Abstract
Background
Macrolides display immunomodulatory effects that may be beneficial in chronic inflammatory pulmonary diseases. The aim of the study was to document whether long term use of azithromycin may be associated with respiratory benefits in young patients with cystic fibrosis.
Methods
A multicentre, randomised, double blind, placebo controlled trial was conducted from October 2001 to June 2003. The criteria for enrolment were age older than 6 years and forced expiratory volume in 1 second (FEV1) of 40% or more. The active group received either 250 mg or 500 mg (body weight < or ⩾40 kg) of oral azithromycin three times a week for 12 months. The primary end point was change in FEV1.
Results
Eighty two patients of mean (SD) age 11.0 (3.3) years and mean (SD) FEV1 85 (22)% predicted were randomised: 40 in the azithromycin group and 42 in the placebo group. Nineteen patients were infected with Pseudomonas aeruginosa. The relative change in FEV1 at month 12 did not differ significantly between the two groups. The number of pulmonary exacerbations (count ratio 0.50 (95% CI 0.32 to 0.79), p<0.005), the time elapsed before the first pulmonary exacerbation (hazard ratio 0.37 (95% CI 0.22 to 0.63), p<0.0001), and the number of additional courses of oral antibiotics were significantly reduced in the azithromycin group regardless of the infectious status (count ratio 0.55 (95% CI 0.36 to 0.85), p<0.01). No severe adverse events were reported.
Conclusion
Long term use of low dose azithromycin in young patients with cystic fibrosis has a beneficial effect on lung disease expression, even before infection with Pseudomonas aeruginosa.
Keywords: children, cystic fibrosis, azithromycin, lung function, respiratory exacerbation
Cystic fibrosis (CF) is an autosomal recessive disorder characterised by multiple organ dysfunction, especially progressive lung disease, pancreatic insufficiency, and increased sweat electrolyte concentrations. The CF transmembrane conductance regulator (CFTR) gene codes for a protein that functions as a chloride channel in epithelial membranes. Morbidity and mortality from CF are commonly due to loss of lung function, which inexorably follows a chronic course of inflammation, bacterial infection, and airway obstruction.1,2 For a long time it has been thought that the ineffective clearance of bacteria from CF airways was primary to pathogenesis, leading secondarily to lung inflammation. However, there is now growing evidence that exaggerated inflammation is present in the airways very early on, possibly even before infection.3,4 The lung inflammatory response is persistently neutrophilic, with upregulation of neutrophil chemotactic mediators. Accumulation of activated neutrophils with release of toxic products impairs host defence, contributing to subsequent chronic infection by microorganisms such as Pseudomonas aeruginosa. Amplification of the vicious cycle of inflammation/infection leads to progressive lung destruction.5,6
As inflammation is a central contributor to the pathogenesis of CF pulmonary disease, limiting the excessive production of inflammatory mediators represents a major therapeutic strategy for slowing the decline in lung function and improving survival. A compelling rationale for the use of non‐steroidal anti‐inflammatory drugs, together with encouraging results of macrolide antibiotics in various chronic inflammatory pulmonary disorders such as diffuse panbronchiolitis and asthma, have led to the use of these agents in CF, mainly for their anti‐inflammatory properties.7,8,9 Unlike their anti‐infective actions, the immunomodulatory effects of the 14‐ and 15‐membered ring macrolide antibiotics are expressed at lower doses and usually after a relatively prolonged period of treatment. The largest study to date using low dose macrolides was conducted in adult CF patients chronically infected with P aeruginosa and indicated improvement in clinical parameters and pulmonary function after 6 months of treatment.10
It is important to know whether macrolides may be beneficial at an early stage of CF disease to support their use as anti‐inflammatory agents in young children. We therefore designed a multicentre, randomised, double blind, placebo controlled trial to investigate the effects of 12 months of treatment with low dose azithromycin on lung disease progression.
Methods
Patients
Eighteen CF accredited care centres in France participated in the trial which was coordinated and sponsored by the French CF Association Vaincre la Mucoviscidose. The study was approved by the medical ethics committee of Paris and written informed consent was obtained for each participant and/or their parents/guardians before entry.
The criteria for enrolment were a diagnosis of CF (sweat chloride >60 mmol/l or a genotype known to cause the disease), age 6–21 years, ability to perform reproducible pulmonary function tests with spirometry, forced expiratory volume in 1 second (FEV1) >40% of the predicted value, and ability to swallow tablets. Exclusion criteria were allergy to macrolide antibiotics, long term treatment (>3 months) with macrolides during the 12 month period before study entry, liver disease with liver function tests more than twice the laboratory upper limit, history of portal hypertension, kidney disease with serum creatinine >150 μmol/l and/or creatinine clearance <50 ml/min, introduction of recombinant human dornase alfa (rhDNase) and/or inhaled tobramycin and/or inhaled steroids in the 3 months before study entry.
Study design and procedures
The study was a double blind, randomised, multicentre trial of 12 months' duration. Patients were recruited by a local investigator in every centre and eligibility was assessed at an initial screening visit. Patients were randomised at a subsequent pretreatment visit and baseline clinical information was recorded. Randomisation was stratified according to centre and P aeruginosa infection status. P aeruginosa infection was defined as at least three consecutive positive sputum cultures. The allocation sequence was generated by a centralised secure randomisation department not participating in the trial and a study number was assigned by an interactive voice response system. The blinded drug kits assigned to the patients were provided at the study centers at the time of enrolment and at each clinic visit. The study preparations were delivered as identically packaged tablets containing either azithromycin or placebo. Azithromycin was supplied as 250 mg tablets. Patients were asked to take one tablet 3 days/week if they weighed less than 40 kg or two tablets if they weighed 40 kg or more. Kits were distributed at each CF centre by the chief pharmacist. The patients and all study investigators remained blinded to the treatment assigned until the study had been completed.
