Abstract
Francisella tularensis (F. tularensis) has been designated by the CDC as one of the ten organisms most likely to be engineered for bioterrorism. Symptoms of tularemia in humans are non-specific, thus making the disease difficult to diagnose. If not quickly diagnosed and treated, the disease has a high mortality rate - thus methods for early and specific diagnosis are of critical importance.
This immunoaffinity MALDI MS/MS (iMALDI) assay provides unambiguous detection of F. tularensis peptides at attomole levels from peptide solutions, and at low CFU levels from bacteria. The addition of stable-labeled versions of the peptide as internal standards allows absolute quantitation of F. tularensis peptides with a linear dynamic range spanning two orders of magnitude. The ability of mass spectrometry to obtain amino acid sequence data on affinity-captured peptides provides absolute specificity and avoids “false positives” from the non-specific binding. The F. tularensis iMALDI assay has been applied to different samples, such as nasal swabs.
This novel quantitative diagnostic F. tularensis iMALDI assay allows the safe, sensitive and specific detection of F. tularensis. The assay can be easily adapted to other target peptides and therefore has broad application potential in clinical diagnosis of other pathogens and diseases.
Keywords: Francisella tularensis, immuno Tandem Mass Spectrometry, MALDI, quantitation, iMALDI
1. Introduction
Tularemia is caused by Francisella tularensis (F. tularensis), a small, nonmotile, aerobic Gram-negative cocco-bacillus. Although normally causing a relatively rare tick-borne disease in humans, F. tularensis has the potential to be engineered for bioterrorism. The bacteria can penetrate unbroken skin, can survive and multiply within macrophages, and can then spread to various organs through the blood [1]. Ten bacteria injected subcutaneously [2], 10-50 on contact with unbroken skin [3], 10-50 given by aerosol [4, 5], or 102 to108 bacteria by ingestion [3] are sufficient to cause infection. Humans who have direct physical contact with infected animals or insects, or have inhaled aerosolized bacteria, have a good chance of becoming infected. Untreated, the mortality rate can be 30% [6].
Initial non-specific flu-like symptoms usually appear 3 days after exposure [7], and general laboratory tests (CRP, LDH, alkaline phosphatase, leukocytes, etc.) are insufficient for diagnosis. Because early antibiotic therapy (with streptomycin or gentamicin) can greatly reduce the lethality rate [8], an immediate diagnosis of an infection with F. tularensis is critical. Because of the virulence of F. tularensis, the severity of the disease, the rapidity of progression from initial onset to seriousness or death, and the high mortality rate, several agencies [9] have been concerned about the weaponization of F. tularensis, especially the use of aerosolized bacteria by terrorists as an airborne pathogen [10-12]. F. tularensis has been designated as one of the organisms most likely to be engineered for bioterrorism [13], and one of the six “category A bioterrorism organisms” [1, 11, 14, 15].
Bacteriological methods can be used for detecting F. tularensis [16], but culturing the organism is difficult [2, 4, 10, 17], time-consuming (sometimes taking several days), and is potentially hazardous to laboratory personnel [18]. Moreover, several studies have shown [19] that the sensitivities and specificities of these methods are low (note: “specificity” means that there are no “false positives” - i.e., the test gives a positive result only for the target organism).
Since culturing F. tularensis is difficult, serological tests such as the bacterial microagglutination (MA) test, have been used to diagnose tularemia, but this takes one week for measurable levels of antibodies to develop, and an additional week for sufficient antibody levels for a reliable test [10, 20-23]. Antibodies against F. tularensis may cross react with other organisms such as Brucella, Proteus OX19, and Yersinia spp. [10], which reduces the specificity and could lead to false positives. More recently, another type of serological test, an enzyme-linked immunosorbent assay (ELISA), achieved a detection limit of 103 bacteria mL-1 in PBS and 104 bacteria mL-1 in human serum [24]. However, when samples are contaminated with other microorganisms [25], accurate diagnosis with ELISA or culturing methods is very difficult due to their low specificities.
PCR is a molecular method for detection of F. tularensis that usually only takes several hours per reaction. A hand-held PCR assay could detect F. tularensis in 3 hours, and achieved the analytical sensitivity of 100 bacteria mL-1 PBS or 103 - 104 bacteria mL-1 serum [26]. However, PCR may give false positives from contamination with other DNA, which lowers its specificity. Moreover, simultaneous assaying for multiple species or virulence factors by PCR is difficult [27].
In this paper, we describe a peptide-based immunoaffinity MALDI mass spectrometry (iMALDI) assay for detection of F. tularensis, which circumvents many of the problems associated with traditional detection methods. It is based on capture of the F. tularensis IglC aa 49-61 peptide. This F. tularensis peptide assay is capable of fast, safe, sensitive, and specific detection of F. tularensis in PBS solution. It can be used for absolute quantitation of target peptides and, therefore, for absolute quantitation of their parent proteins. We also demonstrate the applicability of iMALDI to the detection of F. tularensi in clinical samples, such as human plasma and nasal swabs.
2. Experimental section
In iMALDI (Figure 1) [28] anti-peptide antibodies are first produced and immobilized on affinity beads. Next, the proteome of interest is proteolytically digested. Isotopically-labeled epitope-containing peptides, called “heavy” peptides, are added into the digest as internal standards for quantitation. The digest, containing both the labeled “heavy” peptides and the unlabeled native (“light”) peptides, is incubated with the antibody beads and both types of peptides are adsorbed. After immuno-adsorption, the antibody-beads are arranged in a microarray/spot format on the MALDI-target plate. MALDI matrix solution is then added, which enables the elution of the affinity-bound peptides from the immobilized antibodies permitting MALDI analysis of the peptides. The relative abundances of the molecular ion signals corresponding to the original “light” and “heavy” peptides are used for quantification. Absolute specificity can be achieved by mass spectrometric sequencing of the epitope-containing peptide, using MALDI-MS/MS.
