Abstract
Secretory phospholipase A2 (sPLA2) is the major effector involved in arachidonic acid (AA) mobilization and prostaglandin E2 (PGE2) production during stimulation of P388D1 macrophages with the inflammatory stimuli bacterial lipopolysaccharide and platelet-activating factor. We herein demonstrate that PGE2 in stimulated P388D1 cells is accounted for by the inducible cyclooxygenase (COX)-2. COX-1, though present, appears not to participate significantly in stimulus-induced PGE2 production in P388D1 macrophages. Reconstitution experiments utilizing exogenous recombinant sPLA2 demonstrate that activation of the sPLA2 at the plasma membrane is highly dependent on previous activation of the cytosolic phospholipase A2 (cPLA2). Collectively these results demonstrate (i) that functional coupling exists between sPLA2 and COX-2 in activated cells, (ii) the critical role that cPLA2 plays in lipid mediator production, and (iii) that there is crosstalk between cPLA2 and sPLA2 in the cell.
The phospholipase A2 (PLA2) superfamily is composed of a number of lipolytic enzymes whose common feature is to hydrolyze the fatty acid present in the sn-2 position of glycerophospholipids (1). At least three different PLA2s exist in mammalian cells, namely a secretory PLA2 (sPLA2), the 85-kDa cytosolic group IV PLA2 (cPLA2), and a Ca2+-independent group VI PLA2 (iPLA2) (1, 2). Increasing evidence suggests that all three PLA2 forms may participate in some manner in arachidonic acid (AA) turnover and mobilization with their relative contribution being dependent on the cell type and agonist used.
cPLA2 has been shown to act on intracellular membranes—i.e., those of the perinuclear envelope and endoplasmic reticulum (3, 4). The plasma membrane of the cells appears to be the major site of action of the sPLA2, which is consistent with the fact that sPLA2 requires millimolar Ca2+ for activity (5–11). sPLA2 appears to be responsible for the majority of free AA produced by stimulated P388D1 cells (7, 12–14).
Once liberated from phospholipids, the AA is converted to prostaglandins by the cyclooxygenases (COXes). Two different COX enzymes have been identified in cells (15). The first one, COX-1, is constitutively expressed by most cell types, whereas the other one, COX-2, is generally induced after cell stimulation (15). As is the case for the PLA2s, the relative contribution of each of these COX isoenzymes to overall prostaglandin synthesis appears to be strikingly dependent on cell type and stimulus used (16). However the question remains as to whether a specific coupling of each COX isoenzyme to a particular PLA2 exists. Although supportive evidence for that view is emerging (15, 16), identification of the particular COX and PLA2 isoenzymes involved has proven to be difficult and often contradictory. For example, Herschman and colleagues (11, 17–19) have suggested a coupling between sPLA2 and COX-1 for the immediate response of mast cells; however, Arm and colleagues (20, 21) have suggested that the sPLA2 is coupled to COX-2 in the same cells. In a recent report, Murakami et al. (22) have shown that the cPLA2 couples to both COX-1 and COX-2 for the two phases of prostaglandin production in mouse osteoblasts.
There is a second important unanswered question regarding the cellular biochemistry of sPLA2. This enzyme appears to act poorly against intact cellular membranes. Thus, some sort of physical perturbation or “membrane rearrangement” is required for sPLA2 to act on a cellular membrane (5, 6). However, the biochemical signals that cause such a perturbation are largely unknown. Fourcade et al. (23) have suggested that loss of membrane asymmetry due to phospholipid flip-flop could be one of these signals. We have recently found that accumulation of membrane destabilizers such as diacylglycerol or ceramide may also serve to perturb plasma membrane packing and hence favor sPLA2 action (24). More importantly, we found as well that increasing the intracellular levels of AA by exogenous addition of unlabeled fatty acid to [3H]AA-labeled cells (which mimics cPLA2 activation) was able to trigger release of [3H]AA by a mechanism dependent on sPLA2. These data suggested that cPLA2 activation may be another key event that leads to perturbation of the membrane, rendering it susceptible to sPLA2 attack (13).
In the current study, we have studied the expression of COX isoforms in P388D1 cells, and we have found that a functional link exists between sPLA2 and COX-2 for eliciting prostaglandin production in activated cells. Furthermore, reconstitution experiments using recombinant sPLA2 further support the notion that crosstalk exists between the cPLA2 and the sPLA2 during stimulation of AA release in P388D1 cells. Thus the cPLA2 plays a dual role in arachidonate signaling as it (i) participates in an intermediate signaling step that is required for sPLA2 activation and (ii) acts as a producer of AA itself.
