Abstract
In the last decade the development of a number of biological therapies has revolutionised the treatment of rheumatic diseases. The first and most widely used of these approaches, tumour necrosis factor (TNF) blockade (infliximab, entanercept, adalimumab), has now been administered to over a million patients. However, the success of these biological therapies has also highlighted their limitations. None of these treatments has shown a 100% patient response; normally responses are in the 50–70% range. As proteins, these drugs cannot be given orally and they are expensive to produce, a cost ultimately borne by the patient/health provider that can seriously limit the availability of these drugs. Lastly, these treatments, whether involving the systemic neutralisation of a cytokine (eg, TNF or IL6 receptor blockade (tocilizumab)), the ablation of a B cell population (anti‐CD20, rituximab), or the potential disruption of important cellular interactions as with CTLA4‐Ig (abatacept), can cause major perturbations of the immune system, the long‐term effects of which are still unclear. At present, treatments such as TNF blockade can result in an increased infectious risk and the reactivation of tuberculosis can be a major issue in certain populations. As with all therapies, there is an increasing large refractory population over time. Therefore, despite the undoubted success of these therapies, there is room for improvement. Although it might be too much to expect any new treatment to affect a “cure” (all the current biological therapies require repeated administrations), there are definite gains to be made in terms of cost, oral bioavailability and a more selective interference with the immune–inflammatory response.
An important consequence of the success of biological therapies has been to validate the role of various cytokines and cells in the pathophysiology of rheumatoid arthritis (RA). The clinical results obtained with TNF blockade has confirmed in many ways the preclinical studies that originally indicated that TNF was a key regulator of the inflammatory cascade in RA. This includes the production of other cytokines such as IL6, angiogenesis, adhesion molecules and consequent cell migration, and the production of matrix metalloproteinases (MMP) and other factors involved in tissue destruction.1,2
A consequence of the success of blocking TNF has been to focus attention on finding suitable “drugable” targets, either proximal or distal of this cytokine. This quest of “drugability” has focused research on the signalling pathways associated with cytokine production or action. So far two enzymes have clearly led the field as potential targets, p38MAPK and IKK2. Both targets have the perceived benefit of being involved in the production and actions of TNF. IKK2 is a key enzyme in the activation of the NF‐κB transcription factor that is required for the production of many other inflammatory factors.3,4 p38MAPK is mainly implicated in the production of TNF through the post‐transcription regulation including the stabilisation of mRNA; it is also involved in the regulation of TNF in RA.5 However, despite both enzymes being identified some time ago, IKK2 in 19976 and p38MAPK in 1994,7 no compound has yet succeeded in the clinic. To our knowledge, the most advanced p38MAPK inhibitors have reached phase II where progress has stopped, usually due to toxicity. Whether this toxicity is target‐related or not is unclear, however, deletion of the α isoform of p38MAPK is embryonically lethal in mice.8 A clear confirmation of the wealth of published data from in vitro studies indicate that this enzyme is very widely distributed and has a role in multiple pathways of physiological importance.9 Similarly, the deletion of IKK2 from mice also leads to embryonic lethality,10 this may not be so surprising an observation given that cell survival is among the multiple roles of NF‐κB activation. There is the suspicion therefore that systemic inhibition of either of these enzymes with an acceptable toxicity profile may be a difficult goal to achieve.