Figure 1. Analytical scheme of the iMALDI assay.

Epitope-containing peptides, 49NIVAIEGGEDVTK61, synthesized using isotopically-labeled amino acid V, are added to the proteolytic digest of F. tularensis bacteria and are subsequently incubated with the anti-aa49-61 (F. tularensis IglC) antibody beads to immunoadsorb both isotopically-labeled and unlabelled peptides. After immunoadsorption of the differentially-labeled peptides, the antibody beads are arranged in a microarray/spot format on the MALDI-target plate. MALDI matrix solution added to the affinity-bound peptides elutes the peptides from the immobilized antibodies, permitting MALDI analysis of the peptides. The relative abundances of the molecular ion signals corresponding to heavy (isotopically-labeled) and light (unlabelled) peptides are used to quantify the amount of this protein in the original sample. Absolute specificity can be achieved by mass spectrometric sequencing of the epitope-containing peptide, using MALDI-MS/MS.
2.1. Target protein
The 23kDa protein, IglC, from F. tularensis bacteria is encoded by iglC, whose sequence has no significant homology to any other gene present in the GenBank database [29]. Live Vaccine Strain (LVS) bacteria, at a concentration of 2.25×109 CFU (Colony Forming Units) mL-1 in 70% ethanol, were used. The total protein concentration of the bacteria sample was 700ng mL-1 as determined with an ELX800 Universal Microplate Reader.
2.2. Nasal swab samples
Mice were inoculated intranasally with 1 × 105 LVS. Two days post inoculation, a small, moist, alginate swab was used to rub across the nostrils of the mice. The swab was then swirled in a tube containing 100 μL PBS. Next, 100 μL of 95% ethanol was added to the sample to ensure inactivation.
2.3. Tryptic digestion
Digestion of human plasma (UNC blood bank) was carried out in 25mM ammonium bicarbonate (Sigma) at 37°C overnight. A ∼1:10 enzyme:substrate ratio of trypsin (Sequencing-grade modified trypsin, Promega) to protein was used. The digested human plasma was spiked with F. tularensis peptides or a bacterial digest to mimic clinical samples. Before digestion, the nasal swab solution was diluted with ammonium bicarbonate until the final concentration of ethanol was 38%, which is compatible with tryptic digestion.
2.4. Antibody production and immobilization of antibodies on beads
Four F. tularensis IglC tryptic peptides, which are absolutely unique to, and thus diagnostic of F. tularensis, were selected for their high sensitivity in the MALDI-MS mode (Figure 2 and Table 1). These four peptides were synthesized by Sigma-Genosys. Antibodies were raised against each peptide, and tested by ELISA to determine the detection sensitivities/efficiencies. The peptide that showed the highest binding efficiency was selected for use in the Francisella peptide assay, and the corresponding antibody was purified by Sigma-Genosys.
Figure 2. Selection of F. tularensis IglC peptides for raising antibodies to be used for the F. tularensis iMALDI assay.
MALDI-MS of proteolytic F. tularensis IglC peptides obtained by in-solution digestion of IglC with trypsin. Four “true” (C-terminal cleavage of K or R residues) tryptic peptides of IglC (shown in blue) were selected for antibody production based on the high sensitivity in the MALDI-MS.
Table 1.
Affinity determination of the four anti-(F. tularensis IglC) peptide antibodies against their epitope peptide by ELISA. The cysteine residue marked with asterisk has been added to the native sequence because of ease of conjugation with the carrier protein
| Tryptic F.t. p23 peptides used antibody production | Anti-(F.t. p23) peptide Antibodies | ELISA response (titer) |
|---|---|---|
| 153AFSISIEPTELMGVS167 | [(F.t. p23) aa153-167] | 1/50,000 |
| 8QQVTSGETIHVR19 | [(F.t. p23) aa8-19] | 1/3,000 |
| 48C*NIVAIEGGEDVTK61 | [(F.t. p23) aa48-61] | 1/500,000 |
| 62ADSATAAASVIR73 | [(F.t. p23) aa62-73] | 1/10,000 |
The anti-peptide antibody was then immobilized on CNBr-activated sepharose beads (Amersham Pharmacia) according to the manufacturer’s instructions [30]. Briefly, by reacting with the primary amine groups on the antibody, the sepharose beads covalently linked to the antibody. Excess binding sites on the beads are blocked by incubation with an amine-containing buffer, (in this case, Tris). The process was completed by a series of washes at alternating pH.
2.5. Immuno-adsorption protocol
An aliquot of settled antibody-bead slurry (1-5 μL) was added to a compact reaction column (USB) and washed 4-5 times with 400 μL of 0.1× PBS. A bacterial digest or synthetic F. tularensis IglC peptide [CNIVAIEGGEDVTK, aa 49-61, calculated MW=1446.71 (note: the N-terminal cysteine, C, is not part of the native sequence, but was added to facilitate antibody production)] was dissolved in water/buffer and diluted to a series of concentrations, e.g. 25 ng μL-1, 5 ng μL-1, 0.5 ng μL-1, etc. A 20 μL aliquot of each solution was incubated separately with a small amount (1∼5 μL) of antibody-beads to immuno-adsorb the epitope-containing peptide. Peptide solutions or a bacterial digest spiked into a plasma digest mixture were used to mimic clinical samples. Three negative control experiments were performed by incubating (a) unconjugated agarose beads with PBS; (b) unconjugated agarose beads with synthetic peptide or bacteria digest sample; and (c) antibody-beads with PBS, respectively.
After incubation for 2-4 h at room temperature with end-to-end rotation on a “Labquake” rotator (Lab Industries), the beads were washed 6 times with 400 μL of freshly-made 50 mM ammonium bicarbonate. When high levels of non-specific binding were expected in complex samples such as plasma, the beads were washed 3 times with 400mM of NaCl (Sigma) followed by 3 times with 50 mM ammonium bicarbonate. Then the beads were re-suspended in a small volume of 50 mM ammonium bicarbonate (1-5 μL) and an aliquot of the beads (0.5 μL) was spotted directly onto the MALDI target as described in the Results and Discussion section.