EXPERIMENTAL PROCEDURES
Materials.
Mouse P388D1 macrophage-like cells were obtained from the American Type Culture Collection. Iscove’s modified Dulbecco’s medium (endotoxin <0.05 ng/ml) was from BioWhittaker. Fetal bovine serum was from HyClone. Nonessential amino acids were from Irvine Scientific. [5,6,8,9,11,12,14,15-3H]AA (specific activity 100 Ci/mmol; 1 Ci = 37 GBq) was from New England Nuclear. Platelet-activating factor (PAF), bacterial lipopolysaccharide (LPS; Re 595 from Salmonella minnesota), actinomycin D, cycloheximide, and AA were from Sigma. Okadaic acid was from Calbiochem or Biomol (Plymouth Meeting, PA). Methyl arachidonyl fluorophosphonate (MAFP), NS-398, indomethacin, and aspirin were from Cayman Chemicals (Ann Arbor, MI). Human recombinant synovial PLA2 and purified IgG from anti-human synovial PLA2 rabbit antiserum (BQY-113A) were generously provided by J. L. Bobbitt and R. M. Kramer (Eli Lilly, Indianapolis, IN). Antibodies against murine COX isoforms were generously provided by W. L. Smith (Department of Biochemistry, Michigan State University, East Lansing, MI).
Cell Culture and Labeling Conditions.
P388D1 cells were maintained at 37°C in a humidified atmosphere at 90% air and 10% CO2 in Iscove’s modified Dulbecco’s medium supplemented with 10% fetal bovine serum, 2 mM glutamine, 100 units/ml penicillin, 100 μg/ml streptomycin, and nonessential amino acids. P388D1 cells were plated at 106 per well, allowed to adhere overnight, and used for experiments the following day. All experiments were conducted in serum-free Iscove’s modified Dulbecco’s medium. When required, radiolabeling of the P388D1 cells with [3H]AA was achieved by including 0.5 μCi/ml [3H]AA during the overnight adherence period (20 h). Labeled AA that had not been incorporated into cellular lipids was removed by washing the cells four times with serum-free medium containing 5 mg/ml albumin.
Stimulation of the Cells.
The standard regimen for activating P388D1 cells with LPS and PAF has been described previously (7, 13, 25). Briefly, P388D1 cells were placed in serum-free medium for 30–60 min before the addition of LPS (200 ng/ml) for 1 h, after which they were challenged with 100 nM PAF for the time indicated.
Western Blot Analyses.
The cells were washed twice with serum-free medium and homogenized by 25 strokes in a Dounce homogenizer in a buffer consisting of 20 mM Tris⋅HCl, 2 mM EDTA, 10 mM EGTA, 1 mM phenylmethylsulfonyl fluoride, 20 μM leupeptin, 20 μM aprotinin, and 0.1% 2-mercaptoethanol, pH 7.5. The homogenates were centrifuged at 500 × g for 5 min at 4°C to separate nuclei. The resulting supernatant was centrifuged at 100,000 × g for 90 min at 4°C to separate cytosolic and membrane fractions. Samples from cell homogenates (50 μg) and their equivalent cytosolic and membrane fractions were separated by SDS/PAGE (10% acrylamide gel) and transferred to Immobilon-P (Millipore). Nonspecific binding was blocked by incubating the membranes with 5% nonfat milk in phosphate-buffered saline for 18 h. Membranes were incubated with anti-COX-1 or anti-COX-2 antiserum and then treated with horseradish peroxidase-conjugated protein A (Amersham). Bands were detected by enhanced chemiluminiscence (ECL; Amersham).
Northern Blot Analyses.
Total RNA was isolated from unstimulated or LPS/PAF-stimulated cells by the Trizol reagent method (Life Technologies), exactly as indicated by the manufacturer. Five micrograms of RNA was electrophoresed in an 1% formaldehyde/agarose gel and transferred to nylon filters (Hybond; Amersham) in 10× SSC buffer (1× SSC = 0.15 M NaCl, 0.015 M sodium citrate, pH 7.0). Hybridizations were performed in QuickHyb solution (Stratagene) by following the manufacturer’s instructions. 32P-labeled probes for COX-1 or COX-2 (Cayman Chemicals) were coincubated with the filters for 1 h at 66°C, followed by three washes with 2× SSC containing 0.1% SDS at room temperature for 30 min. A final wash was carried out at 60°C for 30 min with 1× SSC containing 0.1% SDS. Bands were visualized by autoradiography.