The quest for the mechanisms inducing TNF production in RA, the basis of disease chronicity
Another major question that has arisen from the biological therapies is that in general they do not achieve a permanent remission of the disease. Anti‐TNF approaches require repeated administration as much as twice weekly (entanercept) and once every 8 weeks for the longer‐lived antibodies such as infliximab. The factors that drive TNF production would appear to be still active and unaffected by these treatments. Therefore the identification of the pathways driving the production of TNF would not only move our understanding closer to the source of the chronicity of RA, but also potentially provide a better therapeutic target. Inhibiting the inducer(s) of TNF production would provide a more selective suppression of TNF than the systemic neutralisation of the cytokine. This should have benefits in terms of safety. Of course, in RA where there are likely to be multiple complex interactions between various cell types and soluble factors, there may be no single stimulus driving cytokine production in all patients. Previously, studies from this laboratory suggest that cytokine‐activated T cells that are generated in the milieu of the cytokine‐rich environment of the inflamed joint are capable of inducing TNF production from macrophages.11 However, other possible candidates are factors that are normally part of the acute inflammatory response against infection. This is even more appealing when one considers that several forms of self‐limiting arthritis are induced by infections such as Lyme disease and chlamydia.12,13
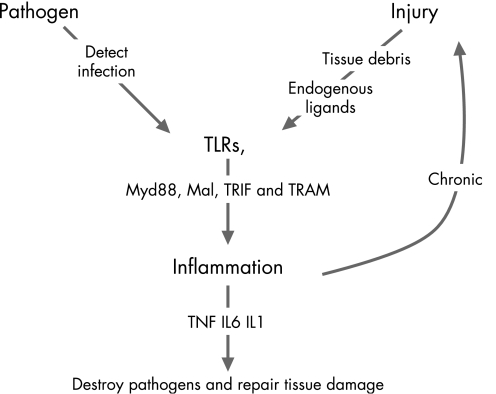
In the last decade there has been a major leap in our understanding of how the host immune system responds to the challenge of infection with the identification of the toll‐like receptor (TLR) family. The toll receptors were first discovered in Drosophila but are now known to be widely expressed in nature and are even present in plants.14,15 Although the original toll receptor was originally identified in flies as a developmental protein, in adults it has a major role in defence against infection, a function replicated by TLRs in many organisms including mammals. To date 14 mammalian TLRs have been identified, 10 of which are found in man. These receptors have a structural homology of leucine‐rich repeats in their extracellular domains, however, they are designed to recognise different ligands, termed PAMPs (pathogen‐associated molecular patterns) (fig 1), that is, molecules that would only be present in the host as the result of the presence of a pathogenic infection. The first identified of these was LPS which is recognised by TLR4.16 Subsequently, TLR2 and the associated TLRs 1 and 6 were shown to recognise proteoglycans, whereas TLR2 in conjunction with the non‐TLR molecule Dectin 1 binds the yeast product zymosan.17 Flagellin is the ligand for TLR5 and TLR9 recognises the non‐methylated CpG rich DNA of bacteria. The other TLRs, 3, 7 and 8, appear to be more concerned with recognising viral infections and, unlike the other TLRs except TLR9, are predominately located in the endosomal compartment rather than on the cell surface.15 To this end, TLR3 and TLR7/8 recognise dsRNA and ssRNA, respectively. The ligand for TLR10 has not been identified. Like LPS, the other TLR ligands are also potent stimulators of inflammation. Normal infection‐induced inflammation is self‐limiting and resolves, but there are instances as in septic shock, acute respiratory distress syndrome and cerebral malaria where a failure to regulate the inflammatory response leads it to become part of the pathology.
Figure 1 Toll‐like receptors: a link between acute and chronic inflammation. TLRs can respond to both endogenous and exogenous ligands leading to the production of inflammatory factors. Damage to cells caused by inflammation may potentially feed back on to the TLRs through generation of endogenous ligands, thus initiating a cyclical pattern that may underlie chronic inflammation.
Could TLRs and their endogenous ligands have a role in RA?
