infiltration was minimal or absent in mice infected with the epitope mutants BDV-NQPKLRD or BDV-NQLRD that remained healthy after challenge with the vaccinia virus vector (Fig. 4C).
The spread of BDV with the E130Q mutation remains T-cell restricted in H-2k mice.
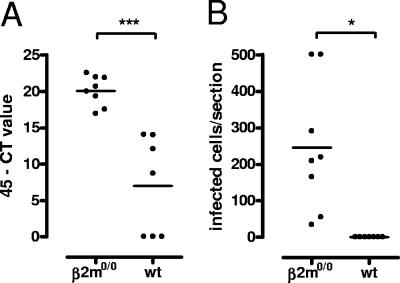
Since the BDV resistance of adult MRL mice is mediated by CD8 T cells (14), we used this experimental setup to evaluate whether BDV can be cleared from the CNS if the TELEISSI epitope is mutated. If BDV-NQPKLRD contained sequences which are recognized by CD8 T cells in adult MRL mice, it should replicate substantially less well in wild-type mice than in β2 m0/0 mice that lack mature CD8 T cells. If, on the other hand, BDV-NQPKLRD escaped control by CD8 T cells, similar viral replication kinetics should be observed in the brains of adult wild-type and β2 m0/0 MRL mice. In the experiment whose results are shown in Fig. 5, groups of wild-type and β2 m0/0 mice were infected with 104 FFU of BDV-NQPKLRD and sacrificed 6 weeks later. One brain hemisphere was then analyzed for viral load by quantitative RT-PCR. BDV-NQPKLRD was abundantly present in all eight β2 m0/0 mice (Fig. 5A). In contrast, it was undetectable in three of seven wild-type mice and present at low levels in the remaining four animals, indicating that the replication and spread of BDV-NQPKLRD were controlled by CD8 T cells. Similar results were obtained when the second brain hemisphere was analyzed for virus-infected cells by immunohistochemistry. When this less-sensitive method was used, all seven brains of wild-type mice appeared to be free of virus, whereas variable numbers of BDV-positive cells were found in all eight brains of β2 m0/0 mice (Fig. 5B). Thus, unidentified CD8 T-cell epitopes, which presumably are derived from BDV proteins other than the nucleoprotein N, seem to compensate for the loss of TELEISSI and are able to mediate virus restriction.
FIG. 5.
BDV carrying mutant epitope TQLEISSI does not escape replication control by antiviral CD8 T cells. Adult (>60 days old) β2 m0/0 and wild-type (wt) MRL mice were infected with 104 FFU of BDV-NQPKLRD. The animals were sacrificed when severe disease occurred or else on day 90 postinfection. Brains were examined for viral load by quantitative RT-PCR (A) or immunohistochemistry (B). Horizontal lines indicate the arithmetic means of the results for each group of animals. Stars indicate statistically significant (*, P < 0.05) or highly statistically significant (***, P < 0.0001) differences in viral load between groups of mice. The value of the threshold cycle (CT) at which a statistically significant increase of the fluorescence signal is first detected was subtracted from 45 (the total number of cycles used).
BDV with E130Q mutation retains ability to induce immunopathology in MRL mice infected as newborns, although with delayed kinetics.
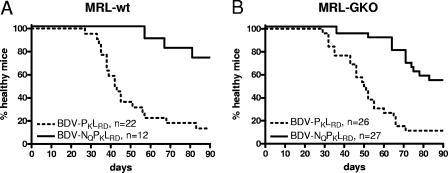
Since the TQLEISSI mutant virus remained restricted by CD8 T cells of MRL mice, it was of interest to determine whether the T-cell response against the minor epitopes might result in neurological disease. Nineteen of the 22 wild-type MRL mice infected as newborns with BDV-PKLRD developed neurological disease during the observation period of 90 days, with the first animals becoming ill at day 27 (Fig. 6A). Only 3 of the 12 animals infected with the mutant BDV-NQPKLRD showed neurological disease at 90 days postinfection (Fig. 6A). In addition, disease induction was significantly delayed in animals infected with the mutant virus as newborns (P = 0.0002; log rank test).
FIG. 6.