After the entry visit (month 0), patients returned for visits every 2 months until month 12. At each visit patient evaluation included physical examination with weight and height measurements, pulmonary function tests of FEV1 and forced vital capacity (FVC), and microbiological analysis of sputum and throat cultures for the common CF pathogens and mycobacteria as previously described.11 Information on pulmonary exacerbations, adverse events, and treatments was recorded. Acute pulmonary exacerbations were defined as an acute exacerbation of CF respiratory symptoms that, in the opinion of the patient's physician, required administration of new oral or intravenous antibiotics. A pulmonary exacerbation was defined according to criteria published by the 1994 CF Foundation Microbiology and Infectious Disease Consensus Conference as the presence of at least three of the following new findings or changes in clinical status: increased cough, increased sputum production, increased respiratory rate, decreased exercise tolerance, new findings on chest examination, new findings on chest radiograph, reduction in FEV1 by more than 10%, weight loss associated with anorexia and decreased dietary intake, fever on more than one occasion, school or work absenteeism due to illness.12 For monitoring adverse events, reported symptoms, clinical findings and laboratory investigations were recorded when necessary. Two additional pulmonary function tests were performed at months 1 and 11. During the trial, patients continued all standard investigations with a yearly chest radiograph, as well as treatment as prescribed by the care team including antibiotics, pancreatic enzymes, vitamins, and physiotherapy. Blood samples to monitor liver function and creatinine were obtained at the entry visit (month 0) and at the visits at months 6 and 12. A CF quality of life questionnaire was filled out by the patient and/or the parents/guardians at the visits at months 0, 2, and 12.13 Any unused study drug was returned at each visit and pills were counted by the pharmacist as a measure of compliance. Patients who missed taking 30% or more of the total study drug prescribed doses were labelled as non‐compliant but remained included in all analyses along with the compliant patients. The study protocol indicated discontinuation of treatment in the event of severe adverse events.
The primary end point was to determine whether azithromycin treatment was associated with changes in FEV1 % predicted between month 12 and month 0. Secondary end points included evaluation of the number of pulmonary exacerbations, the use of antibiotics, modifications of microbiological analysis of sputum or throat cultures (appearance of new pathogens, bacterial culture densities), changes in FVC, nutritional status with measurement of body mass index (BMI), and quality of life. Percentage predicted values for FEV1 and FVC were computed using modified Knudson equations.14 BMI data were also standardised by computing z scores.15 Time to exacerbation was defined as the period elapsed from the day of randomisation until the day of start of treatment for the first exacerbation. Duration time was censored at the date of the last visit for patients who remained exacerbation free. Pulmonary exacerbations were evaluated either by the number of episodes observed during the effective follow up period or an annual rate estimate by the patient. The use of antibiotics was evaluated either as the number of antibiotic courses or the cumulative days of antibiotic treatment by the patient.
For calculating the sample size it was anticipated that the rate of decrease in FEV1 % predicted would be 2% per year for patients without Paeruginosa infection and 4% for infected patients, on the basis of information provided by the French CF Observatory. We hypothesised that the mean trend slope of FEV1 % over 12 months would be 4% higher in the azithromycin group. Sample size was computed according to formula for longitudinal data analysis developed by Diggle et al with nine measurements.16 In calculating the sample size, a measurement error variance was assumed of 576, a correlation between measurements of 0.82, a two sided test formula and a type 1 error of 5%. Using this estimate, a planned sample size of 121 patients per group provided a power of 90% to detect the anticipated difference between treatments.
Statistical analysis
Trend slopes of quantitative outcomes were estimated and compared using a mixed model approach.17 Adjusted comparisons and tests for interactions taking into account effects due to centre and important characteristics at baseline (P aeruginosa infection status, FEV1 % predicted and z BMI) were also performed. Comparisons of groups for quantitative data were made using Student t tests and adjusted comparisons by analyses of variance. Qualitative data were compared by the χ2 test or the Fisher exact test as appropriate and adjusted comparisons by logistic regression. Count data (the number of pulmonary exacerbations per patient, antibiotic courses per patient, or days of treatment per patient, with a zero count representing the absence of an event) were analysed by Poisson regression analysis. The probability for a patient remaining exacerbation free over time was computed by the Kaplan‐Meier method and comparisons between groups were done by the log‐rank test. Cox regression analyses were used to estimate hazard ratios between groups and to perform adjusted comparisons. Means and regression parameter estimates were expressed with the standard deviation in parentheses. Treatment effect estimates were given with the 95% confidence interval in parentheses.
All comparison tests were two sided and p values <0.05 were considered statistically significant. Statistical analyses were done with SAS Version 8.2 (SAS Institute, Cary, NC, USA). Data analyses were based on an intent‐to‐treat approach that included all randomised patients. For patients who did not complete the protocol, the last observation carried forward (LOCF) approach was used to compute the relative change in quantitative outcome parameters. Other analyses including only patients with at least one follow up (full set analysis according to the ICH E9 guideline, http://www.ich.org) or patients with a complete follow up (per protocol analysis) were performed to study the sensitivity of the results to the considered dataset.
Results
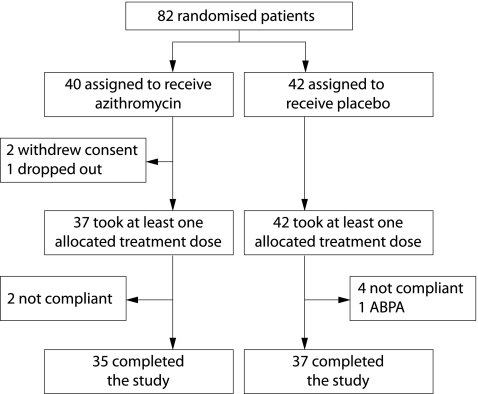
Figure 1 shows the trial profile. Enrolment took place between October 2001 and June 2003. Eighty two patients were randomly assigned in 18 CF centres, 40 to receive azithromycin and 42 placebo. Two patients in the azithromycin group withdrew their consent just after randomisation and one patient was lost to follow up before the first visit. Two patients in the azithromycin group and four in the placebo group were withdrawn by the investigators because they did not take the treatment, and one patient in the placebo group was withdrawn because of severe allergic bronchopulmonary aspergillosis diagnosed during the week after the onset of the study.
