Abstract
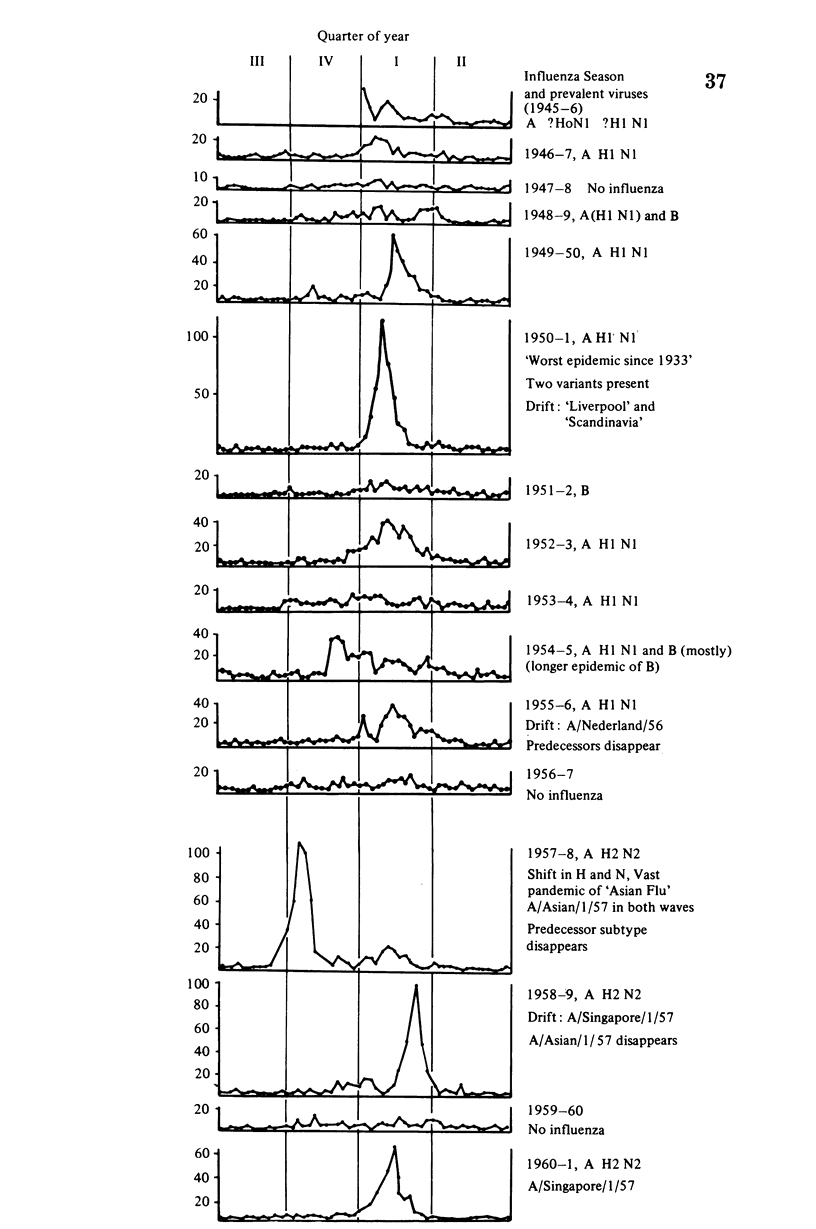
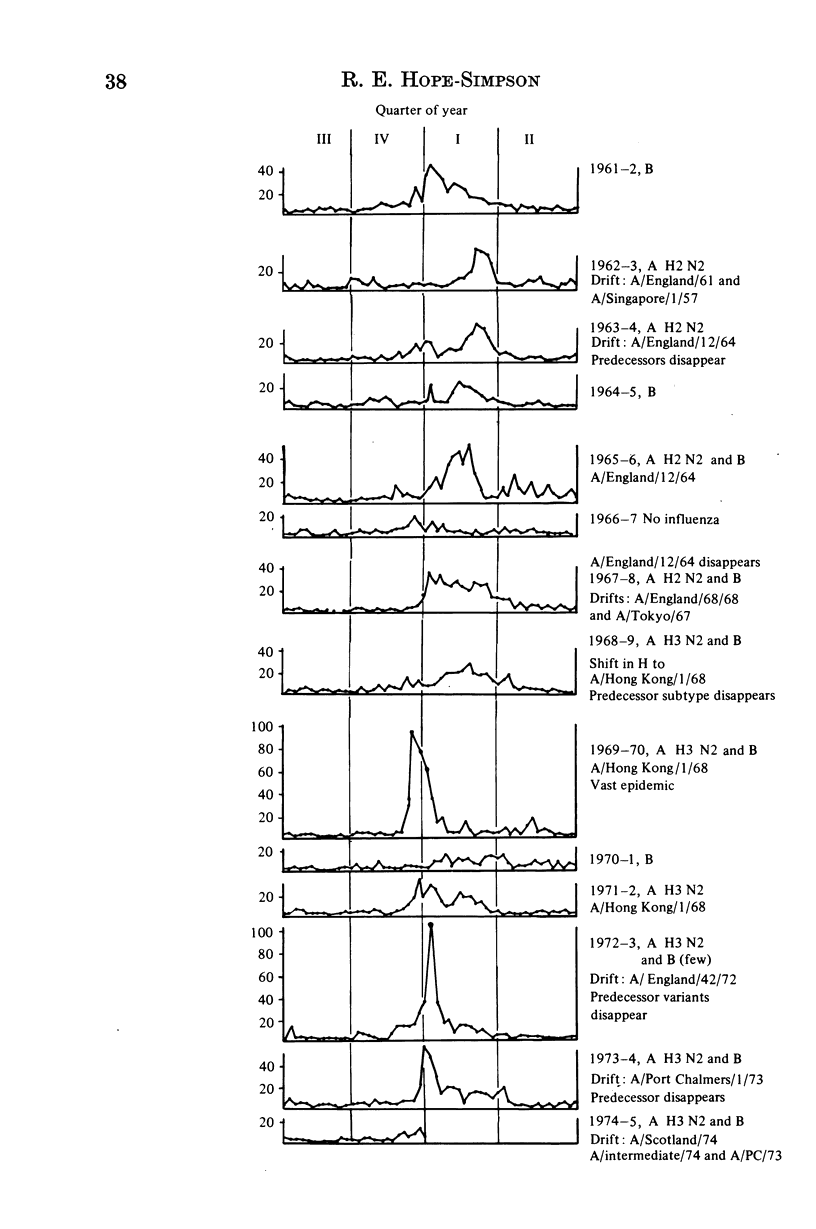
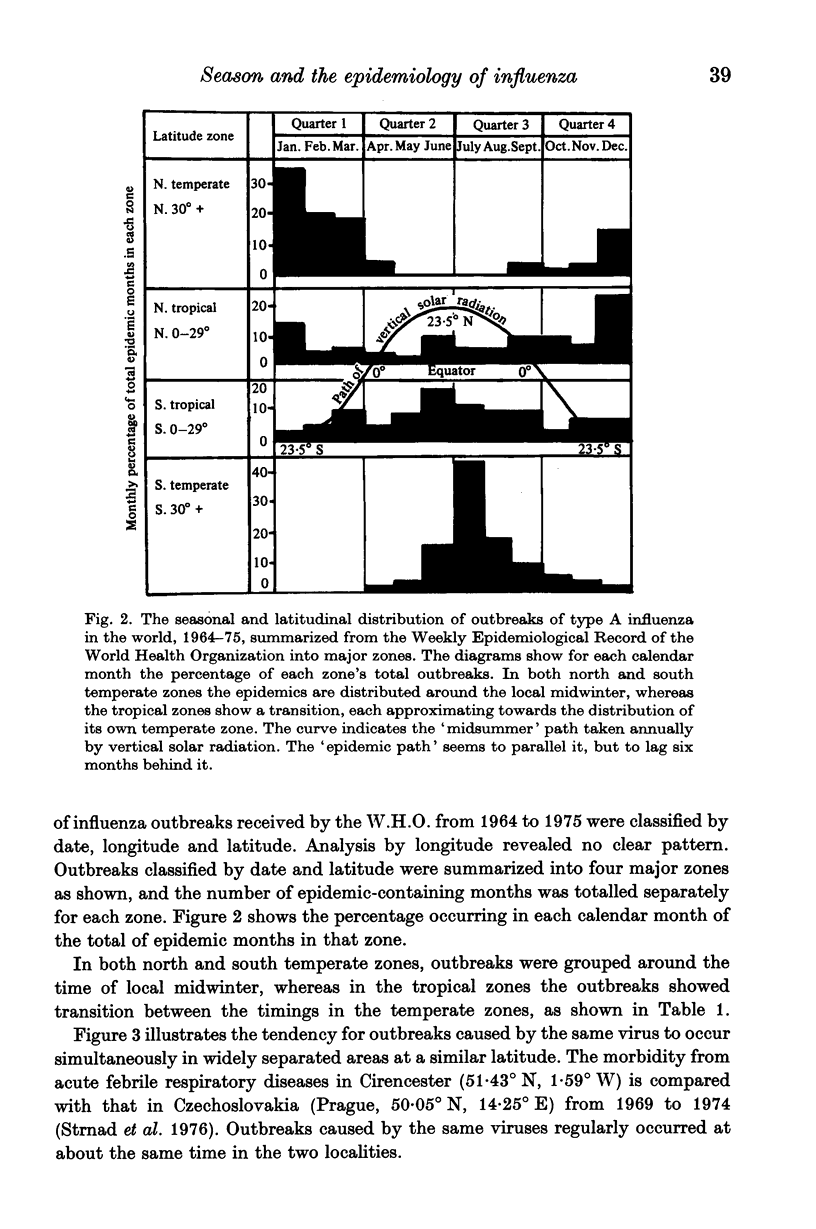
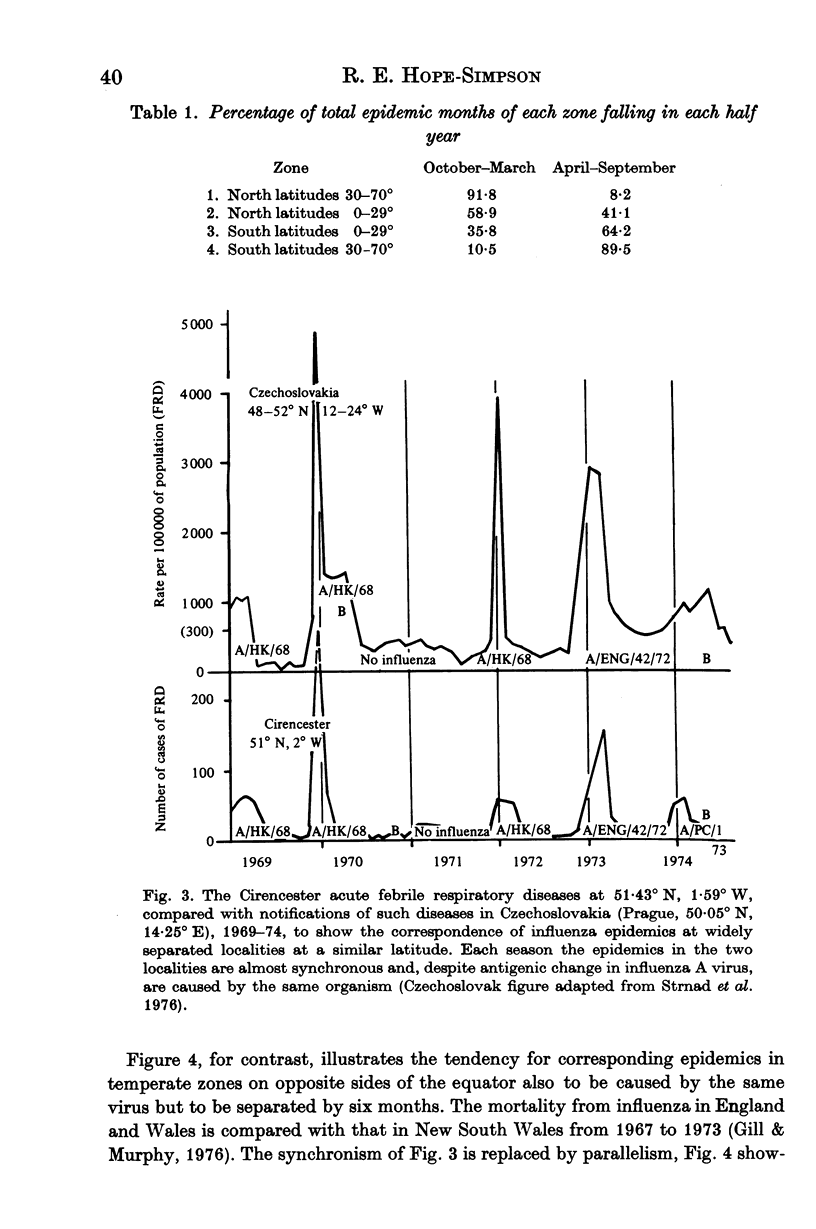
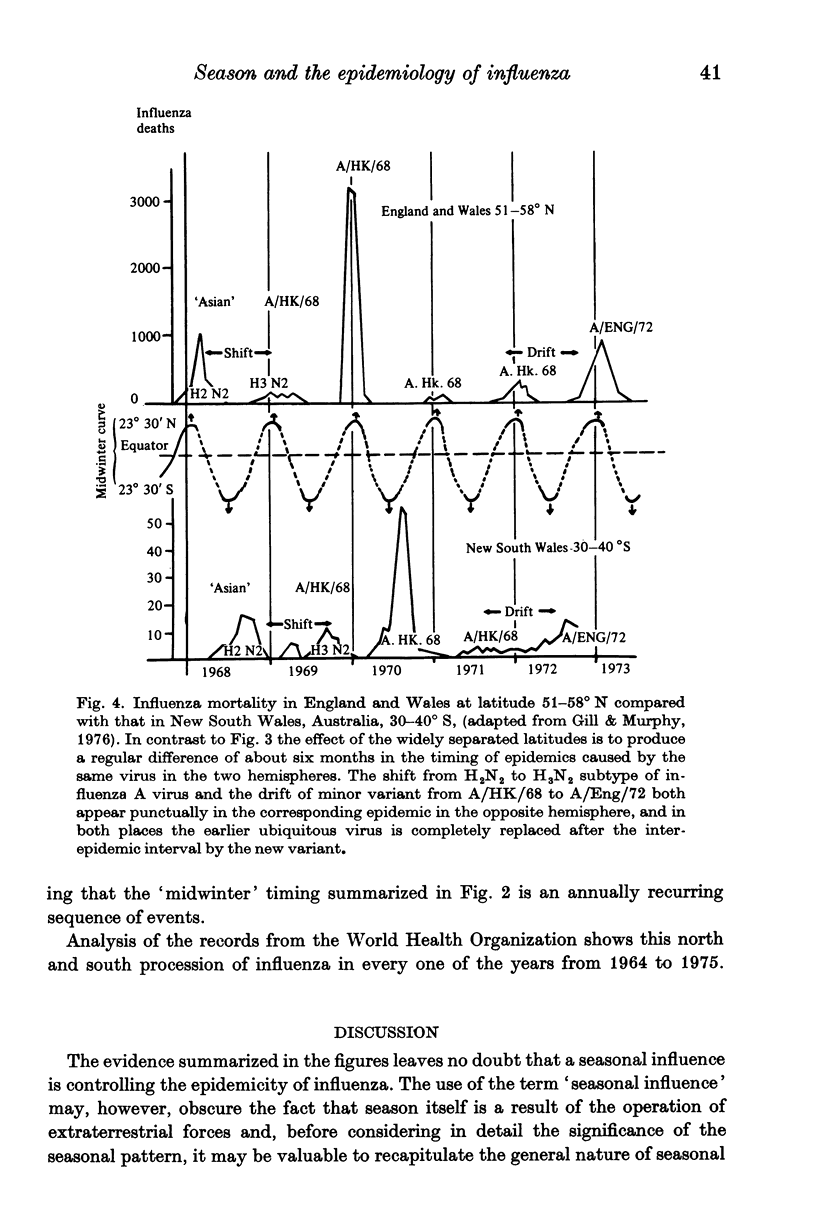
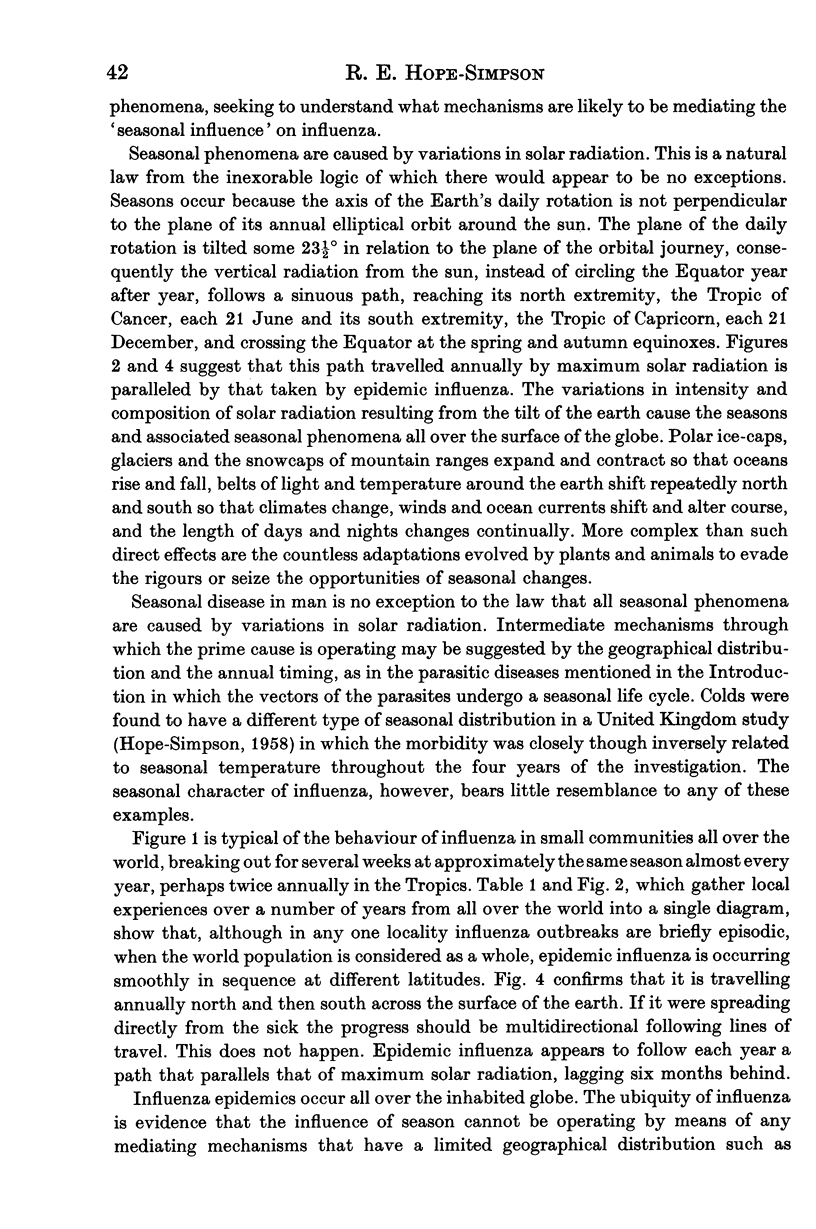
Four types of observations have been used to illustrate the seasonal characteristics of epidemic influenza: (1) The experience of a small population during 28 consecutive years, 1946-74, (2) world influenza outbreaks 1964-75 reported to the World Health Organization, (3) the experience of two widely separated localities at about the same latitude, 1969-74, and (4) the experience of two places at