The discovery that the TLRs also recognise endogenous ligands has widened our view of what role these receptors may play in the immune system.18 Most of the ligands identified to date would be generated as products of tissue injury as cell death (fig 1). The potential benefits of such a complimentary activation of the TLR systems are obvious as it would alert the immune system to breaches of physical barriers such as the skin where infectious organisms might enter. However, there is a major downside in that there is the potential for self‐activation of the TLRs. This is possibly the case in sepsis where a major mediator of the exaggerated inflammatory response is the nuclear protein HMGB1.19 This protein induces macrophage activation and TLR2/TLR4 has been implicated in HGMB1 activity.20 Also HMGB1 has been recently shown to bind to extracellular DNA and therefore act as co‐ligand for TLR9.21 This potential of endogenous‐produced ligands to activate the TLRs presents the scenario that inflammation could be driven independently of any external infection where tissue destruction is occurring for some other reason as in cases of chronic inflammation itself (fig 1). Such a possibility has been proposed in systemic lupus erythematosus (SLE) where there is the formation of HMGB1/DNA complexes that could drive inflammation via TLR9.21 In addition to TLR9, TLR7 was also shown to be involved in the pathology of SLE through the recognition of RNA immune complexes which leads to B cell activation in synergy with the B cell receptor.22 Given the amount of tissue destruction that occurs in RA the possibility exists that the self‐generation of TLR ligands would perpetuate and amplify the inflammatory process.23,24
Studies on TLR signalling in RA
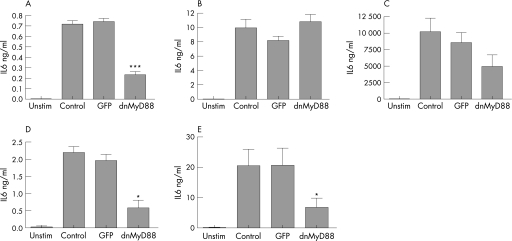
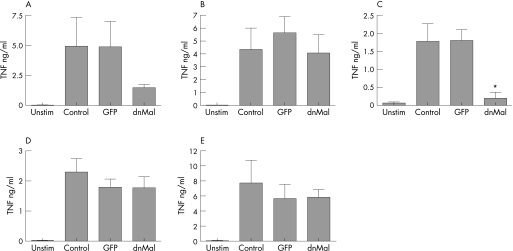
To address whether there was a role of endogenous TLR ligands in driving inflammation in RA we utilised the human RA synovial tissue culture model that was originally used to identify the key role of TNF.25 Rather than attempting to study each individual TLR, we chose to investigate the TLR signalling pathways. Studies in knockout mice have shown that all TLRs, with the exception of TLR3, use the intracellular signalling adaptor molecule Myd88. This protein contains a TIR (Toll/interleukin 1 receptor) domain that forms a homotypic interaction with the TIR domain of the receptor. As the name suggests, the same domain is also found in the IL1 receptor family and, as a consequence, both families use very similar signalling pathways.26 However, there are certain additional receptor complexities concerning TLR signalling over and above that of IL1. Although TLRs 5, 7, 8 and 9, like IL1 just use Myd88, TLR 1/2/6 and 4 also use a related adaptor molecule, Mal/TIRAP. As a further complexity, TLR4 also engages two further adaptors, TRAM and TRIF, the latter also being the only signalling adaptor used by TLR3.26 To address the role of TLR signalling in RA membranes, we generated the dominant negative version of Myd88 (dnMyd88) that would neutralise all TLRs (except TLR3) and IL1 signalling, and dominant negative Mal (dnMal) that would allow differentiation from IL1 signalling at least in the case of TLR1, 2, 4 and 6. To deliver these dominant negatives to RA tissue we utilised our adenoviral vectors as used previously in other studies.27,28 However, before we assessed the role of these molecules in RA, we investigated the activity of the dominant negatives at blocking TLR signalling on populations of normal human monocyte‐derived macrophages as the role of these molecules has generally been assessed in various knockout mice. As shown in fig 2, dnMyd88 reduced the production of TNF induced by TLR1/2/6 (MALP2 or Pam3‐Cys), TLR5 (Flagellin) and TLR7/8 (R848), and IL1 (not shown). In contrast, dnMal only blocked TLR2 signalling and had no effect on TLR5 or TLR7/8 (fig 3). Unfortunately, these cells do not respond to TLR9 ligands and TLR3 does not induce inflammatory cytokines in human macrophages.29 However, as we have shown previously, TLR4 (LPS) signalling was unimpaired by either dnMyD88 or dnMal.28 The reasons for this are unclear and infection with dominant negatives of Mal and TRAM either alone or in combinations with dnMy88 still failed to inhibit LPS activity in macrophages.27
Figure 2 Overexpression of dnMyD88 inhibits TLR2, 5 and 7/8 signalling in human macrophages. M‐CSF‐derived human macrophages were infected with a dominant negative (dn) MyD88 adenovirus (MOI 100:1) for 1 hour in serum‐free media and then cultured for 24 hours in normal media. Cells were then stimulated with media alone or media containing (A) 3 ng/ml Malp‐2, (B) 1 ng/ml LPS, (C) 10 ng/ml Pam3Cys, (D) 10 μg/ml Flagellin or (E) 1 μg/ml R‐848 for 6 hours. The supernatants were analysed for IL6 by ELISA. Mean cytokine production (±SEM) of triplicate cultures from three unrelated donors is shown. For the statistical analysis, a one‐tailed Student t test was used to compare uninfected control cells with recombinant adenovirus‐infected cells (*p<0.05, ***p<0.001).