Figure 1 Trial flow diagram.
Thirty five azithromycin patients and 37 placebo patients completed the treatment course. On the basis of treatment returned, the estimated adherence was 95% for azithromycin and for placebo. Table 1 shows the baseline characteristics of the patients, with information given for the population as a whole as well as for the subpopulations of patients either not infected or infected with P aeruginosa. There were no significant differences between patients receiving azithromycin or placebo with respect to age, sex, CFTR genotype, nutritional and pancreatic status, lung function, lung microbiology, and concomitant medications at enrolment (rhDNAse, inhaled corticosteroids, inhaled antibiotics).
Table 1 Baseline characteristics of patients.
| Azithromycin | Placebo | |||||
|---|---|---|---|---|---|---|
| Total (n = 40) | Absence of P aeruginosa infection (n = 31) | P aeruginosa infection (n = 9) | Total (n = 42) | Absence of P aeruginosa infection (n = 32) | P aeruginosa infection (n = 10) | |
| Mean (SD) age (years) | 10.9 (3.5) | 10.6 (3.4) | 11.8 (3.9) | 11.1 (3.2) | 10.6 (2.8) | 12.6 (3.9) |
| Sex (M/F) | 24/16 | 20/11 | 4/5 | 22/20 | 18/14 | 4/6 |
| CFTR genotype | ||||||
| ΔF508/ΔF508 | 20 | 15 | 5 | 21 | 16 | 5 |
| ΔF508/others | 17 | 13 | 4 | 15 | 13 | 2 |
| Others and unknown | 3 | 3 | 0 | 6 | 3 | 3 |
| Mean (SD) BMI z score | −0.09 (1.36) | −0.06 (1.46) | −0.16 (0.98) | −0.16 (1.30) | −0.14 (1.21) | −0.22 (1.63) |
| Pancreatic insufficiency | 35 | 26 | 9 | 39 | 30 | 9 |
| Mean (SD) pulmonary function | ||||||
| FEV1 (% predicted) | 86.5 (25.9) | 86.0 (26.3) | 88.2 (26.2) | 84.5 (18.4) | 87.7 (19.0) | 74.6 (12.2) |
| FVC (% predicted) | 94.9 (22.5) | 94.9 (23.4) | 94.9 (20.2) | 94.6 (16.7) | 97.0 (17.4) | 87.0 (12.2) |
| Treatment at enrolment | ||||||
| rhDNase | 20 | 12 | 8 | 26 | 20 | 6 |
| Inhaled corticosteroids | 12 | 8 | 4 | 17 | 12 | 5 |
| Inhaled antibiotics | 11 | 5 | 6 | 15 | 6 | 9 |
CFTR, cystic fibrosis transmembrane regulator; BMI, body mass index; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity
Data are mean (SD) or number (%) unless otherwise indicated.
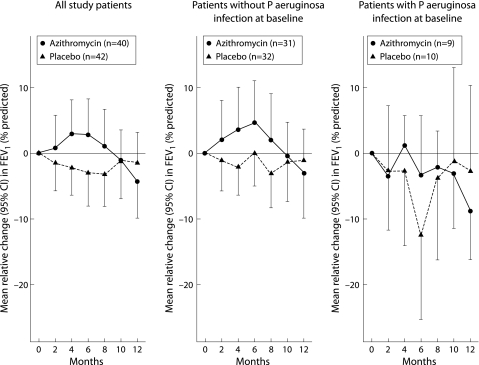
Figure 2 shows the changes in FEV1 % predicted from the start of treatment. No significant difference was recorded between the two treatment groups either in the whole population or in the subpopulations of patients not infected or infected with P aeruginosa. The trend slopes of FEV1 % predicted over 12 months for the population as a whole were not significantly different between azithromycin and placebo (table 2). Results were similar for the subpopulations of patients who were not infected with P aeruginosa and those infected with P aeruginosa. The mean (SD) relative change in FEV1 for the whole population was −4.3 (17.9)% predicted for azithromycin and −1.5 (15.4)% predicted for placebo (table 2). The changes in FVC paralleled those observed for FEV1, with a mean (SD) relative change for the whole population of −1.8 (13.6)% predicted for azithromycin and −4.5 (12.1)% predicted for placebo. Again, there was no significant relative change from baseline in FVC % predicted measured at month 12 in the subpopulations of patients not infected with P aeruginosa and those infected with P aeruginosa.
Figure 2 Mean relative change in FEV1 % predicted from randomisation measurement in the whole population and in the subpopulations of patients not infected or infected with P aeruginosa. The error bars indicate the 95% confidence interval of the mean relative change. No significant difference was recorded between the two treatment groups (azithromycin or placebo), either in the whole population or in the subpopulations of patients not infected or infected with P aeruginosa.