BDV carrying mutant epitope TQLEISSI retains ability to induce immunopathology. Newborn wild-type (wt) MRL (A) or MRL-GKO (B) mice were infected with 104 FFU of either BDV-PKLRD or BDV-NQPKLRD and observed for 90 days. The health status of the animals was recorded daily.
Since gamma interferon-deficient MRL mice (MRL-GKO) restrict BDV growth less strongly than their wild-type counterparts (14), we sought to determine whether MRL-GKO mice might more readily reveal the disease potential of viruses carrying the mutant epitope. Twenty-three of the 26 MRL-GKO mice infected with BDV-PKLRD developed neurological disease by day 90 postinfection, with the first mouse becoming ill on day 29 (Fig. 6B). Of the 27 MRL-GKO mice infected with BDV-NQPKLRD, 12 developed neurological disease by day 90 postinfection (Fig. 6B). As in wild-type MRL mice, BDV-NQPKLRD induced disease with significantly slower kinetics than the parental BDV-PKLRD did (P = 0.0002; log rank test). After the termination of the experiment at day 90, the brains of the remaining healthy animals were analyzed for BDV antigen by immunostaining. Large numbers of infected cells were present in most parts of the brains of all animals, irrespective of whether wild-type or mutant virus had been used for infection (data not shown). To rule out the possibility that the late disease onset in mice infected with epitope mutant virus was due to the appearance of virus variants in which the TELEISSI epitope was reintroduced by spontaneous mutation, reverse-transcribed viral RNA from the brains of three diseased wild-type and three MRL-GKO mice was sequenced. This analysis revealed no evidence for mutations in the epitope sequence of the viral N gene (data not shown), excluding a trivial explanation. Thus, our results indicated that BDV with the E130Q mutation retained the ability to elicit antiviral CD8 T-cell responses which can result in neurological disease.
DISCUSSION
Infected H-2k mice mount a highly focused CD8 T-cell response against a single epitope in the N protein of BDV (39). In the present study, we generated recombinant BDV variants lacking the immunodominant CD8 T-cell epitope TELEISSI of H-2k mice. When designing mutations in the TELEISSI epitope, we focused on amino acid E130 for three reasons. First, this amino acid in BDV N occupies an anchor position in TELEISSI and is thus expected to affect peptide binding to major histocompatibility complex class I very strongly (39). Second, other amino acids of the TELEISSI motif are probably performing vital virus functions, as they are part of a motif that facilitates the nuclear export of BDV N (18). Third, TQLEISSI on suitable target cells was not recognized by TELEISSI-specific CD8 T cells.
Our study showed that adoptive transfer of TELEISSI-specific CD8 T cells into B10.BR mice persistently infected with a mutant virus featuring TQLEISSI in place of TELEISSI did not induce neurological disease. In contrast, the transfer of such cells into B10.BR mice infected with the wild-type BDV induced disease very quickly and efficiently. When CD8 T cells were induced by immunization with a poxvirus vector expressing BDV N, no disease was induced in B10.BR mice infected with the E130Q mutant virus. Since such immunization induced disease in mice infected with wild-type BDV, we concluded that BDV N does not induce clonal expansion of H-2k-restricted CD8 T cells directed against minor epitopes that are able to induce disease. Nevertheless, the E130Q mutant virus was recognized and restricted by the immune system if used to infect adult naïve MRL mice, supporting the view that minor T-cell epitopes of BDV, which are presumably derived from viral proteins other than the N protein, gain importance after the major epitope in N is destroyed by mutation. The BDV phosphoprotein P represents a candidate CD8 T-cell target protein, since we previously observed P-specific lytic activity of brain-derived mononuclear cell preparations derived from diseased mice (13). The mapping of the minor epitopes will be a highly demanding task, as brains from mice showing disease after infection with the epitope mutant virus represent the only source of suitable antiviral T cells for such studies. We showed here that the frequency of disease induced by the mutant virus is low and the time between infection and disease is highly variable (Fig. 6).