Measurement of Prostaglandin E2 (PGE2) Production and of Extracellular [3H]AA Release.
For PGE2 production, LPS-treated cells were stimulated with 100 nM PAF for 10 min. Afterward, the supernatants were removed and cleared of detached cells by centrifugation, and PGE2 was quantitated by using a specific radioimmunoassay (PerSeptive Biosystems, Framingham, MA). For [3H]AA release experiments, the cells, labeled with [3H]AA as described above, were stimulated with 100 nM PAF for 10 min in the presence of 0.1 mg/ml BSA. The supernatants were removed, cleared of detached cells by centrifugation, and assayed for radioactivity by liquid scintillation counting.
Data Presentation.
Assays were carried out in duplicate or triplicate. Each set of experiments was repeated at least three times with similar results. Unless otherwise indicated, the data presented are from representative experiments.
RESULTS AND DISCUSSION
Expression of COX Isoforms.
When P388D1 macrophages are treated with 200 ng/ml LPS for 1 h and then stimulated with 100 nM PAF, a rapid burst of PGE2 is generated, reaching a peak 3–5 min after PAF addition (12). Immediate PGE2 production occurs concomitantly with activation of both cPLA2 and sPLA2, and no further PGE2 is produced in a delayed phase, even after several hours of incubation with LPS/PAF (12, 25). Immunoblot analysis of the COX isoforms expressed by resting P388D1 cells revealed that COX-2 protein was increased by LPS treatment of the cells (Fig. 1A). COX-1, on the contrary, did not appear to change (Fig. 1A). LPS-induced expression of COX-2 was blocked by both actinomycin D and cycloheximide, inhibitors of RNA transcription and protein synthesis, respectively (Fig. 1A). COX-1 expression was not affected by either actinomycin D or cycloheximide (Fig. 1A).
Figure 1.
(A) Expression of COX isoforms in P388D1 cells. The cells were incubated with 5 μM actinomycin D (A) or 10 μM cycloheximide (C) for 30 min before the LPS/PAF treatment (1 h with LPS plus 10 min with PAF). Cells were then lysed as described in the text. Protein (100 μg) was separated by SDS/PAGE and analyzed by immunoblotting using specific antibodies against COX-1 or COX-2. (B) Northern blot of COX-1 and COX-2 from total P388D1 RNA. Total RNA from LPS/PAF-stimulated cells or nonstimulated (−) was isolated and hybridized with probes for COX-1 and COX-2, as indicated. As a control for RNA loading, an “in-gel” RNA picture is shown on the right.
The above results were confirmed by analyzing RNA message levels for both COX-1 and COX-2. When total RNA from resting cells was analyzed by Northern blotting using probes for COX-1, the signal detected was identical to that found when RNA from LPS/PAF-activated cells was used (Fig. 1B). Total RNA from resting cells also gave a positive signal when probes for COX-2 were used, albeit the signal was much weaker than that found for COX-1. A strong signal for COX-2 was detected, however, in RNA samples from LPS/PAF-activated cells (Fig. 1B).
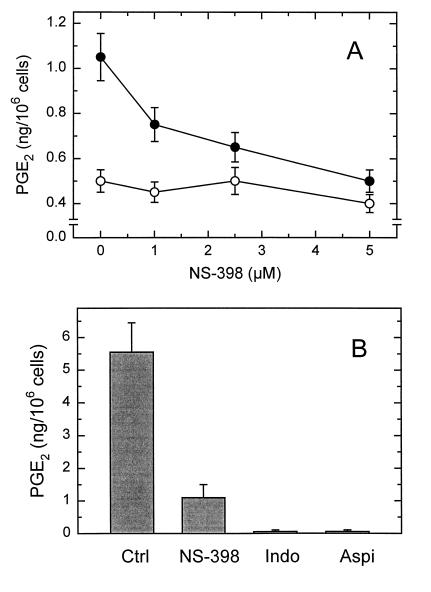
LPS/PAF-induced PGE2 production was completely abolished by NS-398, a specific COX-2 inhibitor (Fig. 2A). NS-398 completely inhibits COX-2 with an IC50 <5 μM, whereas COX-1 remains unaffected at concentrations higher than 100 μM (26). Thus the above data suggest that COX-2 is the only enzyme responsible for stimulus-induced PGE2 in these cells. Our previous results have demonstrated that sPLA2 is the enzyme that provides most of the AA to be used for PGE2 production in activated conditions in P388D1 cells (7, 12, 14). Thus these previous data coupled with the results reported herein formally establish the existence of a link between sPLA2 and COX-2 in activated cells.