2.6. Isotopic labeling for absolute quantitation
The F. tularensis IglC aa 49-61 peptide 49NIVAIEGGEDVTK61 (calculated MW=1343.69) containing an isotopically-labeled valine at position 59 (underlined) (the “heavy” peptide) was synthesized at the UNC Peptide Synthesis Facility, using a 13C-labeled fmoc Valine purchased from Isotec/Sigma-Aldrich according to the fmoc approach described in details elsewhere [31]. The increase in mass from the unlabeled (“light”) F. tularensis IglC aa 49-61 peptide was 6 Da.
2.7. Absolute quantitation
The “heavy” peptide, dissolved in water (HPLC grade, Pierce) was used as an internal standard. Heavy peptide was spiked into a F. tularensis bacterial digest in various amounts, immuno-adsorbed on anti-F. tularensis IglC peptide antibody beads, and analyzed by MALDI-MS of the beads on the MALDI target.
2.8. Mass spectrometric analysis
MALDI-MS experiments were performed on Bruker Daltonics’ (Billerica, MA) Reflex III and Ultraflex MALDI-TOFs, using Bruker’s Anchor-chip MALDI-target plates (400 or 600 μm/384 spot format). MS/MS analyses were carried out on an Applied Biosystems Voyager 4700 (Framingham, MA) MALDI-TOF/TOF. The matrix used for all experiments was recrystallized (from hot methanol) α-cyano-4-hydroxycinnamic acid (HCCA) (Sigma). A saturated solution of HCCA in 50:49.9:0.1 acetonitrile (Caledon Laboratories): water (HPLC grade, Pierce): trifluoroacetic acid (Pierce) was used. A small volume (1-5 μL) of ammonium bicarbonate (ABC) solution (50mM) was added for easy placement of the beads on the MALDI target. Following placement of the antibody beads on the target, 0.3-0.5 μL of HCCA matrix was added, and the spot was allowed to dry at room temperature.
3. Results and discussion
The iMALDI technique belongs to a general category of techniques which couples affinity capture with direct mass spectrometric analysis of target proteins (Experimental section and Figure 1) [32-49]. In iMALDI, anti-peptide antibodies are immobilized on sepharose beads for affinity capture, rather than on the surface of a plate, thus eliminating the need for special surface chemistry. Additional advantages of using affinity beads are less-stringent sample storage requirements after antibody immobilization, fewer complications resulting from denaturation of the capture antibody in solution, and the ability to incubate several types of beads with small volumes of tryptic-digested biological fluid instead of “soaking” the entire target. Because peptides are more stable and less susceptible to denaturation, the iMALDI should be more reproducible from sample to sample than the techniques based on anti-protein antibodies, and sample storage requirement should not be as stringent.
Unlike conventional affinity capture/elution/MALDI techniques [33, 34], the “stable isotope standards with capture by anti-peptide antibodies” (SISCAPA) approach [35], or on-target elution followed by removal of affinity beads as was done by Li [50], in iMALDI the affinity beads are placed directly on the MALDI target and analyzed without prior elution of the bound analytes [32-49], which greatly reduces the sample loss and therefore increases the detection sensitivity. In iMALDI, after immuno-adsorption, the antibody beads are arranged in a microarray/spot format on the MALDI-target plate. Addition of MALDI matrix solution releases the affinity-bound peptides from the immobilized antibodies permitting MALDI-analysis of the peptides. Multiple samples can be analyzed simultaneously by mass spectrometry as an array of different anti-peptide antibody beads on a MALDI target. Furthermore, since complete inactivation of the bacteria can be achieved by enzymatically digesting the lysate at the time of sample collection, the iMALDI technique carries low risk to laboratory personnel.
3.1. Sensitivity
3.1.1. Detection of F. tularensis bacteria in PBS solution
By direct MALDI-MS analysis of the beads, the detection limit for the synthetic F. tularensis IglC peptide (cysteine was added for antibody production) was determined to be in the low attomole range (14 attomoles) in buffer (HPLC-grade water or PBS). Without enrichment by iMALDI, in MALDI-MS analysis, the detection sensitivity of the peptide in buffer was in the low femtomole range (17 femtomoles) (Figure 3). In the enrichment process, the peptides are bound to antibody beads, which greatly reduces losses due to adsorption by tubes and tips. Moreover, when spotted on the target plate, even after elution by the matrix solution, the peptides do not spread out all over the spot area. Instead, they tend to aggregate at “hot spots”, and when the laser is focused at these “hot spots”, greatly increased detection sensitivities can be obtained.
Figure 3. Detection sensitivity of synthetic F. tularensis IglC peptides in solution and using the F. tularensis iMALDI assay.
MALDI-MS spectrum of synthetic F. tularensis IglC peptide CNIVAIEGGEDVTK a) in solution: a-1) 100 femtomoles; a-2) 1 femtomoles; a-3) 10 attomoles. b) affinity-bound to anti-aa 48-61 (F. tularensis IglC) antibody beads: b-1) 138 femtomoles; b-2) 1.38 femtomoles; b-3) 13.8 attomoles.
The F. tularensis iMALDI assay, based on the anti-F. tularensis IglC, aa49-61 antibody, can also detect the target F. tularensis peptide from a bacterial digest. The target F. tularensis peptide was determined in a bacterial digest equivalent to 80 bacteria. The bacteria were digested and incubated with a small aliquot (1-5 μL) of anti-aa 49-61 NIVAIEGGEDVTK antibody beads. One tenth of the antibody beads were spotted on the MALDI target plate and analyzed directly. Although there were signals from some unknown impurities or non-specifically bound peptides from, for example, the bacterial digest, the target peptide was still detectable by its mass. The singly-charged, epitope-containing tryptic peptide (aa 49-61 NIVAIEGGEDVTK) from the IglC protein was observed at m/z = 1344.7 (Figure 4). Therefore the detection limit for bacteria in PBS solution is determined to be 8 CFU bacteria on target by using 50% of the antibody beads incubated with 50μL of a bacterial solution in PBS, at a concentration of 320 CFU mL-1, which is as low as the most sensitive detection systems yet developed [51, 52]. It should be noted that 8 CFU does not represent the lowest possible detection limit in real applications, but is an estimate of the lowest possible detection limit of our method, as the tryptic digestion of the protein equivalent of 8 CFU might be difficult.