Interestingly, in addition to CD8 T-cell-mediated virus replication control, T-cell-dependent immunopathology was also observed in the absence of the TELEISSI epitope. Since we excluded the trivial explanation that the mutant virus is able to revert to the wild type under our experimental conditions, our data show that the immune response directed against the minor CD8 T-cell epitopes of BDV is remarkably strong. We considered the possibility that the R66K mutation in the P protein that was introduced to enhance the virulence of BDV for mice (1) might have created a new T-cell epitope. However, epitope prediction programs failed to yield evidence in favor of this possibility (unpublished observations). The observed delay of disease onset in BDV-NQPKLRD-infected newborn MRL mice compared to the time of onset in BDV-PKLRD-infected mice is most probably a direct consequence of a more limited expansion of antiviral CD8 T cells directed against the minor epitopes. However, we cannot rule out the alternative possibility that the slightly slower growth of the mutant virus also contributed to the reduced pathogenicity. It is conceivable that slower virus replication per se altered the dynamics of the antiviral T-cell response, which eventually resulted in reduced immunopathology. Altered viral replication kinetics can also shift the immunodominance patterns of the antiviral cytotoxic T-cell response, as shown in the LCMV infection model (34). It remains unclear why BDV-NQPKLRD replicated slightly less well than BDV-PKLRD. The E130Q mutation does not destroy any known motifs through which the N protein of BDV can interact with the P protein or other interaction partners of viral or cellular origin.
The major conclusions from our work with BDV are in good agreement with the findings of other researchers who studied different viruses. A mutant LCMV lacking both immunodominant CD8 T-cell epitopes of BALB/c mice was eliminated with reduced kinetics from infected animals. A subdominant CD8 T-cell epitope which was identified could not fully compensate for the loss of the major epitope (47). The replication of LCMV with a mutation in one of the major H-2b-restricted CD8 T-cell epitopes induced a CD8 T-cell response against other viral epitopes strong enough to eventually eliminate the mutant virus. However, unlike the case with BDV, mutant LCMV lacking two major CD8 T-cell epitopes no longer induced immunopathology (21). In the case of herpes simplex virus 1, a quick and efficient compensation for the loss of an immunodominant major histocompatibility complex class I-restricted determinant was described (45). A mutant influenza A virus with alterations in the H2-Db anchor residues of its two major epitopes induced higher morbidity in C57BL/6 mice than wild-type virus, and the mutant virus was cleared with reduced kinetics (46).
It seems common that epitope escape viruses exhibit reduced fitness. Most SIV and human immunodeficiency virus epitope mutants that were analyzed showed reduced replication speed, reduced expression of the gag gene, or destabilization of the viral core, indicating that fitness costs limit escape from CD8 T cells (29). In Theiler's virus, epitope-destroying mutations altered the receptor-binding properties of VP2 so that the mutant virus no longer infected critical cell types in vivo (23). Collectively, these studies show that minor epitopes, which usually do not have a great potential to induce specific CD8 T cells, can gain relevance if the major epitope is destroyed, and that viral escape from cytotoxic T-lymphocyte responses is often accompanied by substantial fitness costs. In the case of BDV carrying the E130Q mutation, fitness was impaired only slightly but the control of these mutant viruses by antiviral T cells remained surprisingly good in naïve mice.
Acknowledgments
We thank Rosita Frank for excellent technical assistance, Josef Schneider and Thomas Schenk for supplying the quantitative RT-PCR protocol, the NIAID Tetramer Facility (Atlanta, GA), and the NIH AIDS Research and Reference Reagent Program for producing H2-Kk-TELEISSI tetramer.
This work was supported by the Deutsche Forschungsgemeinschaft (SFB 620).
Footnotes
Published ahead of print on 8 August 2007.