Table 2 Mean (SD) changes in FEV1 and FVC % predicted in the azithromycin and placebo groups during the study.
| Azithromycin | Placebo | Azithromycin−placebo difference estimate (95% CI) | |
|---|---|---|---|
| FEV1 % predicted (%) | |||
| Trend slope over the 12 months | |||
| Total population | −4.9 (2.0) | −1.7 (2.0) | −3.2 (−8.9 to 2.3), NS |
| Patients not infected with PA | −5.0 (2.5) | −1.8 (2.4) | −3.2 (−10.0 to 3.6), NS |
| Patients infected with PA | −4.1 (3.2) | −1.2 (3.1) | −2.9 (−11.7 to 5.8), NS |
| Relative change | |||
| Total population | −4.3 (17.9) | −1.5 (15.4) | −2.8 (−10.1 to 4.5), NS |
| Patients not infected with PA | −3.0 (19.3) | −1.1 (13.5) | −1.9 (−10.3 to 6.5), NS |
| Patients infected with PA | −8.7 (11.5) | −2.7 (21.0) | −6.0 (−22.7 to 10.7), NS |
| FVC % predicted (%) | |||
| Trend slope over the 12 months | |||
| Total population | −2.4 (1.7) | −3.6 (1.7) | 1.2 (−3.4 to 5.8), NS |
| Patients not infected with PA | −2.2 (1.9) | −5.1 (1.9) | 2.9 (−2.3 to 8.2), NS |
| Patients infected with PA | −3.2 (3.3) | 2.2 (3.2) | −5.4 (−14.5 to 3.7), NS |
| Relative change | |||
| Total population | −1.8 (13.6) | −4.5 (12.1) | 2.7 (−3.0 to 8.4), NS |
| Patients not infected with PA | −1.0 (13.3) | −4.3 (9.2) | 3.3 (−2.4 to 9.1), NS |
| Patients infected with PA | −4.3 (15.4) | −4.9 (19.4) | 1.0 (−16.6 to 17.6), NS |
CI, confidence interval; FEV1, forced expiratory volume in 1 second; FVC, forced vital capacity; PA, Pseudomonas aeruginosa; NS, not significant; SD, standard deviation.
Sample sizes in the azithromycin and placebo groups were, respectively, 40 and 42 for the total population, 31 and 32 for patients not infected with PA, and 9 and 10 for patients infected with PA.
The number of pulmonary exacerbations per patient was significantly reduced in the azithromycin group (1.5 (0.29)) compared with the placebo group (3.0 (0.40)), (count ratio azithromycin v placebo 0.50 (95% CI 0.32 to 0.79), p<0.005; table 3). These findings applied to the subpopulation of patients not infected with P aeruginosa (azithromycin: mean 1.3 (0.3); placebo: mean 2.8 (0.4)), (count ratio azithromycin v placebo 0.47 (95% CI 0.27 to 0.81), p<0.01) and to those infected with P aeruginosa (azithromycin: mean 2.1 (0.7); placebo: mean 3.5 (0.9)), (count ratio azithromycin v placebo 0.60 (95% CI 0.27 to 1.36), NS). The rate of pulmonary exacerbations per patient was significantly reduced in the azithromycin group (mean (SD) 1.6 (0.3)) compared with the placebo group (mean (SD) 3.3 (0.4)), (rate ratio azithromycin v placebo 0.50 (95% CI 0.33 to 0.78), p<0.002). Again, these findings applied to the subpopulation of patients not infected with P aeruginosa (azithromycin: mean 1.4 (0.3); placebo: mean 3.0 (0.4)), (rate ratio azithromycin v placebo 0.47 (95% CI 0.28 to 0.79), p<0.005) and to those infected with P aeruginosa (azithromycin: mean 2.4 (0.8); placebo: mean 4.0 (0.9)), (rate ratio azithromycin v placebo 0.60 (95% CI 0.28 to 1.29), NS).
Table 3 Mean (SD) antibiotic use in the azithromycin and placebo groups during the study.
| Azithromycin | Placebo | Count ratio azithromycin/placebo estimate (95% CI) | |
|---|---|---|---|
| Oral antibiotics | |||
| Number of courses | |||
| Total population | 2.1 (0.4) | 3.8 (0.5) | 0.55 (0.36 to 0.85), p<0.01 |
| Patients not infected with PA | 2.1 (0.4) | 3.6 (0.5) | 0.59 (0.36 to 0.98), p<0.05 |
| Patients infected with PA | 2.2 (0.9) | 4.5 (1.2) | 0.49 (0.20 to 1.24), NS |
| Cumulative days of treatment | |||
| Total population | 62 (13) | 74 (13) | 0.85 (0.50 to 1.44), NS |
| Patients not infected with PA | 67 (15) | 67 (15) | 1.00 (0.54 to 1.88), NS |
| Patients infected with PA | 53 (23) | 96 (29) | 0.56 (0.20 to 1.53), NS |
| IV antibiotics | |||
| Number of courses | |||
| Total population | 0.8 (0.2) | 1.6 (0.4) | 0.48 (0.22 to 1.02), NS |
| Patients not infected with PA | 0.4 (0.2) | 0.5 (0.2) | 0.80 (0.30 to 2.13), NS |
| Patients infected with PA | 2.1 (0.8) | 5.2 (1.2) | 0.41 (0.17 to 0.96), p<0.05 |
| Cumulative days of treatment | |||
| Total population | 12 (4) | 24 (5) | 0.51 (0.24 to 1.09), NS |
| Patients not infected with PA | 6 (2) | 6 (2) | 0.95 (0.36 to 2.52), NS |
| Patients infected with PA | 34 (13) | 81 (19) | 0.42 (0.18 to 1.00), p = 0.05 |
SD, standard deviation; CI, confidence interval; PA, Pseudomonas aeruginosa; IV, intravenous; NS, not significant.
Sample sizes in the azithromycin and placebo groups were, respectively, 40 and 42 for the total population, 31 and 32 for the patients not infected with PA, and 9 and 10 for patients infected with PA.