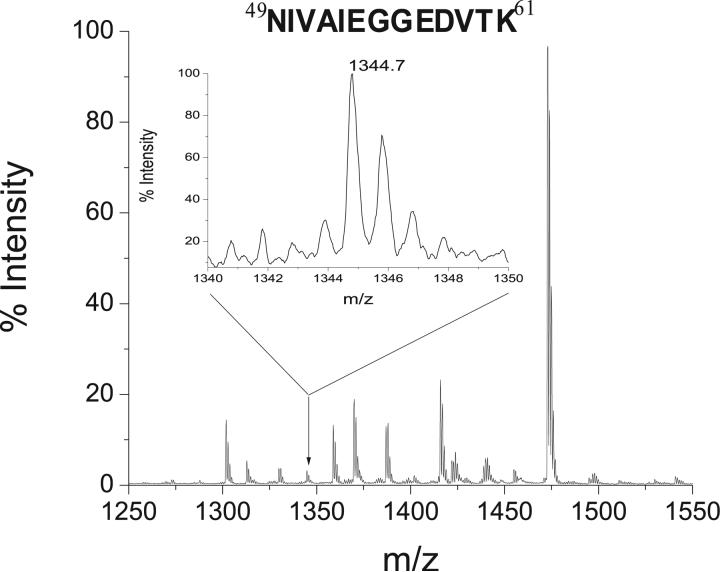
Figure 4. Detection of F. tularensis bacteria in PBS solution using the F. tularensis iMALDI assay.
MALDI-MS spectrum of peptides obtained after proteolysis of F. tularensis bacteria in PBS solution, affinity-bound to anti-aa49-61 (F. tularensis IglC) antibody beads. The singly-charged epitope-containing tryptic peptide (aa 49-61 F. tularensis IglC protein) is observed at m/z = 1344.7 (see inset). The spectrum represents the amount of IglC peptide equivalent to 8 CFU for F. tularensis bacteria.
3.1.2. Detection of F. tularensis bacteria in blood
The following detection limits were determined for the synthetic F. tularensis IglC, aa49-61 and F. tularensis bacteria spiked into blood samples (plasma): 69 attomoles of the F. tularensis IglC aa49-61 peptide and 800 CFU of bacteria (Figure 5) on target by using 50% of the antibody beads incubated with 125μL of spiked plasma, at a concentration of 1 femtomole mL-1 IglC aa49-61 peptide and 1280 CFU mL-1 bacteria, respectively. Although this method is not as sensitive for the detection of F. tularensis bacteria in blood as it is for the detection of bacteria in PBS solution, the detection limit is still comparable to most ELISA methods [24, 53]. However, our technology has the advantage of greater safety because we are detecting bacterial peptides after the bacteria have been inactivated by lysis and proteolysis. In addition, our technology has higher specificity, since tandem mass spectrometry is a molecular approach with sequencing capabilities to provide absolute identification of the target molecule.
Figure 5. Detection of F. tularensis bacteria in plasma samples using the F. tularensis iMALDI assay.
MALDI-MS spectrum of peptides obtained after proteolysis of F. tularensis bacteria being spiked in plasma digest, affinity-bound to anti-aa49-61 (F. tularensis IglC) antibody beads. The singly-charged epitope-containing tryptic peptide (aa 49-61 F. tularensis IglC protein) is observed at m/z = 1344.7 (see inset). The spectrum represents the amount of IglC peptide equivalent to 800 CFU for F. tularensis bacteria.
Due to the high virulence of bioterrorism pathogens, high sensitivity is one of the most important requirements in order to avoid “false negative” results. The sensitivity in plasma (800 CFU) is lower than in PBS solution (ca. 10 CFU bacteria), may be due to incomplete digestion and to high levels of non-specific binding of other plasma proteins which can suppress the ion signal from the target peptide. Optimized sample preparation protocols may alleviate this problem. In particular, a major advantage of this MS/MS-based technique is that the proteins which are the source of these non-specifically-bound peptides can be identified from the MS/MS spectra of their peptides, and depletion protocols can be specifically designed to remove these proteins prior to digestion and affinity capture of the target peptides [54]. Improved sample preparation protocols, and improvements in mass spectrometric detection technology, should lead to routine detection sensitivities of ∼10-100 attomoles of peptide.
3.1.3. Detection of F. tularensis bacteria in Nasal swab samples
The current technique is also usable for nasal swab analyses. Nasal swabs are widely used in clinical tests, and are a simple and useful method for collecting a wide range of respiratory viruses. The collection of a nasal swab is easy and painless, and it can easily be performed in remote locations [55]. In the mouse nasal swab samples collected 2 days after inoculation, a very low level of target peptide (m/z=1344.7) was detected (Figure 6a). The absence of the signal for this peptide in the uninfected mouse samples supports these results (Figure 6b). MS/MS was not performed on the ion at m/z=1344.7 because the ion abundance was below the instrument threshold for MS/MS acquisition. No bacteria were observed in a culture of the nasal swab solution from the infected animal (which later developed tularemia), thus demonstrating that iMALDI could detect F. tularensis at levels too low for successful culturing of the bacteria.