REFERENCES
- 1.Ackermann, A., P. Staeheli, and U. Schneider. 2007. Adaptation of Borna disease virus to new host species attributed to altered regulation of viral polymerase activity. J. Virol. 81:7933-7940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bilzer, T., O. Planz, W. I. Lipkin, and L. Stitz. 1995. Presence of CD4+ and CD8+ T cells and expression of MHC class I and MHC class II antigen in horses with Borna disease virus-induced encephalitis. Brain Pathol. 5:223-230. [DOI] [PubMed] [Google Scholar]
- 3.Briese, T., J. C. De la Torre, A. Lewis, H. Ludwig, and W. I. Lipkin. 1992. Borna disease virus, a negative-strand RNA virus, transcribes in the nucleus of infected cells. Proc. Natl. Acad. Sci. USA 89:11486-11489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.De la Torre, J. C. 1994. Molecular biology of Borna disease virus: prototype of a new group of animal viruses. J. Virol. 68:7669-7675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Engelhardt, K. R., K. Richter, K. Baur, P. Staeheli, and J. Hausmann. 2005. The functional avidity of virus-specific CD8+ T cells is down-modulated in Borna disease virus-induced immunopathology of the central nervous system. Eur. J. Immunol. 35:487-497. [DOI] [PubMed] [Google Scholar]
- 6.Evans, D. T., D. H. O'Connor, P. Jing, J. L. Dzuris, J. Sidney, J. da Silva, T. M. Allen, H. Horton, J. E. Venham, R. A. Rudersdorf, T. Vogel, C. D. Pauza, R. E. Bontrop, R. DeMars, A. Sette, A. L. Hughes, and D. I. Watkins. 1999. Virus-specific cytotoxic T-lymphocyte responses select for amino-acid variation in simian immunodeficiency virus Env and Nef. Nat. Med. 5:1270-1276. [DOI] [PubMed] [Google Scholar]
- 7.Fassnacht, U., A. Ackermann, P. Staeheli, and J. Hausmann. 2004. Immunization with dendritic cells can break immunological ignorance toward a persisting virus in the central nervous system and induce partial protection against intracerebral viral challenge. J. Gen. Virol. 85:2379-2387. [DOI] [PubMed] [Google Scholar]
- 8.Goulder, P. J., C. Pasquier, E. C. Holmes, B. Liang, Y. Tang, J. Izopet, K. Saune, E. S. Rosenberg, S. K. Burchett, K. McIntosh, M. Barnardo, M. Bunce, B. D. Walker, C. Brander, and R. E. Phillips. 2001. Mother-to- child transmission of HIV infection and CTL escape through HLA-A2- SLYNTVATL epitope sequence variation. Immunol. Lett. 79:109-116. [DOI] [PubMed] [Google Scholar]
- 9.Haas, B., H. Becht, and R. Rott. 1986. Purification and properties of an intranuclear virus-specific antigen from tissue infected with Borna disease virus. J. Gen. Virol. 67:235-241. [DOI] [PubMed] [Google Scholar]
- 10.Hahn, Y. S. 2003. Subversion of immune responses by hepatitis C virus: immunomodulatory strategies beyond evasion? Curr. Opin. Immunol. 15:443-449. [DOI] [PubMed] [Google Scholar]
- 11.Hallensleben, W., M. Schwemmle, J. Hausmann, L. Stitz, B. Volk, A. Pagenstecher, and P. Staeheli. 1998. Borna disease virus-induced neurological disorder in mice: infection of neonates results in immunopathology. J. Virol. 72:4379-4386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hausmann, J., K. Baur, K. R. Engelhardt, T. Fischer, H. J. Rziha, and P. Staeheli. 2005. Vaccine-induced protection against Borna disease in wild-type and perforin-deficient mice. J. Gen. Virol. 86:399-403. [DOI] [PubMed] [Google Scholar]
- 13.Hausmann, J., W. Hallensleben, J. C. De la Torre, A. Pagenstecher, C. Zimmermann, H. Pircher, and P. Staeheli. 1999. T cell ignorance in mice to Borna disease virus can be overcome by peripheral expression of the viral nucleoprotein. Proc. Natl. Acad. Sci. USA 96:9769-9774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hausmann, J., A. Pagenstecher, K. Baur, K. Richter, H. J. Rziha, and P. Staeheli. 2005. CD8 T cells require gamma interferon to clear Borna disease virus from the brain and prevent immune system-mediated neuronal damage. J. Virol. 79:13509-13518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Henkel, M., O. Planz, T. Fischer, L. Stitz, and H. J. Rziha. 2005. Prevention of virus persistence and protection against immunopathology after Borna disease virus infection of the brain by a novel Orf virus recombinant. J. Virol. 79:314-325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kao, M., H. Ludwig, and G. Gosztonyi. 1984. Adaptation of Borna disease virus to the mouse. J. Gen. Virol. 65:1845-1849. [DOI] [PubMed] [Google Scholar]