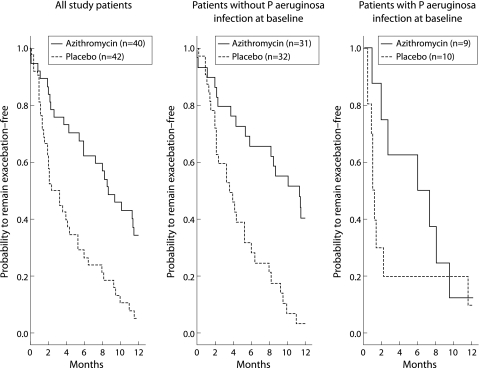
Figure 3 shows that the time to remain free of exacerbations during the study was significantly longer in those receiving azithromycin (median time 8.7 months) than in those given placebo (median time 2.9 months; p<0.0001 (log rank test); hazard ratio azithromycin v placebo 0.37 (95% CI 0.22 to 0.63)). At month 12 the mean (SD) probability of remaining exacerbation free was 34.5 (7.9)% in the azithromycin group compared with 5.3 (3.6)% in the placebo group. For the subpopulation of patients not infected with P aeruginosa, 40.5 (9.3)% remained free of exacerbations when on azithromycin compared with 3.5 (3.5)% of those on placebo (p<0.00001 (log rank test); hazard ratio azithromycin v placebo 0.29 (95% CI 0.15 to 0.55)). For the subpopulation of P aeruginosa infected patients, only one participant treated with either azithromycin or placebo remained free of exacerbations, but the hazard ratio (0.57 (95% CI 0.21 to 1.56)) was not significantly different from 1. The beneficial effect of azithromycin on the occurrence of pulmonary exacerbations was associated with a significant reduction in the need for additional courses of antibiotics during the study. Table 3 gives information on oral and intravenous use of antibiotics from entry to month 12 in the population as a whole as well as in the subpopulations of patients not infected or infected with P aeruginosa. For oral antibiotics, the total number of courses was significantly reduced when patients were receiving azithromycin. The use of intravenous antibiotics was also lower in the azithromycin group, although this reduction did not reach statistical significance.
Figure 3 Probability to remain exacerbation‐free from month 0 to month 12 estimated by the Kaplan‐Meier method. The curves analysed by the log rank test were significantly different (p<0.0001; hazard ratio azithromycin v placebo 0.37 (95% CI 0.22 to 0.63)). At month 12 the mean (SD) probability to remain exacerbation‐free was 34.5 (7.9)% in the azithromycin group and 5.3 (3.6)% in the placebo group. This difference was also observed in the subpopulations of patients not infected or infected with P aeruginosa.
The frequency of positive cultures for all organisms did not differ between the azithromycin and placebo groups during the study. Thirty four patients in the azithromycin group produced respiratory tract samples that could be analysed at baseline compared with 36 in the placebo group. Table 4 gives the number of patients in each group with samples that grew the most common CF pathogens at entry and at month 12. The results of sputum cultures were not different at months 6 and 12, so only the results for month 12 are given in table 4. Similar numbers of positive cultures were recorded throughout the study. Furthermore, no significant difference in the type of micro‐organisms could be documented. Non‐tuberculous mycobacteria were not isolated from any of the study population samples.
Table 4 Lung microbiology at baseline and at month 12.
| Azithromycin | Placebo | |||
|---|---|---|---|---|
| Baseline | Month 12 | Baseline | Month 12 | |
| No of samples analysed | 34 | 31 | 36 | 35 |
| No of samples with positive cultures | 29 | 24 | 29 | 29 |
| No of positive cultures of common CF pathogens | ||||
| Staphylococcus aureus | 19 | 15 | 20 | 20 |
| Methicillin resistant S aureus | 2 | 2 | 5 | 5 |
| Haemophilus influenzae | 6 | 4 | 11 | 9 |
| Pseudomonas aeruginosa | 5 | 3 | 4 | 5 |
| Stenotrophomonas maltophilia | 0 | 1 | 0 | 2 |
| Achromobacter xylosoxidans | 1 | 1 | 1 | 0 |
| Burkholderia cepacia | 1 | 1 | 0 | 0 |
| Aspergillus fumigatus | 3 | 5 | 4 | 5 |
Lung microbiology was documented from respiratory tract samples cultured for the common CF pathogens at baseline and at month 12.
There was no strong evidence of differences resulting from the treatment for nutritional status evaluated by the trend in BMI z scores. The absolute changes in BMI z score were 0.03 (0.40) in the azithromycin group and −0.12 (0.44) in the placebo group (treatment effect 0.15 (95% CI −0.03 to 0.34)). Similar trends in the BMI z score were recorded in the subpopulations of patients not infected with P aeruginosa (0.05 (0.33) for the azithromycin group, −0.13 (0.34) for the placebo group, treatment effect 0.18 (95% CI 0.02 to 0.35)) and those infected with P aeruginosa (−0.05 (0.60) for the azithromycin group and −0.10 (0.69) for the placebo group, treatment effect 0.05 (95% CI −0.58 to 0.67)).
The most frequently observed adverse events (expressed as the number of events in the azithromycin group and in the placebo group, respectively) were abdominal pain (11 and 8), ear/nose/throat infections (14 and 16), diarrhoea (3 and 4), fever (2 and 3), rash (0 and 2), headache (2 and 0), haemoptysis (0 and 2), and vomiting (2 and 0). All events resolved without complication. Assessment of quality of life through the questionnaire indicated no significant differences between the groups in the total score or the physical and psychosocial scores.
We also analysed the stability of all these results to the considered dataset (full set, per protocol set) and the inclusion of potential important covariates and interaction terms in multivariate analyses. These analyses comfirmed the conclusions of the reported results.
Discussion
This randomised placebo controlled trial is the first study of the long term use of low dose azithromycin in young patients with CF. The results showed that treatment for 12 months with oral azithromycin given 3 days a week led to a significant reduction in the number of pulmonary exacerbations requiring courses of antibiotics. Importantly, most of the patients enrolled in the trial were not infected with P aeruginosa, providing evidence that the beneficial effect of azithromycin could be observed at an early stage of lung disease in CF.
The first suggestion that long term macrolide therapy might be of interest in CF was based on the results of low dose erythromycin treatment in patients with diffuse panbronchiolitis.
