Abstract
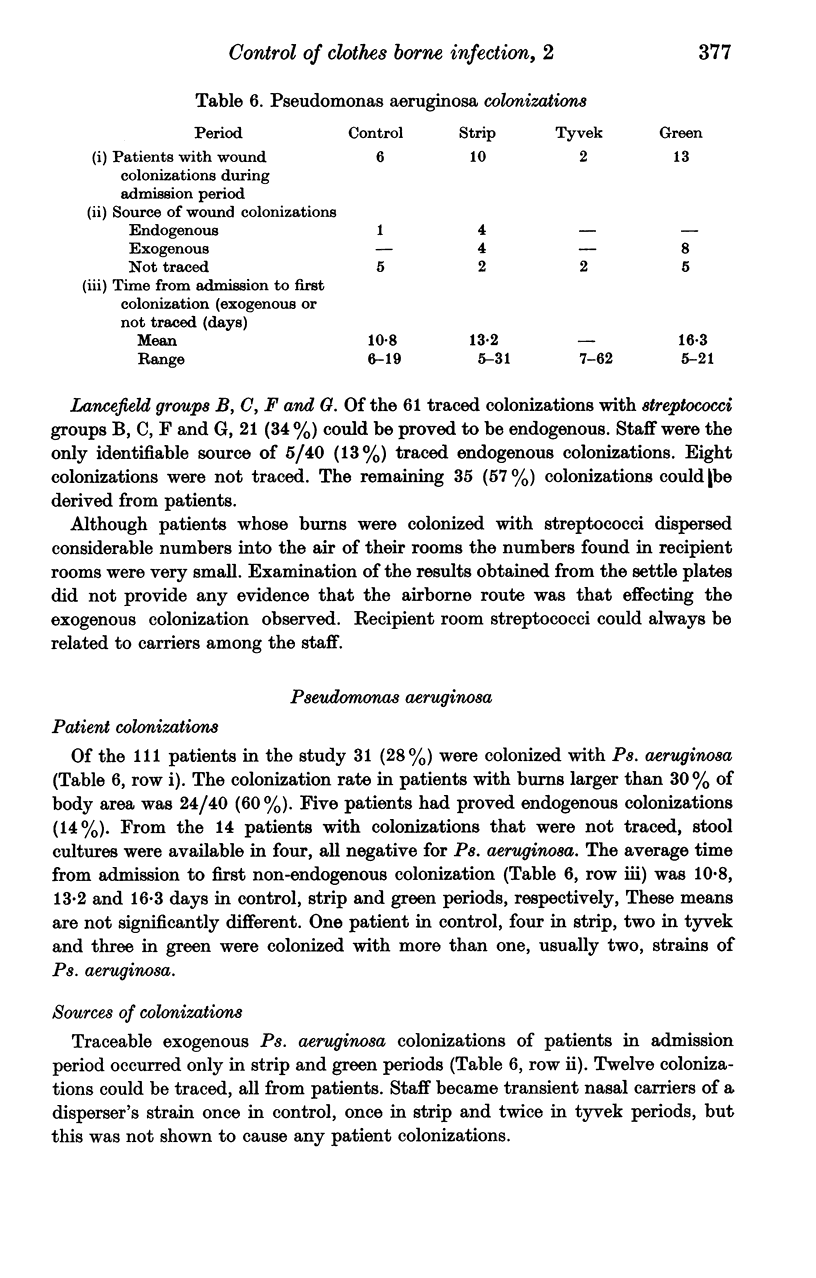
Previous investigations have shown that cross-contamination in a burn unit is mainly clothes-borne. New barrier garments have been designed and tried experimentally. The aim of the present study was to investigate the effects of different clothing routines on cross-contamination. In a long-term study, the rates and routes of colonizations with Staphylococcus aureus, Streptococcus groups A, B, C, F, and G and Pseudomonas aeruginosa were examined. The exogenous colonization rates were, with S. aureus 77%, with Streptococcus species 52% and with Ps. aeruginosa 32%. The colonization rate with Ps. aeruginosa was higher in patients with larger burns. Patients dispersed Streptococcus and Ps. aeruginosa as well as S. aureus into the air of their rooms in considerable amounts, but dispersers were not more important as sources of cross-colonization than non-dispersers. In comparison of clothing routines, there was no difference in overall colonization rates. The newly designed barrier garment that was made from apparently particle-tight material did not reduce the transfer of bacteria from patient to patient. A less rigid routine than that previously used did not increase the risk of cross-contamination. A thorough change of barrier dress after close contact nursing delayed the first exogenous S. aureus colonization from day 6 to day 14 after admission. This routine might be recommended for clinical use. Otherwise, methods must be developed for adequate selection of materials intended for barrier garments.