Figure 3 Overexpression of dnMal inhibits TLR2 signalling in human macrophages. M‐CSF‐derived human macrophages were infected with dominant negative (dn) Mal adenovirus (MOI 100:1) for 1 hour in serum‐free media and then cultured for 24 hours in normal media. Cells were then stimulated with media alone or media containing (A) 3 ng/ml Malp‐2, (B) 1 ng/ml LPS, (C) 10 ng/ml Pam3Cys, (D) 10 μg/ml Flagellin or (E) 1 μg/ml R‐848 for 6 hours. The supernatants were analysed by ELISA for TNF. Mean cytokine production (±SEM) of triplicate cultures from three unrelated donors is shown. For the statistical analysis, a one‐tailed Student t test was used to compare uninfected control cells with recombinant adenovirus‐infected cells (*p<0.05).
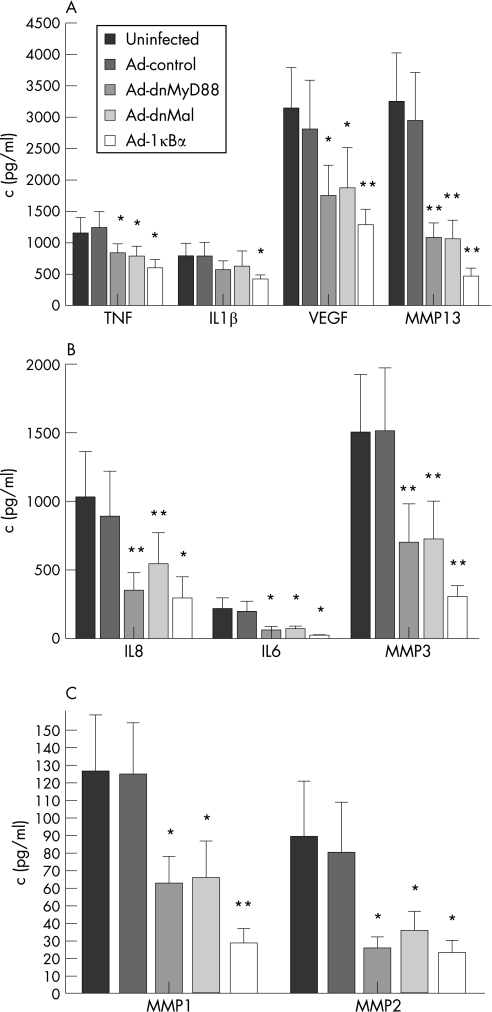
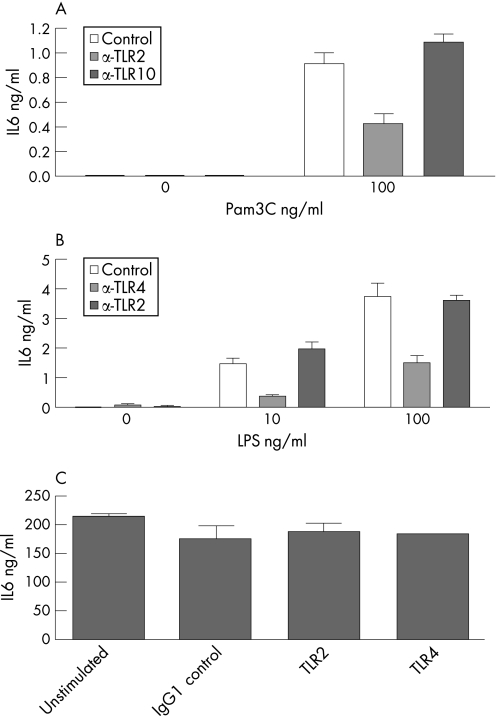
Having established the activity of these inhibitory constructs in a simple TLR system, we applied the same reagents to studies on culture of primary human synovial tissue. As has been previously described, these spontaneously produce TNF, other cytokines, MMPs and other inflammatory mediators in the absence of any exogenous stimulus.30 The factors driving the production of TNF are not yet defined. As shown in fig 4, infecting the cells with a control virus had no effect on the production of TNF or IL6 compared to uninfected controls. In contrast, the use of a viral vector encoding IκBα that would specifically inhibit the NF‐κB pathway4 reduced the level of TNF and other cytokines by 50–70% except for IL6 that was inhibited by over 90%. Dominant negative Myd88 reduced the production of both TNF and IL1 by approximately 30%, although the latter was not significant. IL6 and IL8 production was reduced by 60–70% and VEGF by approximately 50%. Studies with dnMal produced similar levels of inhibition of all these cytokines compared to dnMyD88. We also looked at the effect of inhibiting TLR signalling on the expression of several MMPs. As shown in fig 4, dnMyd88 and dnMAL both reduced the production of all the MMPs by 50–70%. These data would indicate that there is a role for both the Myd88 and Mal signalling pathways in the production of TNF