Figure 6. Detection of F. tularensis bacteria in nasal swab samples using the F. tularensis iMALDI assay.
a) MALDI-MS spectrum of peptides affinity-bound to anti-aa49-61 (F. tularensis IglC) antibody beads, obtained after proteolysis of mouse nasal swab extracts collected two days after the mice were inoculated with F. tularensis. The singly-charged, epitope-containing, tryptic peptide, NIVAIEGGEDVTK, corresponding to aa 49-61 of the F. tularensis IglC protein, was observed at m/z = 1344.7 (see inset). b) MALDI-MS spectrum of anti-aa 49-61 (F. tularensis IglC) antibody beads obtained after proteolysis of nasal swab extracts collected from uninfected mice on the same day.
3.2. Specificity
By “specificity” of the assay, we mean that the target peptide is unique to the organism (as determined by a BLAST search of the peptide sequence). Thus the detection of this peptide, at the appropriate MW and with the correct sequence is a positive indication of the presence of F. tularensis. The iMALDI can provide this specificity by combining two molecular characteristics of the epitope-containing peptides: i) the molecular weight, typically measured by MALDI-MS within an error of ≤100 ppm and ii) the amino acid sequence, determined by performing MS/MS on the same sample.
We have demonstrated that this iMALDI technology is able to accurately determine the molecular weight of an immunoaffinity-enriched F. tularensis peptide from a proteolytic digest of F. tularensis bacteria in PBS solution and blood. The molecular weight determination was accurate to within 60 ppm. Sequence information on the affinity-bound peptide was also obtained by MALDI-MS/MS (Figure 7a). MS/MS analysis produces high-abundance sequence-specific ions, resulting in an almost complete amino acid sequence of the peptide. These sequence-specific ions allow confident assignment of the target peptide (Figure 7b). Using the existing NCBInr database (2006.02.16), searching with only MS data, we retrieved 74,528 hits out of more than 3 million entries; in contrast, searching with combined MS and MS/MS data, resulted in only one hit. This demonstrates the specificity of this iMALDI technique for detecting F. tularensis. Here, we used polyclonal antibodies because of their ready availability. Polyclonal antibodies often contain more than a single epitope within a particular stretch of amino acids, and therefore, are able to capture even modified peptides since they are likely to contain an unmodified stretch of amino acids. This makes this detection method tolerant of small sequence variations. On the other hand, the use of polyclonal antibodies might lead to cross-reactivity with peptides from other species. This could decrease specificity and/or the detection limit of our method. This issue could be resolved by using a several monoclonal antibodies, or perhaps even both types of antibodies, for the final clinical version of this technique.
Figure 7. Highly specific detection of F. tularensis bacteria in PBS solution by mass spectrometric sequencing of the immunoaffinity-enriched F. tularensis IglC aa49-61 peptide, using the F. tularensis iMALDI assay.
a) MALDI-MS/MS spectrum of the peptide at m/z = 1344.7 affinity-bound to anti-aa49-61(F. tularensis IglC) antibody beads, obtained after proteolysis of F. tularensis bacteria in PBS solution. All of the abundant ions can be assigned to sequence-specific y- and b-ions of the F. tularensis IglC peptide aa49-61, resulting in unambiguous identification of the immunoaffinity-enriched peptide. b) This table shows the mass accuracies of the fragment ions, demonstrating that the assignment of these ion signals is correct. This therefore demonstrates that, using our F. tularensis iMALDI assay, F. tularensis bacteria can be detected with high specificity and correspondingly low “false positive” rates.
3.3. Quantitation
Mass spectrometry is well suited for peptide/protein quantitation. MS can perform relative quantitation using reference peptides from two different samples that have been differentially-labeled with stable isotopes, or absolute quantitation if a known amount of a stable-isotope labeled peptide has been added as an internal standard.
To determine the absolute concentration of a given peptide in a sample, and, therefore, the absolute concentration of the original protein, as is done in isotope dilution-mass spectrometry (ID-MS) [56], synthetic stable-isotopically labeled “heavy” peptide is used as an internal standard. These heavy peptides are identical in amino acid sequence to the native epitope-containing “light” peptides from the protein in the sample, but are higher in mass. They are added to the proteolytically-digested protein sample prior to incubation with the immobilized anti-peptide antibody. Following incubation, MALDI-MS analysis of the antibody beads shows doublets of ion signals from the “light” and “heavy” peptides. The relative abundances of the molecular ion signals corresponding to the “light” and “heavy” peptides are used to quantify the amount of the “light” peptide and therefore its parent protein in the original sample.
