Abstract
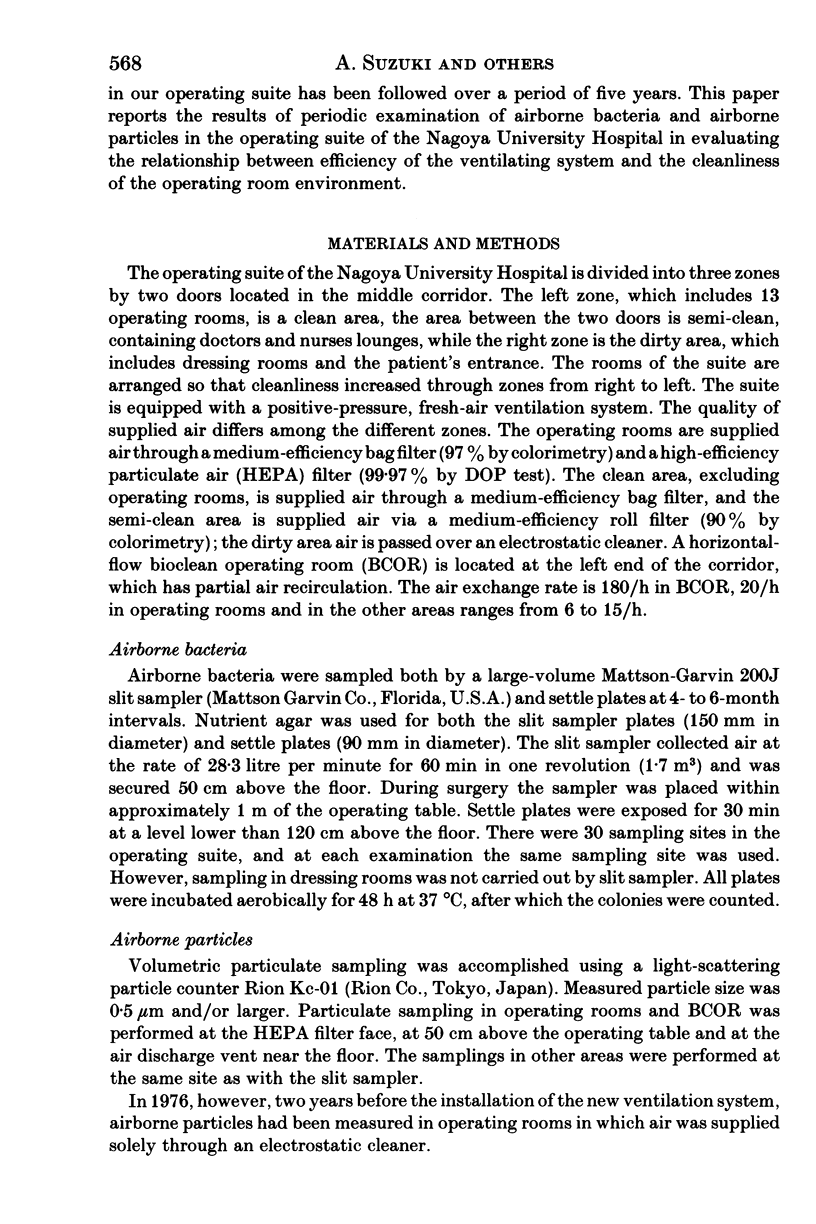
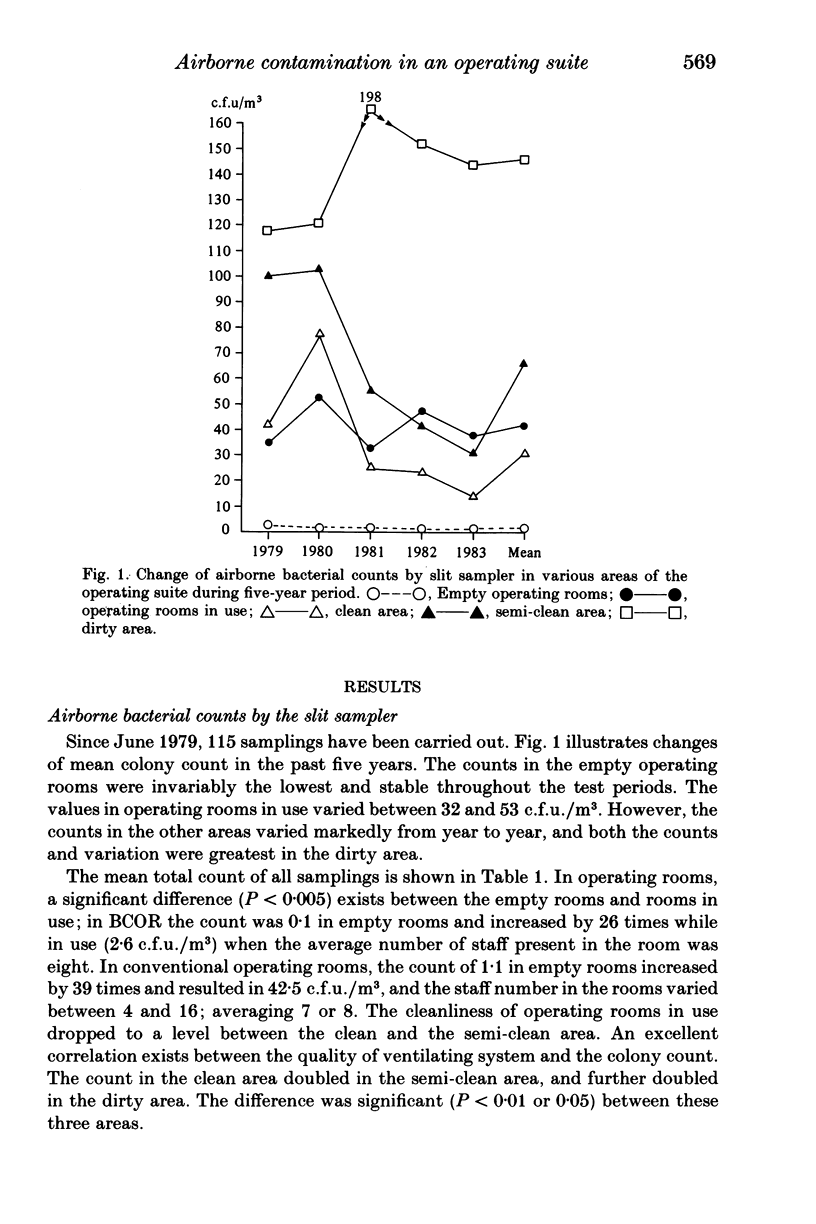
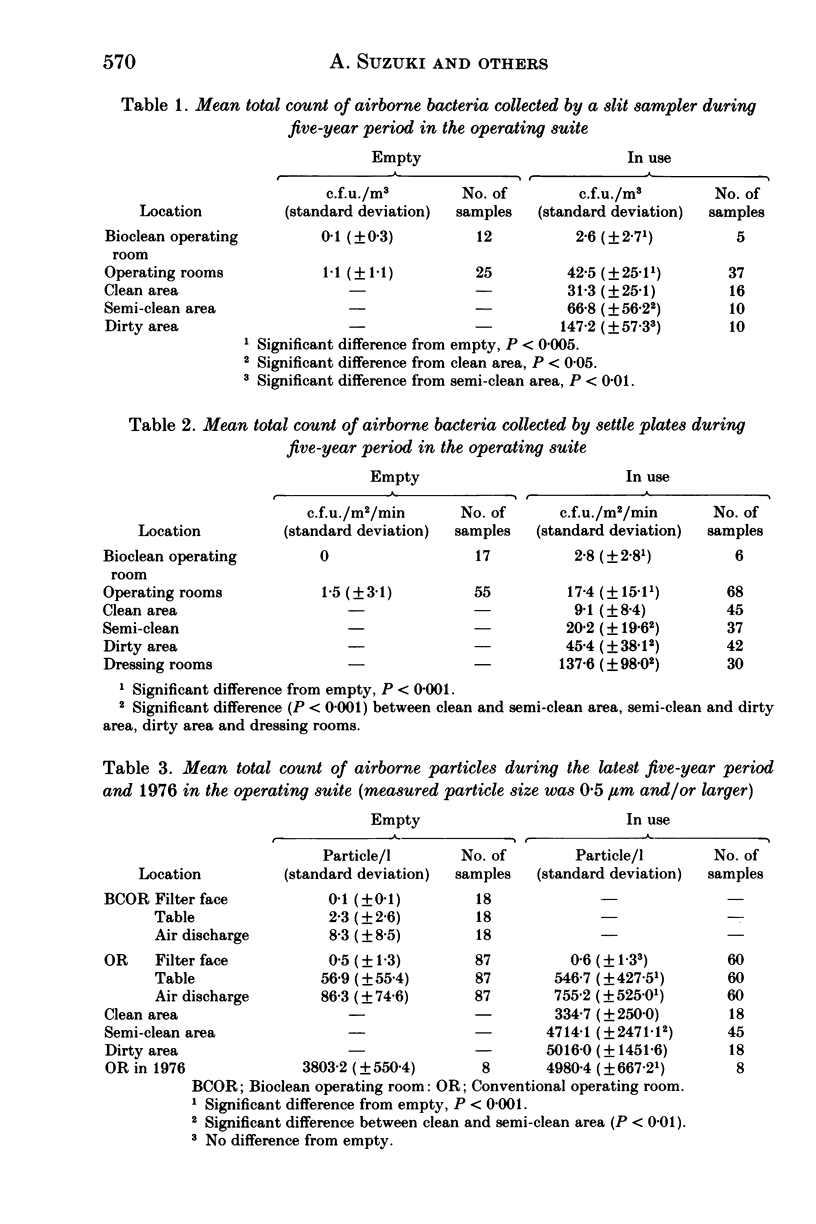
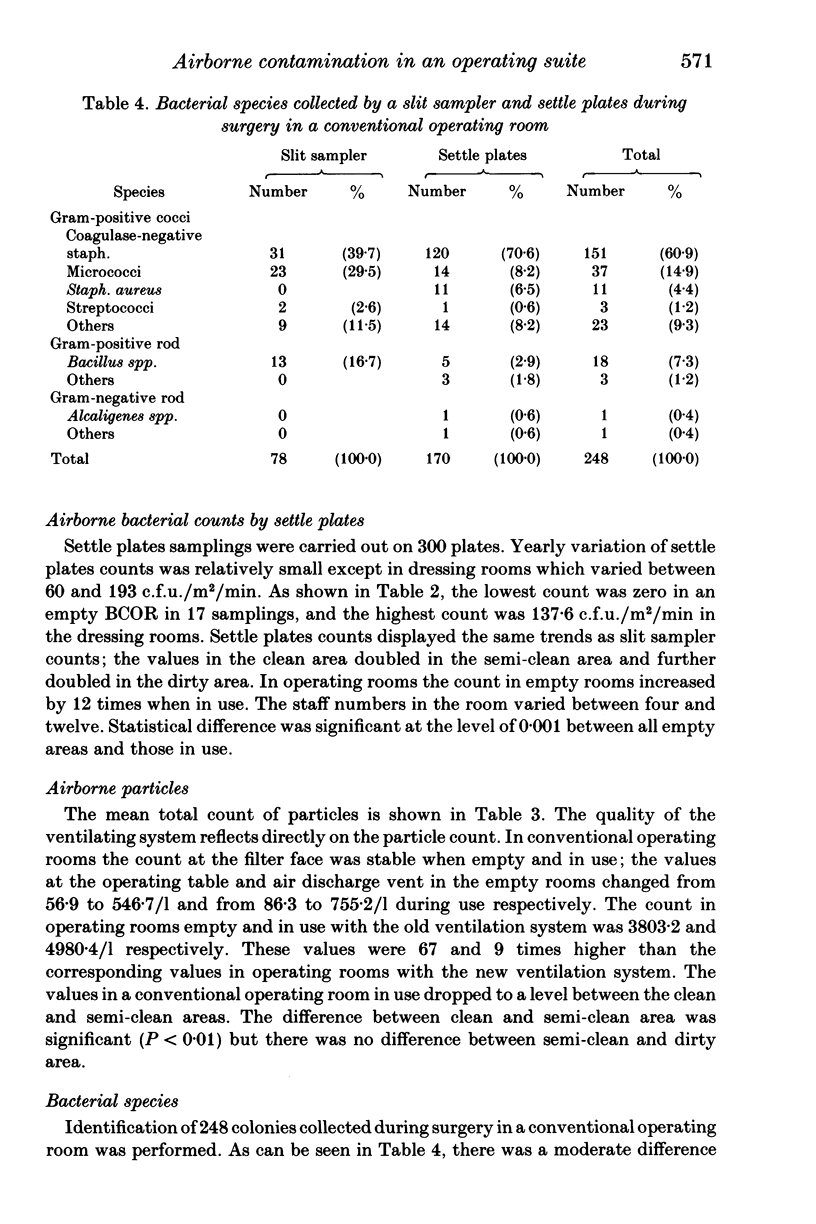
Airborne contamination in an operating suite was studied with a slit sampler, settle plates and a light-scattering particle counter. In conventional operating rooms there was a significant difference between the empty rooms and rooms in use; the mean total bacterial count by a slit sampler changed from 1.1 in empty to 42.5 c.f.u./m3 in use (39 times increase), the settle plates count changed from 1.5 to 17.4 c.f.u./m2/min (12 times increase), and the mean total particle count changed from 56.9 to 546.7/l (10 times increase) respectively. The increase was caused mainly by persons present in the room. Another difference was found between zones in the operating suite; the bacterial count in the clean