Following the preliminary report of a pilot study with patients infected with P aeruginosa, several randomised placebo controlled trials were conducted in CF.18 Wolter and colleagues performed a 3 month parallel group trial in 60 CF adult patients (mean age 27.9 years) with a daily dose of 250 mg azithromycin.19 They reported that subjects randomised to azithromycin maintained pulmonary function and experienced a reduced number of pulmonary exacerbations. Saiman and colleagues conducted a 6 month parallel group trial in 185 adult patients infected with P aeruginosa with a dose of 250 or 500 mg azithromycin given 3 days a week.10 They reported improvement in pulmonary function and decreased rates of pulmonary exacerbation in the azithromycin group. So far, no parallel group trial in CF children has been reported. Equi and colleagues conducted a 15 month crossover trial in 41 young patients with CF (mean age 13.8 years) with a daily dose of 250 or 500 mg azithromycin.20 They reported a significant though modest group response in FEV1 to azithromycin. It is important to point out that many of their patients were infected with P aeruginosa and that they did not analyse their results by microbiological status (that is, absence or presence of P aeruginosa).
On the basis of these studies, we selected for the present trial a long term treatment period (12 months) with low dose azithromycin (250 mg or 500 mg adjusted to patient body weight and given only 3 days a week) in young patients with CF. The groups were well matched, with most of the patients not being infected with P aeruginosa. The drug was well tolerated, with good adherence to treatment and similar minor adverse events in the two groups.
We found no difference in the primary end point of change in FEV1. The results showed that the placebo group did not experience an overall decline in FEV1 over the 12 month study period. This observation can be explained by the early stage of the lung disease in the population studied. Indeed, the mean (SD) FEV1 % predicted values at baseline were 84.5 (18.4)% in the placebo group and 86.5 (25.9)% in the azithromycin group. These values were higher than the baseline FEV1 values reported in the other trials mentioned above (60% in the study by Equi and colleagues, 68.3% and 70.6% in the study by Saiman and colleagues, and 62.3% and 50.9% in the study by Wolter and colleagues.10,19,20 In a study reported several years ago, Davis et al observed that a higher initial FEV1 was associated with a greater rate of decline and, among patients with an initial FEV1 >60% predicted, younger subjects had a faster decline than did older subjects.21 Similar conclusions could not be drawn from our results as no significant changes in lung function could be documented in our young CF study population. Certainly, the constant improvement in therapeutic strategies should contribute to reduce the decline in lung function in children. The study protocol did not include measurements of mid‐expiratory flow between 25% and 75% of FVC. Indeed, from other reports on longitudinal analysis of pulmonary function decline in CF, it is most likely that this functional parameter would not have provided different information.22
Another important consideration for analysis of the pulmonary function test results in our population is the large variation in individual FEV1 measurements gathered during the trial. Intra‐individual variability in spirometry has been reported by several authors in patients with CF, mainly in children.23 When the response group was analysed, virtually no decline in the linear trend of FEV1 could be observed in the placebo group, and no significant improvement was found in FEV1 % predicted after 12 months of treatment with azithromycin. Similar findings were also observed for FVC. Interpretation of these data cannot exclude the possibility that the treatment was not continued long enough to detect changes in FEV1 in the final measurements.
Another possibility would be that the study was not adequately powered to document significant differences in FEV1 % predicted after 12 months of treatment with either azithromycin or placebo. With a hypothesis of a 5% difference in change in FEV1 % predicted between the two groups, the estimated sample size would have been 67 patients per group. However, there was no significant relative change from baseline in FEV1 % predicted measured at month 12 in the placebo group. This can be explained by the fact that the patients were young and had mild lung disease, and that nearly 80% were not infected with P aeruginosa. With regard to the sample size, we were able to include 82 patients by the closure of enrolment in June 2003. The main reason was an inaccurate estimation of CF physician attitude regarding the use of azithromycin when the study was conceived and designed. Indeed, the rate at which this drug has been adopted by practitioners has increased rapidly over the past years, most likely because of its potential anti‐inflammatory effects and the absence of significant adverse events related to azithromycin in any of the trials reported to date. Considering the number of patients enrolled in the present trial, the power to statistically detect a difference of 5% in change in FEV1 % predicted between the two groups was estimated to be 72%. Therefore, because of the insufficient number of patients, no clear conclusion with regard to the effect on lung function parameters such as FVC and FEV1 can be drawn from the study.
Periods of relative stability in lung disease expression are classically punctuated by exacerbations of symptoms.24 In the present study the group randomised to receive azithromycin had a significant decrease in the number of pulmonary exacerbations, which paralleled the reduced number of additional courses of antibiotics received by the patients. These results confirm the data reported by the two other double blind, placebo controlled studies performed in adult patients.10,19
Possible explanations for the efficacy of low dose long term macrolide antibiotic therapy in patients with CF include the antibacterial role of these molecules. Azithromycin is an erythromycin derived 15‐membered ring azalide, structurally modified to permit enhanced intracellular accumulation with greater tissue penetration, as well as increased intracellular and extracellular antimicrobial activity.25 However, in the present study, no significant differences were found in the number of positive cultures for the common CF pathogens at months 6 and 12 between the two groups. These results may be explained at least in part by the young age of the patients. Only three patients in the placebo group acquired P aeruginosa. No recent detection of Staphylococcus aureus could be documented in the azithromycin group compared with two in the placebo group (one methicillin sensitive and one methicillin resistant).
The significant difference in the incidence of acute exacerbations between the study groups is an important and, most likely, clinically relevant measure of respiratory benefit in CF patients. The protocols of most therapeutic trials in CF are designed to see if lung function improves. But patients may still benefit even if functional parameters do not change. Interestingly, Saiman and coworkers recently provided additional information on the various effects of azithromycin among the 185 CF participants enrolled in the US trial.10 Their main objective was to describe the heterogeneity of the treatment response in terms of changes in lung function and frequency of pulmonary exacerbations. They showed that participants treated with azithromycin in whom the pulmonary function did not improve still experienced clinical benefits with a reduction in the number of pulmonary exacerbations. These results, which share similarities with our present data, suggest that analysis of changes in FEV1 may not be the most adequate marker for assessing clinical benefits in young CF patients. Despite the well know difficulty of defining a pulmonary exacerbation in CF, the association of new findings or changes in clinical status and antibiotic intervention may be considered as a valuable marker of acute degradation of CF lung disease.26 Clearly, response to treatment in patients with CF needs to be monitored by both functional and exacerbation parameters.
