Abstract
Recurrence in the contralateral lung of patients who have undergone pneumonectomy for lung cancer is often not surgically treatable. Percutaneous radiofrequency ablation (RFA) of tumours is an emerging minimally invasive technique which has recently been used in the treatment of lung cancer. The case history is presented of a patient who had previously undergone pneumonectomy in whom recurrence of lung cancer was treated by RFA. The procedure was performed under CT guidance and was uneventful. At follow up 9 months later the tumour appeared to have ablated. To our knowledge, no similar case has previously been reported in the literature.
Keywords: lung cancer, pneumonectomy, radiofrequency ablation
Surgical resection of recurrent non‐small cell lung cancer (NSCLC) in the residual lung after pneumonectomy is not always possible and is characterised by a high rate of postoperative mortality.1,2,3 Percutaneous radiofrequency ablation (RFA), a relatively recent minimally invasive local treatment for primary and secondary lung cancers,4,5,6,7 was used in a patient with a single lung. To our knowledge, this has not previously been reported.
Case history
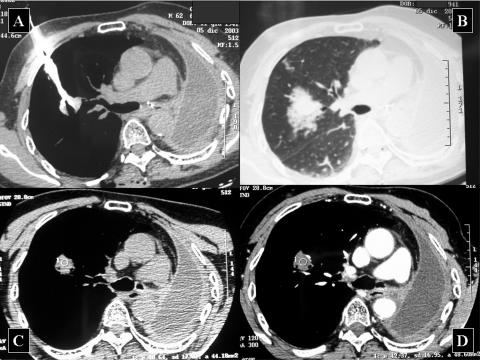
In January 2003 a 62 year old man underwent a left pneumonectomy for NSCLC. Pathological study revealed a satellite nodule in the left upper lobe and a metastatic hilar node assessed as stage IIIB (T4N1). No adjuvant treatment was given. At follow up 11 months later a CT scan of the chest showed a solitary pulmonary nodule, 25 mm in diameter, deep in the parenchyma of the right upper lobe of the residual right lung (fig 1). Bronchoscopy and complete staging did not reveal any other evidence of the disease. Histology of the lesion was not available. In accordance with the criteria of Martini and Melamed, the tumour was considered a second primary lung cancer.
Figure 1 CT scans showing (A) correct placement of the needle inside the tumour, (B) ground glass area of the thermal lesion surrounding the tumour just after the procedure, and (C, D) 1 month later the tumour seems to be slightly reduced in size with no contrast media enhancement.
The patient could have been considered a candidate for surgical resection but the location of the lesion would have involved removal of too much parenchyma (almost a lobectomy). Percutaneous RFA was therefore considered the best option for attempting local tumour eradication with minimum removal of parenchyma. The radiofrequency generator had a maximum power output of 150 W (Model 1500, RITA Medical System, Mountain View, CA, USA). The energy was transferred to the tumour by means of a 14 gauge needle with nine electrodes (StarBurst XL, RITA Medical System). Local anaesthesia and intravenous sedation were given. With the patient in the prone position, the needle was inserted by CT guidance as far as the periphery of the tumour. The electrodes were placed up to 3 cm and the tumour was heated at 90°C for 15 minutes (fig 1A, B). CT scans were performed both during the procedure and at the end and showed no complications. Chest radiographs were also performed after 12, 24, and 48 hours and showed no evidence of complications. The patient was discharged on the second postoperative day. Radiological follow up at 1, 3, 6, and 9 months revealed the presence of a thermal necrotic area at the ablation site without contrast media enhancement that progressively reduced in size, suggesting ablation of the lesion (fig 1C, D). Respiratory function tests at 3 and 6 months did not show any differences in pulmonary reserve compared with the values before RFA.
Discussion
The resection of recurrent tumours on the residual lung after pneumonectomy is unusual.1 These patients, with limited respiratory function, may not tolerate another resection of lung parenchyma. The postoperative mortality rate is high, particularly if pulmonary resection is extensive with removal of a large amount of parenchyma.2,3 Accurate patient selection, based on nodule number, location and diameter, is therefore necessary to avoid surgery in patients with multiple lung recurrences or a deep seated nodule.
A relatively new procedure that permits local treatment of lung tumours with minimal removal of lung parenchyma is RFA. This procedure, used when surgical resection is contraindicated, is under evaluation as a potential complementary therapy for patients with NSCLC. In our institute, after a preclinical study,8 we have been performing radiofrequency thermal ablation of lung tumours since 2001. We have to date used RFA to treat 59 lung tumours in 44 patients; in about half of these cases their clinical condition, particularly their respiratory function, was poorer than that of the patient described in this paper.7 Moreover, as reported in the literature and in our experience, the morbidity rate associated with this method is low.5,6,7 Pneumothorax is the most frequent complication, occurring in 13–53% of patients, with less than half requiring chest tube drainage.
The preliminary results of this technique in terms of local disease control were satisfactory. A radiologically determined response was achieved in eight of 12 patients (67%) with lesions up to 5 cm by Herrera et al,6 while we have achieved a positive response in 78% of patients with tumours less than 3.5 cm.7 These results suggest that this method could be the best option in selected cases with the aim of a curative treatment.
In conclusion, RFA may represent one of several potential treatment options in cases where surgery is not appropriate, even in patients with a single lung. Multidisciplinary cooperation between experienced practitioners is necessary to reduce the risks to an acceptable level.
Footnotes
Competing interests: the authors have no relevant financial interests in the products described that may influence their interpretation of the results.
References
- 1.Terzi A, Lonardoni A, Scanagatta P.et al Lung resection for bronchogenic carcinoma after pneumonectomy: a safe and worthwhile procedure. Eur J Cardiothorac Surg 20042456–459. [DOI] [PubMed] [Google Scholar]
- 2.Spaggiari L, Grunenwald D, Girard P.et al Cancer resection on the residual lung after pneumonectomy for bronchogenic carcinoma. Ann Thorac Surg 1996621598–1602. [DOI] [PubMed] [Google Scholar]
- 3.Donington J S, Miller D L, Rowland C C.et al Subsequent pulmonary resection for bronchogenic carcinoma after pneumonectomy. Ann Thorac Surg 200274154–159. [DOI] [PubMed] [Google Scholar]
- 4.Dupuy D E, Mayo‐Smith W W, Abbott G F.et al Clinical application of radiofrequency tumour ablation in thorax. Radiographics 200222(Special Issue)S259–S269. [DOI] [PubMed] [Google Scholar]
- 5.Steinke K, King J, Glenn D.et al Radiologic appearance and complications of percutaneous computed tomography‐guided radiofrequency‐ablated pulmonary metastases from colorectal carcinoma. J Comput Assist Tomogr 200327750–757. [DOI] [PubMed] [Google Scholar]
- 6.Herrera L J, Fernando H C, Perry Y.et al Radiofrequency ablation of pulmonary malignant tumors in non surgical candidates. J Thorac Cardiovasc Surg 2003125929–937. [DOI] [PubMed] [Google Scholar]
- 7.Mussi A, Ambrogi M C. Percutaneous thermal ablation of lung tumours (editorial). Ann Osp San Camillo Forlanini 20035225–227. [Google Scholar]
- 8.Ambrogi M C, Fontanini G, Lencioni R.et al A preliminary study on thermal ablation of lung tumour. Contemporary Oncol 20048373–379. [Google Scholar]