and, more so, IL6 in these RA membranes. While a role for Myd88 would suggest IL1 as well as the TLRs, the role of Mal would indicate an important role for TLR signalling, although a contribution from IL1 signalling might also be present. Given these results, we investigated whether TLR2 or TLR4 were involved in driving cytokine production in RA membranes. Antibodies to TLR2 and TLR4 are able to block the response of human macrophages to PAM3Cys or LPS, respectively (fig 5A, B). However, these antibodies were unable to block the spontaneous production of cytokines in the synovial membranes (fig 5C).
Figure 4 Overexpression of dnMyD88 or dnMal inhibits spontaneous cytokine and MMP production in rheumatoid synovial membranes. Rheumatoid synovial membrane cultures were infected with adenoviruses containing dnMyD88, dnMal and IκBα for 1 hour in serum‐free media and the viruses were removed and replaced with normal media. Supernatants were collected after 48 hours and levels of (A) TNFα, IL1, VEGF, MMP13; (B) IL8, IL6, MMP3, and (C) MMP1, MMP2 were measured by ELISA. Concentration of cytokine production from six to eight unrelated patients is shown. For the statistical analysis a one‐tailed Student t test was used to compare uninfected control cells with recombinant adenovirus‐infected cells (*p<0.05, **p<0.01).
Figure 5 Spontaneous IL6 production from RA synovial membrane cultures is not inhibited by TLR2 or TLR4 blocking antibodies. Macrophages were generated from peripheral blood monocytes in culture with 100 ng/ml M‐CSF for 3 days. (A) Macrophages were left untreated or incubated for 1 hr with 10 μg/ml isotype control antibody or 10 μg/ml α‐TLR2 and then stimulated with 10 and 100 ng/ml Pam3Cys‐Ser‐Lys4 for 18 hrs. (B) Macrophages were left untreated or incubated for 1 hr with 10 μg/ml α‐TLR2 or 10 μg/ml α‐TLR4 and then stimulated with 0.5 or 1 ng/ml LPS for 18hrs. (C) RA synovial membrane cells were cultured with 10 μg/ml isotype control, α‐TLR2 or α‐TLR4 for 48 hrs, n = 5. Mean cytokine production (±SD) of triplicate cultures is shown and is representative of three independent experiments from unrelated donors in parts A and B, and five in part C.