The reduced number of pulmonary exacerbations requiring courses of antibiotics documented in the present study with young CF patients may relate to the anti‐inflammatory properties of azithromycin. A growing body of experimental and clinical evidence indicates that low dose macrolide antibiotics express anti‐inflammatory and tissue reparative effects that are distinct from their antibacterial properties.27 The structure of the 15‐membered ring macrolides promotes interaction of the drug with phospholipids in the plasma and intracellular organelle membranes, thereby interfering with the regulation of signalling pathways involved in the various components of the inflammatory response.28,29 Among their numerous effects, macrolides have been reported to inhibit the release of pro‐inflammatory mediators, to limit the pulmonary influx of neutrophils, to regulate mucus secretion, and to alter the formation of the biofilm matrix. In CF, there is currently no direct demonstration of the anti‐inflammatory action of macrolides.30 Saiman and colleagues found that sputum neutrophil elastase activity increased in the placebo group over 6 months but remained the same in the azithromycin group.10 By contrast, Equi and colleagues could not document any changes in airway interleukin (IL)‐8 and neutrophil elastase concentrations in the subgroup of patients who produced sputum.20 This discrepancy can be explained by the difficulty in obtaining reliable measurements of inflammatory mediators in the sputum of CF patients. Information obtained in other chronic inflammatory pulmonary conditions is therefore of interest. In diffuse panbronchiolitis, decreased levels of IL‐8 were reported in the bronchoalveolar lavage fluids of patients treated with macrolides.31 Improvement in clinical symptoms of corticosteroid dependent patients with asthma and a reduction in corticosteroid dosage with concomitant macrolide therapy have also been reported in several studies.7
In conclusion, the results of this randomised controlled trial show the beneficial effect of long term use of low dose azithromycin in young patients with CF, even in the absence of infection with P aeruginosa. This benefit was associated with a significant reduction in the occurrence of pulmonary exacerbations requiring additional courses of antibiotics, and may be seen in the absence of changes in lung function. The lower incidence of acute exacerbations in patients receiving azithromycin is an important and clinically relevant measure of beneficial effect. Long term use of azithromycin with sub‐antimicrobial doses may therefore be considered as a therapeutic strategy to slow pulmonary deterioration in CF, possibly through reduction of the inflammatory burden of the disease, although this remains to be better investigated. Additional trials will be needed to evaluate further the efficacy and safety of prolonged use (>1 year) of macrolide antibiotics in children. These trials should be monitored by both relevant clinical and functional parameters.
Acknowledgements
The authors thank Frank Accurso for helpful comments and discussion, and acknowledge all the study participants.
Abbreviations
CF - cystic fibrosis
FEV1 - forced expiratory volume in 1 second
FVC - forced vital capacity
Footnotes
This study was supported by the Cystic Fibrosis Association Vaincre la Mucoviscidose, Paris, France.
Competing interests: none declared.
Investigators at clinical sites: M Roussey (Pediatric Department, Hôpital Sud, Rennes); J Navarro, A Munck, (Pediatric Department, Hôpital Robert Debré, Paris); I Pin (Pediatric Separtment, Hôpital de la Tronche, Grenoble); G Rault, V Storni (Pediatric Department, Centre de Perharidy, Roscoff); D Turck, D Wizla‐Derambure (Pediatric Department, Hôpital Jeanne de Flandre, Lille); F Brémont (Pediatric Department, CHU Purpan, Toulouse); M Michaël Fayon (Pediatric Department, CHU Groupe Pellerin, Hôpital des Enfants, Bordeaux); P Gautry (Pediatric Department, CHG de Brive, Brive); L Delumley, J Languepin (Pediatric Department, CHU Dupuytren, Limoges); B Delaisi (Pediatric Pulmonology Center, Boulogne); V David (Pediatric Department, Hôpital Mère‐Enfant, Nantes); A Sardet (Pediatric Department, Centre Hospitalier de Lens, Lens); C Marguet (Pediatric Department, CHU ‐ Hôpital Charles Nicolle, Rouen); J C Dubus, L Mely (Pediatric Department, Hôpital d'Enfants de la Timone, Marseille); G A Loeuille (Pediatric Department, CHG de Dunkerque, Dunkerque); M Scalbert (Pediatric Department, Hôpital Saint‐Antoine, Lille); P Blanchard (Pediatric Department, CHD Les Oudairies, La Roche sur Yon).
Data safety monitoring board: I Pin, Pediatric Deparment, University of Grenoble, Grenoble; D Turck, Pediatric Deparment, University of Lille, Lille.
Steering Committee: G Pons, Pharmacology Department, Hôpital St Vincent de Paul, Paris; E Jacqcz‐Aigrain, Pharmacology Department, Hôpital R Debré, Paris; T Chinet, Pulmonology Deparment, Hôpital Ambroise Paré, Boulogne; I Durieu, Pulmonology Department, Hôpital Lyon Sud, Lyon.