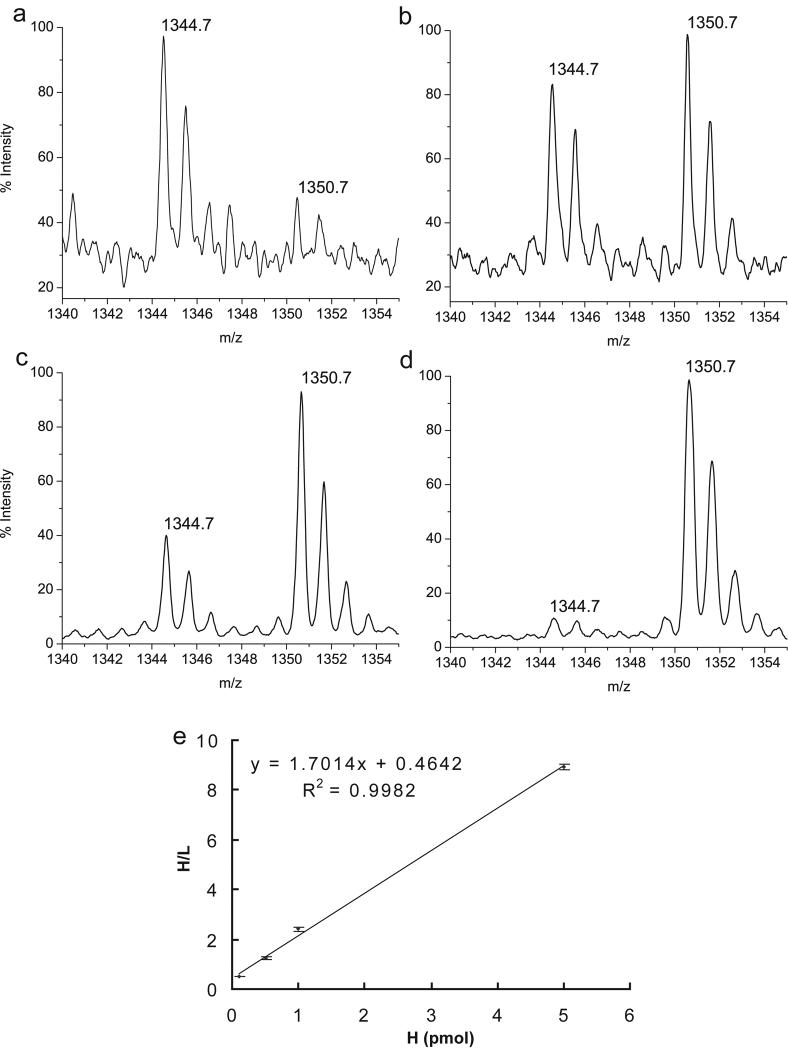
For quantifying F. tularensis IglC protein, the F. tularensis IglC aa 49-61 peptide 49NIVAIEGGEDVTK61 was synthesized with an isotopically-labeled valine at position 59 (underscored). This “heavy” peptide (H) is identical in amino acid sequence to the native epitope-containing “light” peptide (L), but is 6 Da higher in mass (m/z=1350.7) due to 6 13C’s in place of 6 12C’s. In these experiments, the heavy peptide was added in various amounts (100 femtomoles - 5 picomoles) to a proteolytic digestion of F. tularensis bacteria in PBS solution, and was immuno-adsorbed using the anti-F. tularensis IglC aa49-61 antibody immobilized on affinity beads (Figure 8a-d). Analysis of an aliquot of these beads spotted directly on the MALDI target reveals monoisotopic protonated molecular ions from the two peptides, separated by 6 Da. Figure 8e shows a linear correlation (R2=0.9988) between the ratio of the two peptides (H/L) and the amount of H spiked in as internal standard over near two orders of magnitude (from 100 femtomoles to 5 picomoles). The nearly perfect linear correlation demonstrates the stability of iMALDI for the absolute quantitation of F. tularensis peptides using an internal standard.
Figure 8. Quantitation of F. tularensis bacteria using the F. tularensis iMALDI assay.
Absolute quantitation of the IglC peptide NIVAIEGGEDVTK (aa 48-61) (L, light peptide, m/z = 1344.7) in a bacterial sample. F. tularensis bacteria were digested and incubated with different amounts of heavy peptides (H, m/z =1350.7) as internal standards: a) 0.1 picomoles, b) 0.5 picomoles, c) 1 picomoles, d) 5 picomoles, e) Plot of the observed ratios of monoisotopic abundances of H and L in the MALDI-MS spectra (a-d) versus the absolute amount of H added. Note, only a 10% aliquot has been used for the analysis.
Compared to the traditional culturing method and microagglutination (MA) test [2, 4, 10, 17, 20-23], iMALDI is more rapid, sensitive and specific. The peptide sequencing capability of tandem mass spectrometry in iMALDI provides higher molecular specificity than ELISA. The sensitivity of iMALDI is comparable to the most sensitive PCR method [26], but may not be as rapid when the digestion and incubation time is considered. However, the digestion time of iMALDI can be greatly reduced by using immobilized trypsin [57], and the incubation time can be reduced by using an antibody with high affinity. Moreover, compared to other methods, iMALDI has higher safety, better absolute quantitation capabilities, and improved high-throughput analysis capability which significantly reduce the cost per sample. One major disadvantage of iMALDI is that its overall quality highly depends on the affinity and specificity of the antibody. However, this problem should be able to be solved by using different strategies of antibody optimization, or alternative affinity-capture materials such as aptamers [58, 59].
4. Conclusions
We have shown that the combination of two mass spectrometric approaches (MALDI-MS and MALDI-MS/MS), inherent in our iMALDI approach, can unambiguously identify affinity-bound peptides, and therefore, permits specific detection of F. tularensis bacteria. The F. tularensis iMALDI can detect F. tularensis bacteria in PBS solution at a sensitivity of better than 10 CFU of bacteria. Since both the molecular weight and the sequence of the bacterial peptide is determined at high accuracy, the high sensitivity of this technique means a low rate of “false negatives”, and the high specificity means a low rate of “false positives”. In addition, the iMALDI F. tularensis peptide assay is adequate for accurate and absolute quantitation of the target protein concentration. With the addition of robotic liquid handling systems, it would be an even safer technique, as well as being capable of high-throughput analyses. This would make iMALDI an extremely valuable tool for the early detection of F. tularensis and other bioterrorist agents.