Figure 2.
A) Effect of NS-398 on PGE2 production in P388D1 cells. The cells were incubated with the indicated concentrations of NS-398 for 30 min before and during the LPS/PAF treatment. PGE2 in the supernatants was quantitated by using a specific radioimmunoassy. Basal PGE2 production—i.e., that observed in the absence of LPS/PAF at the indicated NS-398 concentrations—is indicated by the open circles. (B) Effect of COX inhibitors on PGE2 production from exogenous AA. The cells were treated with 5 μM NS-398, 25 μM indomethacin (Indo), 25 μM aspirin (Aspi), or neither (Ctrl) for 30 min before and during the 1-h treatment with LPS. Afterward, 1 μM AA was added and the amount of PGE2 produced after 10 min was quantitated by using a specific radioimmunoassay.
From the data shown in Fig. 2A, it is apparent that basal unstimulated PGE2 levels were not affected by NS-398. This finding could suggest that basal PGE2 is produced by COX-1 in the resting cells. However it could also be possible that COX-1 is not functional in P388D1 cells and that the basal PGE2 produced corresponds to the fraction of PGE2 that was produced during preincubation, just before the COX-2 became inactivated by NS-398. To investigate these possibilities, experiments were performed wherein PGE2 production was analyzed in cells exposed to 1 μM exogenous AA (Fig. 2B). As well as being physiologically sound (under normal circumstances, the sPLA2 provides the AA from outside), this approach has the advantage that the total amount of PGE2 produced by the cells can be controlled (by adding more or less exogenous AA). PGE2 production under these conditions was strongly, but not completely, inhibited by NS-398, indicating that the majority of the COX activity to which exogenous AA is accessible arises from COX-2 (≈80%). However, there is also an appreciable contribution by COX-1, as judged by the NS-398-resistant PGE2 production (≈20%) (Fig. 2B). Aspirin and indomethacin, two nonspecific COX inhibitors, abolished PGE2 production (Fig. 2B). Collectively, the results from these experiments suggest that the AA released by the sPLA2 after cellular stimulation is accessible only to COX-2 and not to COX-1, even though the latter is present in active form in the macrophages.
cPLA2 Regulates sPLA2-Dependent AA and PGE2 Production in Activated P388D1 Macrophages.
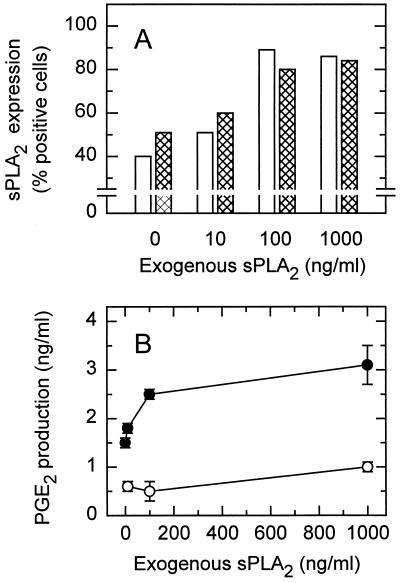
To further assess the coupling of sPLA2 to COX-2 in P388D1 cells, a series of experiments was performed that involved adding exogenous recombinant sPLA2 to the P388D1 cells. The sPLA2 present in P388D1 cells belongs to group V (14). Unfortunately, no purification of group V sPLA2 from either natural or recombinant sources has been reported. Thus for these experiments we used recombinant group IIA sPLA2, which is structurally similar to the group V enzyme (16). Fig. 3A shows that exogenous sPLA2 readily associated in a dose-dependent manner with the membrane of both resting and activated P388D1 cells, as judged by flow cytometry under our previously described conditions (14). However, the ability of exogenous sPLA2 to elicit lipid mediator production was strikingly dependent on the activation state of the cells. Exogenous sPLA2 was almost inactive when added to nonstimulated cells, whereas the enzyme noticeably increased PGE2 production when added to activated cells (Fig. 3B). These data are consistent with work by other laboratories in different cell types (8, 27, 28) and thus give additional support to the idea that, for the sPLA2 to act on cellular membranes, membrane perturbation induced by a costimulator must occur first (5, 6).