latitudes 30 degrees + on opposite sides of the Equator, 1968-74. The following tendencies are shown. (1) Outbreaks of influenza even in the small community came at approximately the same season almost every year. (2) Outbreaks are globally ubiquitous and epidemic loci move smoothly to and fro across the surface of the earth almost every year in a sinuous curve that runs parallel with the 'midsummer' curve of vertical solar radiation, but lags about six months behind it. Such findings exclude the mediation of seasonal control by any agencies of local distribution, and suggest a direct effect of variations in some component of solar radiation on virus or human host. (3) Antigenic variations in influenza A virus tended to have the same seasonal characteristics as epidemicity. This suggests that epidemicity and virus variation are two facets of one seasonally controlled process. None of these seasonal characteristics can be explained by the current concept of influenzal epidemiology. A new hypothesis recently proposed and recapitulated in the Appendix offers a possible explanation. The primary agency mediating seasonal control remains unidentified.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ARCHETTI I., HORSFALL F. L., Jr Persistent antigenic variation of influenza A viruses after incomplete neutralization in ovo with heterologous immune serum. J Exp Med. 1950 Nov 1;92(5):441–462. doi: 10.1084/jem.92.5.441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill P. W., Murphy A. M. Naturally acquired immunity to influenza type A: a clinical and laboratory study. Med J Aust. 1976 Aug 28;2(9):329–333. doi: 10.5694/j.1326-5377.1976.tb130219.x. [DOI] [PubMed] [Google Scholar]
- Hope-Simpson R. E. Epidemic mechanisms of type A influenza. J Hyg (Lond) 1979 Aug;83(1):11–26. doi: 10.1017/s002217240002578x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SIMPSON R. E. H. Common upper respiratory diseases. R Soc Health J. 1958 Sep-Oct;78(5):593–599. doi: 10.1177/146642405807800521. [DOI] [PubMed] [Google Scholar]
- Shadrin A. S., Marinich I. G., Taros L. Y. Experimental and epidemiological estimation of seasonal and climato-geographical features of non-specific resistance of the organism to influenza. J Hyg Epidemiol Microbiol Immunol. 1977;21(2):155–161. [PubMed] [Google Scholar]
- Strnad P., Tŭmová B., Syrŭcek L., Fedová D., Brůcková M., Kunzová L., Stumpa A., Strízová V., Berkovicová V., Losová M. Influenza and other actue respiratory diseases in the Czech Socialist Republic, 1969-1974. Bull World Health Organ. 1976;54(6):657–662. [PMC free article] [PubMed] [Google Scholar]