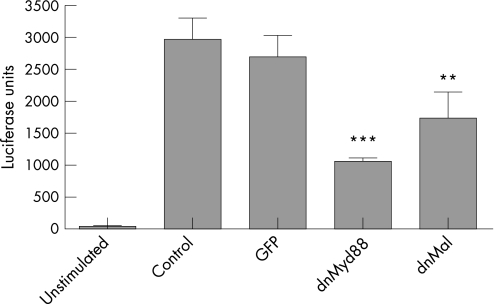
Given this result, we next investigated whether these TLR ligands might exist within the culture supernatants of these cultures. This is a relatively tricky experiment as the culture supernatant already contains cytokines. To investigate the presence of TLR ligands we utilised naive primary human macrophages that contained an NF‐κB luciferase reporter gene construct. Luciferase activity will be induced in these cells by all the TLRs except 3 and 9 (data not shown). To ascertain if any induction of NF‐κB by the synovial joint culture supernatants could be attributable to TLR ligands, the cells were co‐infected with viruses for dnMyd88 or dnMal. As shown in fig 6, dnMyd88 and, to a lesser degree, dnMal inhibited the activation of the NF‐κB luciferase reporter. As might be expected for cultures that would also contain IL1 and ligands for TLRs that do not use Mal, the effect of dnMal was less than that of dnMyd88. Also neither inhibitor produced a complete inhibition as also would be expected as these supernatants also contain other activators of NF‐κB such as TNF that do not use the TLR/IL1 signalling pathway. Therefore, although the antibodies to TLR2 and TLR4 failed to block the spontaneous release of cytokines in RA membranes, there clearly are ligands for TLRs present in these cultures. At present our work is progressing to discover which TLRs are being activated by these potential ligands.
Figure 6 Overexpression of dnMyD88 or dnMal inhibits the activation of NFκB in human macrophages stimulated with the supernatant of rheumatoid membrane cell culture. Human M‐CSF macrophages were infected with an adenovirus expressing a NF‐κB luciferase reporter (MOI 50:1) in SF media for 1 hour. Four hours later cells were either untreated or additionally infected with a GFP control adenovirus or one expressing dnMyD88 or dnMal (MOI 100:1). After 24 hours cells were stimulated with conditioned supernatant generated from incubation with rheumatoid membrane cell cultures over 24 hours and then filtered to remove any cell debris. Absolute luciferase units ± SD of triplicate cultures are shown. For the statistical analysis a one‐tailed Student t test was used to compare uninfected control cells with recombinant adenovirus‐infected cells (**p<0.01, ***p<0.001).
Conclusions
Our data would indicate that there is a potential role for the TLR system in driving the inflammatory and destructive processes in RA. It may not be necessary for TLRs to be involved in the inception of disease (although this could be via micro‐organisms), but they could greatly contribute to chronicity through cycles of inflammation, disease destruction and further inflammation (fig 1). This activity may not be confined to a single TLR as several could be involved. Ongoing studies in this group are attempting to define which TLRs might be involved and the nature of the ligands being recognised. Are TLRs a therapeutic target? Assuming that a substantial proportion of the TNF‐inducing activity is not spread among too many TLRs, then inhibition of one or two might produce a significant enough reduction in TNF to have a therapeutic benefit. In terms of safety that would potentially be a more selective suppression of TNF production than is obtained with TNF blockade, although this cannot really be assessed until actual human studies with an acceptable TLR inhibitor could be performed. Moreover, side effects through inhibiting one or several TLRs may be limited as other pattern recognition receptors such as nucleotide‐binding oligomerisation domains, C‐type lectin receptors and retinoic acid‐induced gene I would still be left intact. A further indication for the feasibility of TLR inhibition as a therapy in terms of its side effects comes from humans with a mutation in the irak4 gene. IRAK4 is a common mediator of TLR signalling and, although individuals with mutated IRAK4 show severe infections in early childhood, this phenotype dissipates with age suggesting additional TLR‐independent, protective mechanisms taking over.31,32,33 TLRs, unlike many receptor systems, might be amenable to inhibition by small molecular weight compounds that would have an advantage over kinase inhibitors in that cell permeability is not a requirement or even desirable. Therefore the likelihood of off‐target effects could be greatly reduced.
Abbreviations
MMP - matrix metalloproteinases
PAMPs - pathogen‐associated molecular patterns
RA - rheumatoid arthritis
SLE - systemic lupus erythematosus
TIR - toll/interleukin 1 receptor
TLR - toll‐like receptor
TNF - tumour necrosis factor
Footnotes
Competing interests: None declared.