Acknowledgements
We thank the UNC-Duke Michael Hooker Proteomics Center (which was partially supported by a gift from an anonymous donor) and the UNC Peptide Synthesis Core. We also thank the Southeast Regional Center of Excellence for Emerging Infections and Biodefense (SERCEB, 5U54AI057157-04) for funding for this project.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Gallagher-Smith M, Kim J, Al-Bawardi R, Josko D. Clin. Lab. Sci. 2004;17:35. [PubMed] [Google Scholar]
- [2].Saslaw S, Eigelsbach HT, Wilson HE, Prior JA, Carhart S. Arch. Intern. Med. 1961;107:689. doi: 10.1001/archinte.1961.03620050055006. [DOI] [PubMed] [Google Scholar]
- [3].Dedie K, Bockemuehl J, Kuehn H, Volkmer K-J, Weinke T. Ferdinand Enke Verlag. Stuttgart: 1993. p. 363. [Google Scholar]
- [4].Saslaw S, Eigelsbach HT, Prior JA, Wilson HE, Carhart S. Arch. Intern. Med. 1961;107:702. doi: 10.1001/archinte.1961.03620050068007. [DOI] [PubMed] [Google Scholar]
- [5].Hornick R. N. Engl. J. Med. 2001;345:1637. doi: 10.1056/NEJM200111293452211. [DOI] [PubMed] [Google Scholar]
- [6].Karwa M, Bronzert P, Kvetan V. Critical Care Clinics. 2003;19:279. doi: 10.1016/s0749-0704(02)00053-2. [DOI] [PubMed] [Google Scholar]
- [7].Ohara Y, Sato T, Fujita H, Ueno T, Homma M. Infection. 1991;19:14. doi: 10.1007/BF01643750. [DOI] [PubMed] [Google Scholar]
- [8].Penn RL. In: Principles and Practice of Infectious Diseases. 4th Edition Tularensis F, editor. Churchill Livingstone: 1995. p. 2060. [Google Scholar]
- [9].Khan AS, Morse S, Lillibridge SR. Lancet. 2000;356:179. doi: 10.1016/S0140-6736(00)02769-0. [DOI] [PubMed] [Google Scholar]
- [10].Evans D, Freidlander AM. In: Textbook of Military Medicine, Office of The Surgeon General. Bellamy RF, editor. Department of the Army, United States of America; Bethesda, MD: 1997. p. 503. [Google Scholar]
- [11].Dennis DT, Inglesby TV, Henderson DA, Bartlett JG, Ascher MS, Eitzen E, Fine AD, Friedlander AM, Hauer J, Layton M, Lillibridge SR, McDade JE, Osterholm MT, O’Toole T, Parker G, Perl TM, Russel PK, Thonat K. JAMA. 2001;285:2763. doi: 10.1001/jama.285.21.2763. [DOI] [PubMed] [Google Scholar]
- [12].Ellis J, Oyston PCF, Green ME, Titball RW. Clin. Microbiol. Rev. 2002;15:631. doi: 10.1128/CMR.15.4.631-646.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Firmani MA, Broussard LA. Expert Rev. Mol. Diagn. 2003;3:605. doi: 10.1586/14737159.3.5.605. [DOI] [PubMed] [Google Scholar]
- [14]. http://www.vet.uga.edu/vpp/IVM/ENG/Modes/bioagents.htm.
- [15].Khan AS, Ashford DA. N. Engl. J. Med. 2001;345:287. doi: 10.1056/NEJM200107263450411. [DOI] [PubMed] [Google Scholar]
- [16].1999 www.microbes-edu.org/professionel/diag/francisella.htm.
- [17].Chu MC, Weyant R. In: Manual of Clinical Microbiology. 8th edition Murray PR, Baron EJ, Jorgensen JH, Pfaller MA, Yolken RH, editors. American Society for Microbioloy; Washington, DC: 2003. [Google Scholar]
- [18].Pike RM. Health Lab. Sci. 1976;13:105. [PubMed] [Google Scholar]
- [19].Junhui Z, Ruifu Y, Jianchun L, Songle Z, Meiling C, Fengxiang C, Hong C. J. Med. Microbiol. 1996;45:477. doi: 10.1099/00222615-45-6-477. [DOI] [PubMed] [Google Scholar]
- [20].Evans ME, Gregory DW, Schaffner W, McGee ZA. Medicine; analytical reviews of general medicine, neurology, psychiatry, dermatology, and pediatrics. 1985;64:251. [PubMed] [Google Scholar]
- [21].Sato T, Fujita H, Ohara Y, Homma M. J. Clin. Microbiol. 1990;28:2372. doi: 10.1128/jcm.28.10.2372-2374.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Koskela P, Salminen A. J. Clin. Microbiol. 1985;22:973. doi: 10.1128/jcm.22.6.973-979.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Syrjala H, Koskela P, Ripatti T, Salminen A, Herva E. J. Infect. Dis. 1986;153:142. doi: 10.1093/infdis/153.1.142. [DOI] [PubMed] [Google Scholar]
- [24].Grunow R, Splettstoesser W, McDonald S, Otterbein C, O’Brien T, Morgan C, Aldrich J, Hofer E, Finke E-J, Meyer H. Clin. Diagn. Lab. Immunol. 2000;7:86. doi: 10.1128/cdli.7.1.86-90.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Kischel N. Vergleich von ELISA, Immunfluoreszenz, Durchflußzytometrie, Westernblot und Agglutinationstest zum Nachweis von Serumantikörpern gegen Francisella tularensis. München: 2003. Dissertation eingereicht bei: Technische Universität München, Fakultät für Medizin, 2002-05-23. [Google Scholar]
- [26].Emanuel PA, Bell R, Dang JL, McClanahan R, David JC, Burgess RJ, Thompson J, Collins L, Hadfield T. J. Clin. Microbiol. 2003;41:689. doi: 10.1128/JCM.41.2.689-693.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Yang S, Rothman RE. Lancet Infect. Dis. 2004;4 doi: 10.1016/S1473-3099(04)01044-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Jiang J, Parker CE, Hoadley KA, Perou CM, Boysen G, Borchers CH. Proteomics. 2007 doi: 10.1002/prca.200700009. Accepted. [DOI] [PubMed] [Google Scholar]