area doubled in the semi-clean area and further doubled in the dirty area in slit sampler count as well as settle plates count, and particle count in the clean area increased by 14 times in the semi-clean and dirty areas. This difference resulted from the different quality of the ventilating system. Air cleanliness of operating rooms in use by persons present in the room dropped to a level between the clean and the semi-clean area in spite of the high quality of the ventilating system. Bacterial species identified were mostly coagulase negative staphylococci and micrococci. Our study indicates that reduction of airborne contamination in an operating suite is accomplished by the combination of an efficient ventilating system and the restriction of the number of persons present in the room.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Bengtsson S., Hambraeus A., Laurell G. Wound infections after surgery in a modern operating suite: clinical, bacteriological and epidemiological findings. J Hyg (Lond) 1979 Aug;83(1):41–57. doi: 10.1017/s002217240002581x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charnley J. Postoperative infection after total hip replacement with special reference to air contamination in the operating room. Clin Orthop Relat Res. 1972 Sep;87:167–187. doi: 10.1097/00003086-197209000-00020. [DOI] [PubMed] [Google Scholar]
- Fitzgerald R. H., Jr Microbiologic environment of the conventional operating room. Arch Surg. 1979 Jul;114(7):772–775. doi: 10.1001/archsurg.1979.01370310014003. [DOI] [PubMed] [Google Scholar]
- Lidwell O. M., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Airborne contamination of wounds in joint replacement operations: the relationship to sepsis rates. J Hosp Infect. 1983 Jun;4(2):111–131. doi: 10.1016/0195-6701(83)90041-5. [DOI] [PubMed] [Google Scholar]
- Lidwell O. M., Lowbury E. J., Whyte W., Blowers R., Stanley S. J., Lowe D. Effect of ultraclean air in operating rooms on deep sepsis in the joint after total hip or knee replacement: a randomised study. Br Med J (Clin Res Ed) 1982 Jul 3;285(6334):10–14. doi: 10.1136/bmj.285.6334.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- NOBLE W. C., LIDWELL O. M., KINGSTON D. THE SIZE DISTRIBUTION OF AIRBORNE PARTICLES CARRYING MICRO-ORGANISMS. J Hyg (Lond) 1963 Dec;61:385–391. doi: 10.1017/s0022172400020994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whyte W., Lidwell O. M., Lowbury E. J., Blowers R. Suggested bacteriological standards for air in ultraclean operating rooms. J Hosp Infect. 1983 Jun;4(2):133–139. doi: 10.1016/0195-6701(83)90042-7. [DOI] [PubMed] [Google Scholar]