Figure 3.
Effect of adding exogenous sPLA2 to P388D1 cells. (A) Either resting (open bars) or LPS/PAF-activated (crosshatched bars) cells were incubated with the indicated concentrations of exogenous sPLA2, and sPLA2 surface expression was determined by flow cytometry. (B) PGE2 production by resting (○) or LPS/PAF-activated (•) P388D1 cells in the presence of the indicated concentrations of exogenous sPLA2. Exogenous sPLA2 was added at the time the cells were exposed to PAF or vehicle, and was present for 10 min.
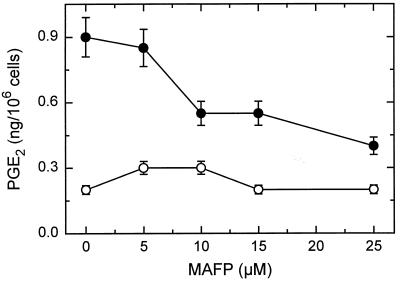
We recently proposed that a transient accumulation of intracellular free AA produced by cPLA2 may constitute another important factor leading to sPLA2 activation in stimulated cells (13). This suggestion was based on the finding that artificially increasing the intracellular free AA levels by exogenous addition of fatty acid enabled phospholipid hydrolysis, apparently mediated by sPLA2 (13). Because transient elevations in the intracellular AA concentration are caused by the cPLA2, these data suggested that crosstalk may exist between the two PLA2s during P388D1 cell activation by LPS/PAF (13). Further evidence for such crosstalk was obtained by experiments determining the effect of MAFP on PGE2 production by LPS/PAF-treated cells. MAFP inhibits cPLA2 but not sPLA2 (13), yet it strongly inhibited PGE2 production (Fig. 4), which is mostly an sPLA2-dependent process (7, 14).
Figure 4.
Effect of MAFP on PGE2 production by P388D1 cells. The cells were incubated with the indicated concentrations of MAFP, which was added 15 min before PAF. PGE2 in the supernatants was quantitated by using a specific radioimmunoassy. Basal PGE2 production—i.e., that observed in the absence of LPS/PAF at the indicated MAFP concentrations—is indicated by ○.
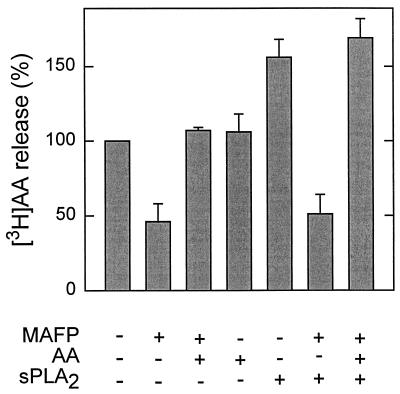
However, validation of the existence of crosstalk between the two PLA2s requires proof that the AA is actually activating the sPLA2 and not inducing phospholipid hydrolysis by some other, unexpected, mechanism. We have further addressed the specificity of AA in activating the sPLA2 by carrying out AA-release reconstitution experiments utilizing exogenous sPLA2. In agreement with our previous data (13), when [3H]AA-prelabeled LPS-treated cells were incubated with PAF in the presence of the cPLA2 inhibitor MAFP (25 μM), [3H]AA release to the extracellular medium was markedly inhibited, but this inhibition was reversed when the cells were exposed to exogenous AA (1 μM) for 1 min before PAF addition (Fig. 5). Consistent with the data shown in Fig. 3B, addition of exogenous sPLA2 (500 ng/ml) increased PAF-stimulated [3H]AA release (Fig. 5). However, exogenous sPLA2 did not have any effect on PAF-stimulated [3H]AA release when MAFP-treated cells were used; in fact, the response still remained inhibited (Fig. 5).
Figure 5.
AA restores the enhancing effect of exogenous sPLA2 on [3H]AA mobilization in activated P388D1 cells. [3H]AA-labeled LPS-treated cells were preincubated with MAFP (25 μM) for 15 min where indicated. Subsequently, 1 μM exogenous unlabeled AA was added 1 min before treatment with PAF (100 nM), as indicated. Where indicated, exogenous sPLA2 (500 ng/ml) was added together with PAF. The data are expressed as a percentage of the response observed in activated cells in the absence of any addition, which was taken as 100%.