- 17.Kim, T. S., and S. Perlman. 2003. Protection against CTL escape and clinical disease in a murine model of virus persistence. J. Immunol. 171:2006-2013. [DOI] [PubMed] [Google Scholar]
- 18.Kobayashi, T., W. Kamitani, G. Zhang, M. Watanabe, K. Tomonaga, and K. Ikuta. 2001. Borna disease virus nucleoprotein requires both nuclear localization and export activities for viral nucleocytoplasmic shuttling. J. Virol. 75:3404-3412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ludwig, H., L. Bode, and G. Gosztonyi. 1988. Borna disease: a persistent virus infection of the central nervous system. Prog. Med. Virol. 35:107-151. [PubMed] [Google Scholar]
- 20.Martin, A., P. Staeheli, and U. Schneider. 2006. RNA polymerase II-controlled expression of antigenomic RNA enhances the rescue efficacies of two different members of the Mononegavirales independently of the site of viral genome replication. J. Virol. 80:5708-5715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moskophidis, D., and R. M. Zinkernagel. 1995. Immunobiology of cytotoxic T-cell escape mutants of lymphocytic choriomeningitis virus. J. Virol. 69:2187-2193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Muller, U., U. Steinhoff, L. F. Reis, S. Hemmi, J. Pavlovic, R. M. Zinkernagel, and M. Aguet. 1994. Functional role of type I and type II interferons in antiviral defense. Science 264:1918-1921. [DOI] [PubMed] [Google Scholar]
- 23.Myoung, J., W. Hou, B. Kang, M. A. Lyman, J. A. Kang, and B. S. Kim. 2007. The immunodominant CD8(+) T cell epitope region of Theiler's virus in resistant C57BL/6 mice is critical for anti-viral immune responses, viral persistence, and binding to the host cells. Virology 360:159-171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nishino, Y., D. Kobasa, S. A. Rubin, M. V. Pletnikov, and K. M. Carbone. 2002. Enhanced neurovirulence of Borna disease virus variants associated with nucleotide changes in the glycoprotein and L polymerase genes. J. Virol. 76:8650-8658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nöske, K., T. Bilzer, O. Planz, and L. Stitz. 1998. Virus-specific CD4+ T cells eliminate Borna disease virus from the brain via induction of cytotoxic CD8+ T cells. J. Virol. 72:4387-4395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Perlman, S., and L. Pewe. 1998. Role of CTL mutants in demyelination induced by mouse hepatitis virus, strain JHM. Adv. Exp. Med. Biol. 440:515-519. [DOI] [PubMed] [Google Scholar]
- 27.Pewe, L., S. Xue, and S. Perlman. 1998. Infection with cytotoxic T-lymphocyte escape mutants results in increased mortality and growth retardation in mice infected with a neurotropic coronavirus. J. Virol. 72:5912-5918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peyerl, F. W., D. H. Barouch, and N. L. Letvin. 2004. Structural constraints on viral escape from HIV- and SIV-specific cytotoxic T-lymphocytes. Viral Immunol. 17:144-151. [DOI] [PubMed] [Google Scholar]
- 29.Peyerl, F. W., H. S. Bazick, M. H. Newberg, D. H. Barouch, J. Sodroski, and N. L. Letvin. 2004. Fitness costs limit viral escape from cytotoxic T lymphocytes at a structurally constrained epitope. J. Virol. 78:13901-13910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pircher, H., D. Moskophidis, U. Rohrer, K. Burki, H. Hengartner, and R. M. Zinkernagel. 1990. Viral escape by selection of cytotoxic T cell-resistant virus variants in vivo. Nature 346:629-633. [DOI] [PubMed] [Google Scholar]