References
- 1.Maini R N, Feldmann M. How does infliximab work in rheumatoid arthritis? Arthritis Res 20024(Suppl 2)S22–S28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Feldmann M, Maini R N. Lasker Clinical Medical Research Award. TNF defined as a therapeutic target for rheumatoid arthritis and other autoimmune diseases. Nat Med 200391245–1250. [DOI] [PubMed] [Google Scholar]
- 3.Barnes P J, Karin M. Nuclear factor‐kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 19973361066–1071. [DOI] [PubMed] [Google Scholar]
- 4.Foxwell B, Browne K, Bondeson J, Clarke C, de Martin R, Brennan F.et al Efficient adenoviral infection with IkappaB alpha reveals that macrophage tumor necrosis factor alpha production in rheumatoid arthritis is NF‐kappaB dependent. Proc Natl Acad Sci USA 1998958211–8215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Campbell J, Ciesielski C J, Hunt A E, Horwood N J, Beech J T, Hayes L A.et al A novel mechanism for TNF‐alpha regulation by p38 MAPK: involvement of NF‐kappa B with implications for therapy in rheumatoid arthritis. J Immunol 20041736928–6937. [DOI] [PubMed] [Google Scholar]
- 6.DiDonato J A, Hayakawa M, Rothwarf D M, Zandi E, Karin M. A cytokine‐responsive IkappaB kinase that activates the transcription factor NF‐kappaB. Nature 1997388548–554. [DOI] [PubMed] [Google Scholar]
- 7.Han J, Lee J D, Bibbs L, Ulevitch R J. A MAP kinase targeted by endotoxin and hyperosmolarity in mammalian cells. Science 1994265808–811. [DOI] [PubMed] [Google Scholar]
- 8.Allen M, Svensson L, Roach M, Hambor J, McNeish J, Gabel C A. Deficiency of the stress kinase p38alpha results in embryonic lethality: characterization of the kinase dependence of stress responses of enzyme‐deficient embryonic stem cells. J Exp Med 2000191859–870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ashwell J D. The many paths to p38 mitogen‐activated protein kinase activation in the immune system. Nat Rev Immunol 20066532–540. [DOI] [PubMed] [Google Scholar]
- 10.Tanaka M, Fuentes M E, Yamaguchi K, Durnin M H, Dalrymple S A, Hardy K L.et al Embryonic lethality, liver degeneration, and impaired NF‐kappa B activation in IKK‐beta‐deficient mice. Immunity 199910421–429. [DOI] [PubMed] [Google Scholar]
- 11.Brennan F, Foey A. Cytokine regulation in RA synovial tissue: role of T cell/macrophage contact‐dependent interactions. Arthritis Res 20024(Suppl 2)S177–S182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zeidler H, Kuipers J, Kohler L. Chlamydia‐induced arthritis. Curr Opin Rheumatol 200416380–392. [DOI] [PubMed] [Google Scholar]
- 13.Franz J K, Krause A. Lyme disease (Lyme borreliosis). Best Pract Res Clin Rheumatol 200317241–264. [DOI] [PubMed] [Google Scholar]
- 14.Beutler B, Rehli M. Evolution of the TIR, tolls and TLRs: functional inferences from computational biology. Curr Top Microbiol Immunol 20022701–21. [DOI] [PubMed] [Google Scholar]
- 15.Trinchieri G, Sher A. Cooperation of Toll‐like receptor signals in innate immune defence. Nat Rev Immunol 20077179–190. [DOI] [PubMed] [Google Scholar]
- 16.Poltorak A, He X, Smirnova I, Liu M Y, Van Huffel C, Du X.et al Defective LPS signaling in C3H/HeJ and C57BL/10ScCr mice: mutations in Tlr4 gene. Science 19982822085–2088. [DOI] [PubMed] [Google Scholar]