The inability of exogenous sPLA2 to enhance [3H]AA release in MAFP-treated cells cannot be explained by lack of membrane perturbation, because a costimulator—i.e., PAF—is also present. Moreover because, as mentioned above, MAFP does not have any inhibitory effect on sPLA2 (13), these results demonstrate that MAFP specifically blocks generation of a signal that is required for the exogenous sPLA2 to attack the membrane. Direct proof that this signal is provided by elevation of the intracellular free AA levels was given by the finding that coincubation with this fatty acid not only reversed the MAFP inhibition but even restored the enhanced [3H]AA release response to PAF plus exogenous sPLA2 (Fig. 5). The enhancing effect of AA appears to be specific, because other fatty acids tested, whether saturated (palmitic acid, stearic acid, arachidic acid) or unsaturated (oleic acid, linoleic acid), failed to restore the [3H]AA release (13).
P388D1 cells manifest an extraordinarily high capacity to incorporate exogenous AA into membrane phospholipids (12, 29, 30). As much as 25% of the fatty acid at 1 μM—the concentration used in the experiment shown in Fig. 5—is incorporated into the phospholipids of 106 cells in 10 min in the absence of albumin (12). This amount gives a rate of incorporation of about 25 pmol of AA per min per 106 cells. However, in the presence of albumin—as employed in the experiment depicted in Fig. 5—the amount of available AA is reduced to one-fourth, as the majority is trapped by the albumin in the incubation medium (J.B. and E.A.D., unpublished data). Thus the rate of incorporation of exogenous unlabeled AA under the conditions of Fig. 5 is about 6 pmol per min per 106 cells. At 1 μM AA, little fatty acid is incorporated into triacylglycerols, which indicates that the steady-state lysophospholipid pool is sufficient to account for this rate of incorporation of free AA even in the absence of albumin (30). Moreover, the specific activity of the reacylating enzymes arachidonoyl-CoA synthetase and lysophospholipid:acyl-CoA acyltransferase in P388D1 cells are 104 and 33 nmol per min per 106 cells (ref. 29; one million P388D1 cells comprises ≈100 μg of protein). Therefore, because of the exceedingly high activity of the reacylating enzymes in P388D1 cells it is highly unlikely that the restoring effect of exogenous unlabeled AA on [3H]AA release shown in Fig. 5 is because of inhibition of [3H]AA reacylation in the cells. Further experimental support for this interpretation is given by the finding that exogenous AA does not affect [3H]AA release in cells not treated with MAFP (Fig. 5). If the enhancing effect of exogenous AA on [3H]AA release in MAFP-treated cells was because of inhibition of reacylation, one would expect an enhanced [3H]AA release in the non-MAFP-treated cells as well, which was clearly not the case (Fig. 5).
AA and PGE2 Release Mechanism in P388D1 Cells.
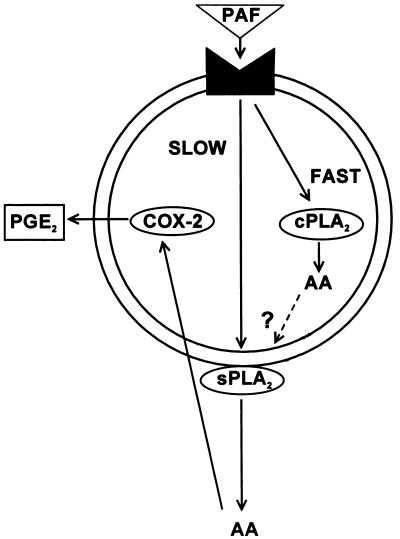
Collectively, the data in this study establish that elevated levels of intracellular AA specifically lead to activation of sPLA2 at the outer leaflet of the plasma membrane. Because elevated intracellular free AA levels are caused solely by cPLA2 activation (13), the current results formally establish that crosstalk exists between cPLA2 and sPLA2 during P388D1 cell activation by LPS/PAF. Therefore, the current data document a dual role for AA during macrophage activation by LPS/PAF. As well as serving itself as a substrate for the synthesis of other lipid mediators, the AA—or a metabolite—serves a signaling role by enabling activation of the sPLA2 and thus allowing for a further amplification of the inflammatory response. These results, along with our previous data (12–14), support a mechanism for AA mobilization in P388D1 cells whereby PAF receptor occupancy immediately leads to cPLA2 activation, which, in turn, induces a transient elevation of intracellular free AA levels (Fig. 6). Elevated levels of free AA during the initial stages of P388D1 cell activation may serve important metabolic and biochemical functions, one of which is to help activate the sPLA2 that has appeared at the plasma membrane. Whether the activating effect of cPLA2-derived AA on the sPLA2 is a direct one or is mediated by accessory system(s) remains to be elucidated.