Full text
PDF
Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Alford D. J., Ritter M. A., French M. L., Hart J. B. The operating room gown as a barrier to bacterial shedding. Am J Surg. 1973 May;125(5):589–591. doi: 10.1016/0002-9610(73)90143-8. [DOI] [PubMed] [Google Scholar]
- Aly R., Maibach H. I., Shinefield H. R., Mandel A., Strauss W. G. Bacterial interference among strains of Staphylococcus aureus in man. J Infect Dis. 1974 Jun;129(6):720–724. doi: 10.1093/infdis/129.6.720. [DOI] [PubMed] [Google Scholar]
- BERNARD H. R., SPEERS R., Jr, O'GRADY F., SHOOTER R. A. REDUCTION OF DISSEMINATION OF SKIN BACTERIA BY MODIFICATION OF OPERATING-ROOM CLOTHING AND BY ULTRAVIOLET IRRADIATION. Lancet. 1965 Sep 4;2(7410):458–461. doi: 10.1016/s0140-6736(65)91421-2. [DOI] [PubMed] [Google Scholar]
- Barclay T. L., Dexter F. Infection and cross-infection in a new Burns Centre. Br J Surg. 1968 Mar;55(3):197–202. doi: 10.1002/bjs.1800550309. [DOI] [PubMed] [Google Scholar]
- Cars O., Forsum U., Hjelm E. New immunofluorescence method for the identification of group a, b, c, e, and g streptococci. Acta Pathol Microbiol Scand B. 1975 Apr;83(2):145–152. doi: 10.1111/j.1699-0463.1975.tb00085.x. [DOI] [PubMed] [Google Scholar]
- Cason J. S., Jackson D. M., Lowbury E. J., Ricketts C. R. Antiseptic and aseptic prophylaxis for burns: use of silver nitrate and of isolators. Br Med J. 1966 Nov 26;2(5525):1288–1294. doi: 10.1136/bmj.2.5525.1288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans H. E., Akpata S. O., Baki A., Behrman R. E. Bacteriologic and clinical evaluation of gowning in a premature nursery. J Pediatr. 1971 May;78(5):883–886. doi: 10.1016/s0022-3476(71)80370-0. [DOI] [PubMed] [Google Scholar]
- Hambraeus A., Ransjö U. Attempts to control clothes-borne infection in a burn unit. I. Experimental investigations of some clothes for barrier nursing. J Hyg (Lond) 1977 Oct;79(2):193–202. doi: 10.1017/s0022172400052992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hambraeus A. Studies on transmission of Staphylococcus aureus in an isolated ward for burned patients. J Hyg (Lond) 1973 Mar;71(1):171–183. doi: 10.1017/s0022172400046349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes W. H. The irreducible minimum in cross-infection control and isolation nursing. J Hyg (Lond) 1970 Sep;68(3):379–392. doi: 10.1017/s0022172400042285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kominos S. D., Copeland C. E., Grosiak B. Mode of transmission of Pseudomonas aeruginosa in a burn unit and an intensive care unit in a general hospital. Appl Microbiol. 1972 Feb;23(2):309–312. doi: 10.1128/am.23.2.309-312.1972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- LIDWELL O. M., NOBLE W. C., DOLPHIN G. W. The use of radiation to estimate the numbers of micro-organisms in airborne particles. J Hyg (Lond) 1959 Sep;57:299–308. doi: 10.1017/s0022172400020167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lidwell O. M., Brock B., Shooter R. A., Cooke E. M., Thomas G. E. Airborne infection in a fully air-conditioned hospital. IV. Airborne dispersal of Staphylococcus aureus and its nasal acquisition by patients. J Hyg (Lond) 1975 Dec;75(3):445–474. doi: 10.1017/s0022172400024505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liljedahl S. O., Malmborg A. S., Nyström B., Sjöberg L. Spread of Pseudomonas aeruginosa in a burns unit. J Med Microbiol. 1972 Nov;5(4):473–481. doi: 10.1099/00222615-5-4-473. [DOI] [PubMed] [Google Scholar]
- Lowbury E. J., Babb J. R., Ford P. M. Protective isolation in a burns unit: the use of plastic isolators and air curtains. J Hyg (Lond) 1971 Dec;69(4):529–546. doi: 10.1017/s002217240002180x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacMillar B. G., Edmonds P., Hummel R. P., Maley M. P. Epidemilogy of Pseudomonas in a burn intensive care unit. J Trauma. 1973 Jul;13(7):627–638. doi: 10.1097/00005373-197307000-00007. [DOI] [PubMed] [Google Scholar]
- PERRY W. D., SIEGEL A. C., RAMMELKAMP C. H., Jr Transmission of group A streptococci. II. The role of contaminated dust. Am J Hyg. 1957 Jul;66(1):96–101. doi: 10.1093/oxfordjournals.aje.a119889. [DOI] [PubMed] [Google Scholar]
- Poplack D. G., Penland W. Z., Levine A. S. Bacteriological isolation garment. Lancet. 1974 Jun 22;1(7869):1261–1262. doi: 10.1016/s0140-6736(74)90012-9. [DOI] [PubMed] [Google Scholar]
- RUBBO S. D., SAUNDERS J. LIBERATION OF ORGANISMS FROM CONTAMINATED TEXTILES. J Hyg (Lond) 1963 Dec;61:507–513. doi: 10.1017/s0022172400021136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- RUBBO S. D., SAUNDERS J. LIBERATION OF ORGANISMS FROM CONTAMINATED TEXTILES. J Hyg (Lond) 1963 Dec;61:507–513. doi: 10.1017/s0022172400021136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whyte W., Vesley D., Hodgson R. Bacterial dispersion in relation to operating room clothing. J Hyg (Lond) 1976 Jun;76(3):367–378. doi: 10.1017/s0022172400055297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wormald P. J. The effect of a changed environment on bacterial colonization rates in an established burns centre. J Hyg (Lond) 1970 Dec;68(4):633–645. doi: 10.1017/s0022172400042571. [DOI] [PMC free article] [PubMed] [Google Scholar]