- 17.Netea M G, Gow N A, Munro C A, Bates S, Collins C, Ferwerda G.et al Immune sensing of Candida albicans requires cooperative recognition of mannans and glucans by lectin and Toll‐like receptors. J Clin Invest 20061161642–1650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marshak‐Rothstein A. Toll‐like receptors in systemic autoimmune disease. Nat Rev Immunol 20066823–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lotze M T, Tracey K J. High‐mobility group box 1 protein (HMGB1): nuclear weapon in the immune arsenal. Nat Rev Immunol 20055331–342. [DOI] [PubMed] [Google Scholar]
- 20.Yu M, Wang H, Ding A, Golenbock D T, Latz E, Czura C J.et al HMGB1 signals through toll‐like receptor (TLR) 4 and TLR2. Shock 200626174–179. [DOI] [PubMed] [Google Scholar]
- 21.Tian J, Avalos A M, Mao S Y, Chen B, Senthil K, Wu H.et al Toll‐like receptor 9‐dependent activation by DNA‐containing immune complexes is mediated by HMGB1 and RAGE. Nat Immunol 20078487–496. [DOI] [PubMed] [Google Scholar]
- 22.Marshak‐Rothstein A, Rifkin I R. Immunologically active autoantigens: the role of toll‐like receptors in the development of chronic inflammatory disease. Annu Rev Immunol 200725419–441. [DOI] [PubMed] [Google Scholar]
- 23.Ospelt C, Neidhart M, Gay R E, Gay S. Synovial activation in rheumatoid arthritis. Front Biosci 200492323–2334. [DOI] [PubMed] [Google Scholar]
- 24.Andreakos E, Sacre S, Foxwell B M, Feldmann M. The toll‐like receptor‐nuclear factor kappaB pathway in rheumatoid arthritis. Front Biosci 2005102478–2488. [DOI] [PubMed] [Google Scholar]
- 25.Brennan F M, Chantry D, Jackson A, Maini R, Feldmann M. Inhibitory effect of TNF alpha antibodies on synovial cell interleukin‐1 production in rheumatoid arthritis. Lancet 19892244–247. [DOI] [PubMed] [Google Scholar]
- 26.O'Neill L A, Bowie A G. The family of five: TIR‐domain‐containing adaptors in Toll‐like receptor signalling. Nat Rev Immunol 20077353–364. [DOI] [PubMed] [Google Scholar]
- 27.Sacre S M, Lundberg A M, Andreakos E, Taylor C, Feldmann M, Foxwell B M. Selective use of TRAM in lipopolysaccharide (LPS) and lipoteichoic acid (LTA) induced NF‐kappaB activation and cytokine production in primary human cells: TRAM is an adaptor for LPS and LTA signaling. J Immunol 20071782148–2154. [DOI] [PubMed] [Google Scholar]
- 28.Andreakos E, Sacre S M, Smith C, Lundberg A, Kiriakidis S, Stonehouse T.et al Distinct pathways of LPS‐induced NF‐kappa B activation and cytokine production in human myeloid and nonmyeloid cells defined by selective utilization of MyD88 and Mal/TIRAP. Blood 20041032229–2237. [DOI] [PubMed] [Google Scholar]
- 29.Lundberg A M, Drexler S K, Monaco C, Williams L M, Sacre S M, Feldmann M.et al Key differences in TLR3/POLY1: C signaling and cytokine induction by human primary cell: a phenomenon absent from murine cell systems. Blood. 2007 Jul 27; Epub ahead of print [DOI] [PubMed]
- 30.Brennan F M, Chantry D, Jackson A M, Maini R N, Feldmann M. Cytokine production in culture by cells isolated from the synovial membrane. J Autoimmun 19892(Suppl)177–186. [DOI] [PubMed] [Google Scholar]
- 31.Medvedev A E, Lentschat A, Kuhns D B, Blanco J C, Salkowski C, Zhang S.et al Distinct mutations in IRAK‐4 confer hyporesponsiveness to lipopolysaccharide and interleukin‐1 in a patient with recurrent bacterial infections. J Exp Med 2003198521–531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Picard C, Puel A, Bonnet M, Ku C L, Bustamante J, Yang K.et al Pyogenic bacterial infections in humans with IRAK‐4 deficiency. Science 20032992076–2079. [DOI] [PubMed] [Google Scholar]
- 33.Kuhns D B, Long Priel D A, Gallin J I. Endotoxin and IL‐1 hyporesponsiveness in a patient with recurrent bacterial infections. J Immunol 19971583959–3964. [PubMed] [Google Scholar]