Figure 6.
Crosstalk between cPLA2 and sPLA2 in eliciting AA mobilization in activated P388D1 macrophages. PAF activation of the LPS-primed macrophages triggers the “fast” activation of the cPLA2 intracellularly, which in turn allows the “slow” action of sPLA2 at the plasma membrane. The AA liberated by the sPLA2 can be taken up and utilized by COX-2 to generate prostaglandins such as PGE2. For further details see text.
Once the sPLA2 is activated at the plasma membrane, it starts to hydrolyze phospholipids and release AA to the extracellular medium. Part of this AA will be recaptured by the cell, and a minor portion of it (see below) will be made accessible to COX-2, the enzyme responsible for producing PGE2 during activation conditions. COX-1, though present and active, is spared from the process. Thus, the sPLA2 specifically feeds COX-2, not COX-1. One possibility for the COX-1 not to participate in PGE2 production in activated cells could be that this enzyme is located farther away from the sPLA2 than is COX-2. Because of the exceedingly high reacylating capacity of the P388D1 cells (29, 30), only less than 5% of the liberated AA is converted into prostaglandins (31). If the sPLA2—and/or the cPLA2—releases AA not in the immediate vicinity of COX-1, the fatty acid might be impeded in reaching the enzyme, as it would be acylated back into phospholipids well before reaching COX-1. According to this scheme, it could be envisioned that the active COX-2 pool is located in close proximity to the intracellular compartment wherein cellular uptake of AA takes place. Further work will be necessary to explore this intriguing possibility.
Acknowledgments
We are most appreciative to Drs. J. L. Bobbitt, R. M. Kramer, and W. L. Smith for providing the antibodies used in these studies. This work was supported by Grants HD 26171 and GM 20501 from the National Institutes of Health.
ABBREVIATIONS
- PLA2
phospholipase A2
- cPLA2
85-kDa group IV cytosolic phospholipase A2
- sPLA2
secretory phospholipase A2
- AA
arachidonic acid
- COX
cyclooxygenase
- PGE2
prostaglandin E2
- LPS
bacterial lipopolysaccharide
- PAF
platelet-activating factor
- MAFP
methyl arachidonyl fluorophosphonate
References
- 1.Dennis E A. J Biol Chem. 1994;269:13057–13060. [PubMed] [Google Scholar]
- 2.Dennis E A. Trends Biochem Sci. 1997;22:1–2. doi: 10.1016/s0968-0004(96)20031-3. [DOI] [PubMed] [Google Scholar]
- 3.Glover S, de Carvalho M S, Bayburt T, Jones M, Chi E, Leslie C C, Gelb M H. J Biol Chem. 1995;270:15359–15367. doi: 10.1074/jbc.270.25.15359. [DOI] [PubMed] [Google Scholar]
- 4.Schievella A R, Regier M K, Smith W L, Lin L L. J Biol Chem. 1995;270:30749–30754. doi: 10.1074/jbc.270.51.30749. [DOI] [PubMed] [Google Scholar]
- 5.Kudo I, Murakami M, Hara S, Inoue K. Biochim Biophys Acta. 1993;1170:217–231. doi: 10.1016/0005-2760(93)90003-r. [DOI] [PubMed] [Google Scholar]
- 6.Murakami M, Kudo I, Inoue K. J Lipid Mediators. 1995;12:119–130. doi: 10.1016/0929-7855(95)00013-g. [DOI] [PubMed] [Google Scholar]
- 7.Barbour S E, Dennis E A. J Biol Chem. 1993;268:21875–21882. [PubMed] [Google Scholar]
- 8.Pfeilschifter J, Schalkwijk C, Briner V A, van den Bosch H. J Clin Invest. 1993;92:2516–2523. doi: 10.1172/JCI116860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murakami M, Kudo I, Inoue K. J Biol Chem. 1993;268:839–844. [PubMed] [Google Scholar]