References
- 1.Wine J. The genesis of cystic fibrosis lung disease. J Clin Invest 1999103309–312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bush A, Accurso F, MacNee W.et al Cystic fibrosis, pediatrics, control of breathing, pulmonary physiology and anatomy, and surfactant biology in AJRCCM in 2004. Am J Respir Crit Care Med 2005171545–553. [DOI] [PubMed] [Google Scholar]
- 3.Sagel S D, Kapsner R, Osberg I.et al Airway inflammation in children with cystic fibrosis and healthy children assessed by sputum induction. Am J Respir Crit Care Med 20011641425–1431. [DOI] [PubMed] [Google Scholar]
- 4.Sagel S D, Accurso F J. Monitoring inflammation in CF. Cytokines. Clin Rev Allergy Immunol 20022341–57. [DOI] [PubMed] [Google Scholar]
- 5.Ratjen F, Doring G. Cystic fibrosis. Lancet 2003361681–689. [DOI] [PubMed] [Google Scholar]
- 6.Robinson P. Cystic fibrosis. Thorax 200156237–241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hatipoglu U, Rubinstein I. Low‐dose, long‐term macrolide therapy in asthma: an overview. Clin Mol Allergy 200424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jaffe A, Bush A. Anti‐inflammatory effects of macrolides in lung disease. Pediatr Pulmonol 200131464–473. [DOI] [PubMed] [Google Scholar]
- 9.Southern K W, Barker P M. Azithromycin for cystic fibrosis. Eur Respir J 200424834–838. [DOI] [PubMed] [Google Scholar]
- 10.Saiman L, Marshall B C, Mayer‐Hamblett N.et al Azithromycin in patients with cystic fibrosis chronically infected with Pseudomonas aeruginosa. A randomized controlled trial. JAMA 20032901749–1756. [DOI] [PubMed] [Google Scholar]
- 11.Pierre‐Audigier C, Ferroni A, Sermet‐Gaudelus I.et al Age‐related prevalence and distribution of nontuberculous mycobacterial species among patients with cystic fibrosis. J Clin Microbiol 2005433467–3470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cystic Fibrosis Foundation Microbiology and infectious disease in cystic fibrosis. Volume V, Section 1. Bethesda, MD: Cystic Fibrosis Foundation, 19941–26.
- 13.Henry B, Aussage P, Grosskopf C.et al Development of the Cystic Fibrosis Questionnaire (CFQ) for assessing quality of life in pediatric and adult patients. Qual Life Res 20031263–76. [DOI] [PubMed] [Google Scholar]
- 14.Knudson R J, Lebowitz M D, Holberg C J.et al Changes in the normal maximal expiratory flow‐volume curve with growth and aging. Am Rev Respir Dis 1983127725–734. [DOI] [PubMed] [Google Scholar]
- 15.Rolland‐Cachera M, Cole T, Sempe M.et al Body mass index variations: centiles from birth to 87 years. Eur J Clin Nutr 19914513–21. [PubMed] [Google Scholar]
- 16.Diggle P J, Heagerly P, Liang K Y.et alAnalysis of longitudinal data. 2nd ed. Oxford: University Press, 2002
- 17.Edwards L. Modern statistical techniques for the analysis of longitudinal data in biomedical research. Pediatr Pulmonol 200030330–344. [DOI] [PubMed] [Google Scholar]
- 18.Jaffe A, Francis J, Rosenthal M.et al Long‐term azithromycin may improve lung function in children with cystic fibrosis. Lancet 1998351420. [DOI] [PubMed] [Google Scholar]
- 19.Wolter J, Seeney S, Bell S.et al Effect of long term treatment with azithromycin on disease parameters in cystic fibrosis: a randomised trial. Thorax 200257212–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Equi A, Balfour‐Lynn I M, Bush A.et al Long term azithromycin in children with cystic fibrosis: a randomised, placebo‐controlled crossover trial. Lancet 2002360978–984. [DOI] [PubMed] [Google Scholar]
- 21.Davis P B, Byard P J, Konstan M W. Identifying treatments that halt progression of pulmonary disease in cystic fibrosis. Pediatr Res 199741161–165. [DOI] [PubMed] [Google Scholar]
- 22.Corey M, Edwards L, Levison H.et al Longitudinal analysis of pulmonary function decline in patients with cystic fibrosis. J Pediatr 1997131809–814. [DOI] [PubMed] [Google Scholar]
- 23.Merkus P, Tiddens H, de Jongste J. Annual lung function changes in young patients with chronic lung disease. Eur Respir J 200219886–891. [DOI] [PubMed] [Google Scholar]
- 24.Marshall B. Pulmonary exacerbations in cystic fibrosis. Am J Respir Crit Care Med 2004169781–782. [DOI] [PubMed] [Google Scholar]
- 25.Wozniak D J, Keyser R. Effects of subinhibitory concentrations of macrolide antibiotics on Pseudomonas aeruginosa. Chest 200412562–9S. [DOI] [PubMed] [Google Scholar]
- 26.Ferkol T, Rosenfeld M, Milla C E. Cystic fibrosis pulmonary exacerbations. J Pediatr 2006148259–264. [DOI] [PubMed] [Google Scholar]
- 27.Garey K W, Alwani A, Danziger L H.et al Tissue reparative effects of macrolide antibiotics in chronic inflammatory sinopulmonary diseases. Chest 2003123261–265. [DOI] [PubMed] [Google Scholar]
- 28.Tsai W C, Rodriguez M L, Young K S.et al Azithromycin blocks neutrophil recruitment in Pseudomonas endobronchial infection. Am J Respir Crit Care Med 20041701331–1339. [DOI] [PubMed] [Google Scholar]
- 29.Amsden G W. Anti‐inflammatory effects of macrolides: an underappreciated benefit in the treatment of community‐acquired respiratory tract infections and chronic inflammatory pulmonary conditions? J Antimicrob Chemother 20055510–21. [DOI] [PubMed] [Google Scholar]
- 30.Ordonez C L, Stulbarg M, Grundland H.et al Effect of clarithromycin on airway obstruction and inflammatory markers in induced sputum in cystic fibrosis: a pilot study. Pediatr Pulmonol 20013229–37. [DOI] [PubMed] [Google Scholar]
- 31.Sakito O, Kadota J, Kohno S.et al Interleukin 1 beta, tumor necrosis factor alpha, and interleukin 8 in bronchoalveolar lavage fluid of patients with diffuse panbronchiolitis: a potential mechanism of macrolide therapy. Respiration 19966342–48. [DOI] [PubMed] [Google Scholar]