- [29]. www.ncbi.nlm.nih.gov/Genbank/
- [30].Warren EN, Jiang J, Parker CE, Borchers CH. BioTechniques. 2005;38:S7. doi: 10.2144/05386su01. [DOI] [PubMed] [Google Scholar]
- [31].Warren MRE, Parker CE, Mocanu V, Klapper DG, Borchers CH. Rapid Communic. Mass Spectrom. 2005;19:429. doi: 10.1002/rcm.1798. [DOI] [PubMed] [Google Scholar]
- [32].Jiang J, Parker CE, Robinette D, Borchers CH. BIOforum Europe. 2006:18. [Google Scholar]
- [33].Niederkofler EE, Tubbs KA, Gruber K, Nedelkov D, Kiernan UA, Williams P, Nelson RW. Anal. Chem. 2001;73:3294. doi: 10.1021/ac010143j. [DOI] [PubMed] [Google Scholar]
- [34].R.W.K. Nelson JR, Bieber AL, Williams P. Anal. Chem. 1995;67:1153. doi: 10.1021/ac00103a003. [DOI] [PubMed] [Google Scholar]
- [35].Anderson NL, Anderson NG, Haines LR, Hardie DB, Olafson RW, Pearson TW. J. Proteome Res. 2004;3:235. doi: 10.1021/pr034086h. [DOI] [PubMed] [Google Scholar]
- [36].Niederkofler EE, Tubbs KA, Gruber K, Nedelkov D, Kiernan UA, Williams P, Nelson RW. Anal. Chem. 2001;73:3294. doi: 10.1021/ac010143j. [DOI] [PubMed] [Google Scholar]
- [37].Brockman AH, Orlando R. Anal. Chem. 1995;67:4581. doi: 10.1021/ac00120a024. [DOI] [PubMed] [Google Scholar]
- [38].Tubbs KA, Kiernan UA, Niederkofler EE, Nedelkov D, Bieber AL, Nelson RW. Anal. Chem. 2006;78:3271. doi: 10.1021/ac060013g. [DOI] [PubMed] [Google Scholar]
- [39].Nedelkov D. Expert Rev. Proteomics. 2006;3:631. doi: 10.1586/14789450.3.6.631. [DOI] [PubMed] [Google Scholar]
- [40].L.H. Cazares GW, Jr, Leung SM, Nasim S, Adam BL, Yip TT, Schellhammer PF, Gong L, Vlahou A. Prostate Cancer Prostatic Dis. 1999;2:264. doi: 10.1038/sj.pcan.4500384. [DOI] [PubMed] [Google Scholar]
- [41].Hlavaty J, Partin A, Kusinitz F, Shue M, Stieg A. Clin. Chem. 2001 e. al. [Google Scholar]
- [42].Paweletz CP, Trock B, Pennanen M, Tsangaris T, Magnant C, Liotta LA, Petricoin EF., 3rd Dis. Markers. 2001;17:301. doi: 10.1155/2001/674959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Vlahou A, Schellhammer PF, Mendrinos S, Patel K, Kondylis FI, Gong L, Nasim S, Wright GL., Jr, Jr. Am. J. Pathol. 2001;158:1491. doi: 10.1016/S0002-9440(10)64100-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Petricoin E, Ardekani A, Hitt B, Levine P, Fusaro V , Lancet. 2002;359:572. doi: 10.1016/S0140-6736(02)07746-2. e. al. [DOI] [PubMed] [Google Scholar]
- [45].Parker C, Papac D, Trojak S, Tomer K. J. Immunol. 1996;157:198. [PubMed] [Google Scholar]
- [46].Papac DI, Hoyes J, Tomer KB. Anal. Chem. 1994;66:2609. [Google Scholar]
- [47].Raska C, Parker C, Sunnarborg S, Pope R, Lee D. J. Am. Soc. Mass Spectrom. 2003;14:1076. doi: 10.1016/S1044-0305(03)00405-7. e. al. [DOI] [PubMed] [Google Scholar]
- [48].Raska CS, Parker CE, Dominski Z, Marzluff WF, Glish GL, Pope RM, Borchers CH. Anal. Chem. 2002;74:3429. doi: 10.1021/ac0111199. [DOI] [PubMed] [Google Scholar]
- [49].Hutchens TW, Yip TT. Rapid Commun. Mass Spectrom. 1993;7:576. doi: 10.1002/(SICI)1097-0231(199611)10:14<1797::AID-RCM754>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- [50].Schriemer DC, Li L. Anal. Chem. 1996;68:3382. doi: 10.1021/ac960219p. [DOI] [PubMed] [Google Scholar]
- [51].Versage JL, Severin DDM, Chu MC, Petersen JM. J. Clin. Microbiol. 2003;41:5492. doi: 10.1128/JCM.41.12.5492-5499.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Grunow R, Splettstoesser W, McDonald S, Otterbein C, O’Brien T, Morgan C, Aldrich J, Hofer E, Finke EJ, Meyer H. Clin. Diagn. Lab. Immunol. 2000;7:86. doi: 10.1128/cdli.7.1.86-90.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Viljanen MK, Nurmi T, Salminen A. J. Infect. Dis. 1983;148:715. doi: 10.1093/infdis/148.4.715. [DOI] [PubMed] [Google Scholar]
- [54].Scarlett CO, Mocanu V, Jiang J, Lessey BA, Dicheva NN, Parker CE, Borchers CH. Proceeding of the 53rd Annual Conference on Mass Spectrometry and Allied Topics; San Antonio, TX. June 5-9, 2005.2005. [Google Scholar]
- [55].Heikkinen T, Marttila J, Salmi AA, Ruuskanen O. J. Clin. Microbiol. 2002;40:4337. doi: 10.1128/JCM.40.11.4337-4339.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Barr JR, Maggio VL, Patterson DG, Jr., Cooper GR, Henderson LO, Turner WE, Smith SJ, Hannon WH, Needham LL, Sampson EJ. Clin. Chem. 1996;42:1676. [PubMed] [Google Scholar]
- [57].Freije JR, Mulder PPMFA, Werkman W, Rieux L, Niederlander HAG, Verpoorte E, Bischoff R. J. Proteome Res. 2005;4:1805. doi: 10.1021/pr050142y. [DOI] [PubMed] [Google Scholar]
- [58].Xu W, Ellington AD. Proc. Natl. Acad. Sci. USA. 1996;93:7475. doi: 10.1073/pnas.93.15.7475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].McCauley TG, Hamaguchi N, Stanton M. Anal. Biochem. 2003;319:244. doi: 10.1016/s0003-2697(03)00297-5. [DOI] [PubMed] [Google Scholar]