- 10.Fonteh A N, Bass D A, Marshall L A, Seeds M, Samet J M, Chilton F H. J Immunol. 1994;152:5438–5446. [PubMed] [Google Scholar]
- 11.Reddy S T, Herschman H R. J Biol Chem. 1996;271:186–191. doi: 10.1074/jbc.271.1.186. [DOI] [PubMed] [Google Scholar]
- 12.Balsinde J, Barbour S E, Bianco I D, Dennis E A. Proc Natl Acad Sci USA. 1994;91:11060–11064. doi: 10.1073/pnas.91.23.11060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Balsinde J, Dennis E A. J Biol Chem. 1996;271:6758–6765. doi: 10.1074/jbc.271.12.6758. [DOI] [PubMed] [Google Scholar]
- 14.Balboa M A, Balsinde J, Winstead M V, Tischfield J A, Dennis E A. J Biol Chem. 1996;271:32381–32384. doi: 10.1074/jbc.271.50.32381. [DOI] [PubMed] [Google Scholar]
- 15.Herschman H R. Biochim Biophys Acta. 1996;1299:125–140. doi: 10.1016/0005-2760(95)00194-8. [DOI] [PubMed] [Google Scholar]
- 16.Tischfield J A. J Biol Chem. 1997;272:17247–17250. doi: 10.1074/jbc.272.28.17247. [DOI] [PubMed] [Google Scholar]
- 17.Reddy S R, Herschman H R. J Biol Chem. 1997;272:3231–3237. doi: 10.1074/jbc.272.6.3231. [DOI] [PubMed] [Google Scholar]
- 18.Reddy S R, Winstead M W, Tischfield J A, Herschman H R. J Biol Chem. 1997;272:13591–13596. doi: 10.1074/jbc.272.21.13591. [DOI] [PubMed] [Google Scholar]
- 19.Reddy S R, Herschman H R. J Biol Chem. 1994;269:15473–15480. [PubMed] [Google Scholar]
- 20.Murakami M, Matsumoto R, Austen K F, Arm J P. J Biol Chem. 1994;269:22269–22275. [PubMed] [Google Scholar]
- 21.Bingham C O, Murakami M, Fujishima H, Hunt J E, Austen K F, Arm J P. J Biol Chem. 1996;271:25936–25944. doi: 10.1074/jbc.271.42.25936. [DOI] [PubMed] [Google Scholar]
- 22.Murakami M, Kuwata H, Amakasu Y, Shimbara S, Nakatani Y, Atsumi G, Kudo I. J Biol Chem. 1997;272:19891–19897. doi: 10.1074/jbc.272.32.19891. [DOI] [PubMed] [Google Scholar]
- 23.Fourcade O, Simon M F, Viodé C, Rugani N, Leballe F, Ragab A, Fournié B, Sarda L, Chap H. Cell. 1995;80:919–927. doi: 10.1016/0092-8674(95)90295-3. [DOI] [PubMed] [Google Scholar]
- 24.Balsinde J, Balboa M A, Dennis E A. J Biol Chem. 1997;272:20373–20377. doi: 10.1074/jbc.272.33.20373. [DOI] [PubMed] [Google Scholar]
- 25.Glaser K B, Asmis R, Dennis E A. J Biol Chem. 1990;265:8658–8664. [PubMed] [Google Scholar]
- 26.Futaki N, Takahashi S, Yokoyama M, Arai I, Higuchi S, Otomo S. Prostaglandins. 1994;47:55–59. doi: 10.1016/0090-6980(94)90074-4. [DOI] [PubMed] [Google Scholar]
- 27.Murakami M, Nakatani Y, Kudo I. J Biol Chem. 1996;271:30041–30051. doi: 10.1074/jbc.271.47.30041. [DOI] [PubMed] [Google Scholar]
- 28.Suga H, Murakami M, Kudo I, Inoue K. J Biochem (Tokyo) 1995;118:939–945. doi: 10.1093/jb/118.5.939. [DOI] [PubMed] [Google Scholar]
- 29.Balsinde J, Bianco I D, Ackermann E J, Conde-Frieboes K, Dennis E A. Proc Natl Acad Sci USA. 1995;92:8527–8531. doi: 10.1073/pnas.92.18.8527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Balsinde J, Dennis E A. Eur J Biochem. 1996;235:480–485. doi: 10.1111/j.1432-1033.1996.00480.x. [DOI] [PubMed] [Google Scholar]
- 31.Asmis R, Dennis E A. Ann N Y Acad Sci. 1994;744:1–10. doi: 10.1111/j.1749-6632.1994.tb52718.x. [DOI] [PubMed] [Google Scholar]