- 31.Planz, O., T. Bilzer, and L. Stitz. 1995. Immunopathogenic role of T-cell subsets in Borna disease virus-induced progressive encephalitis. J. Virol. 69:896-903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Planz, O., and L. Stitz. 1999. Borna disease virus nucleoprotein (p40) is a major target for CD8+-T-cell-mediated immune response. J. Virol. 73:1715-1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Price, G. E., R. Ou, H. Jiang, L. Huang, and D. Moskophidis. 2000. Viral escape by selection of cytotoxic T cell-resistant variants in influenza A virus pneumonia. J. Exp. Med. 191:1853-1867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Probst, H. C., K. Tschannen, A. Gallimore, M. Martinic, M. Basler, T. Dumrese, E. Jones, and M. F. van den Broek. 2003. Immunodominance of an antiviral cytotoxic T cell response is shaped by the kinetics of viral protein expression. J. Immunol. 171:5415-5422. [DOI] [PubMed] [Google Scholar]
- 35.Rauer, M., J. Gotz, D. Schuppli, P. Staeheli, and J. Hausmann. 2004. Transgenic mice expressing the nucleoprotein of Borna disease virus in either neurons or astrocytes: decreased susceptibility to homotypic infection and disease. J. Virol. 78:3621-3632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Richt, J. A., L. Stitz, U. Deschl, K. Frese, and R. Rott. 1990. Borna disease virus-induced meningoencephalomyelitis caused by a virus-specific CD4+ T cell-mediated immune reaction. J. Gen. Virol. 71:2565-2573. [DOI] [PubMed] [Google Scholar]
- 37.Richt, J. A., L. Stitz, H. Wekerle, and R. Rott. 1989. Borna disease, a progressive meningoencephalomyelitis as a model for CD4+ T cell-mediated immunopathology in the brain. J. Exp. Med. 170:1045-1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rott, R., and H. Becht. 1995. Natural and experimental Borna disease in animals. Curr. Top. Microbiol. Immunol. 190:17-30. [DOI] [PubMed] [Google Scholar]
- 39.Schamel, K., P. Staeheli, and J. Hausmann. 2001. Identification of the immunodominant H-2K(k)-restricted cytotoxic T-cell epitope in the Borna disease virus nucleoprotein. J. Virol. 75:8579-8588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Schneemann, A., P. A. Schneider, R. A. Lamb, and W. I. Lipkin. 1995. The remarkable coding strategy of Borna disease virus: a new member of the nonsegmented negative strand RNA viruses. Virology 210:1-8. [DOI] [PubMed] [Google Scholar]
- 41.Schneider, U., M. Schwemmle, and P. Staeheli. 2005. Genome trimming: a unique strategy for replication control employed by Borna disease virus. Proc. Natl. Acad. Sci. USA 102:3441-3446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sobbe, M., T. Bilzer, S. Gommel, K. Nöske, O. Planz, and L. Stitz. 1997. Induction of degenerative brain lesions after adoptive transfer of brain lymphocytes from Borna disease virus-infected rats: presence of CD8+ T cells and perforin mRNA. J. Virol. 71:2400-2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Staeheli, P., M. Sentandreu, A. Pagenstecher, and J. Hausmann. 2001. Alpha/beta interferon promotes transcription and inhibits replication of Borna disease virus in persistently infected cells. J. Virol. 75:8216-8223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Stitz, L., M. Sobbe, and T. Bilzer. 1992. Preventive effects of early anti-CD4 or anti-CD8 treatment on Borna disease in rats. J. Virol. 66:3316-3323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Stock, A. T., C. M. Jones, W. R. Heath, and F. R. Carbone. 2006. CTL response compensation for the loss of an immunodominant class I-restricted HSV-1 determinant. Immunol. Cell Biol. 84:543-550. [DOI] [PubMed] [Google Scholar]
- 46.Webby, R. J., S. Andreansky, J. Stambas, J. E. Rehg, R. G. Webster, P. C. Doherty, and S. J. Turner. 2003. Protection and compensation in the influenza virus-specific CD8+ T cell response. Proc. Natl. Acad. Sci. USA 100:7235-7240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Weidt, G., O. Utermohlen, J. Heukeshoven, F. Lehmann-Grube, and W. Deppert. 1998. Relationship among immunodominance of single CD8+ T cell epitopes, virus load, and kinetics of primary antiviral CTL response. J. Immunol. 160:2923-2931. [PubMed] [Google Scholar]