Abstract
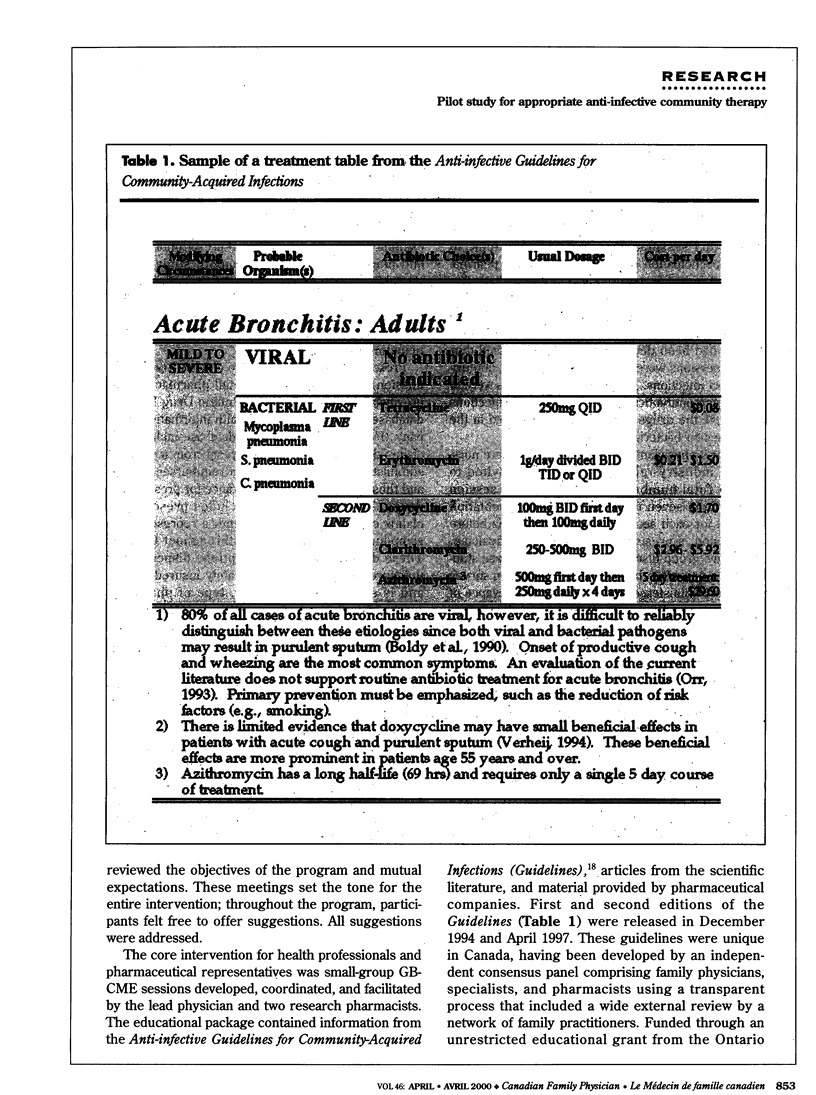
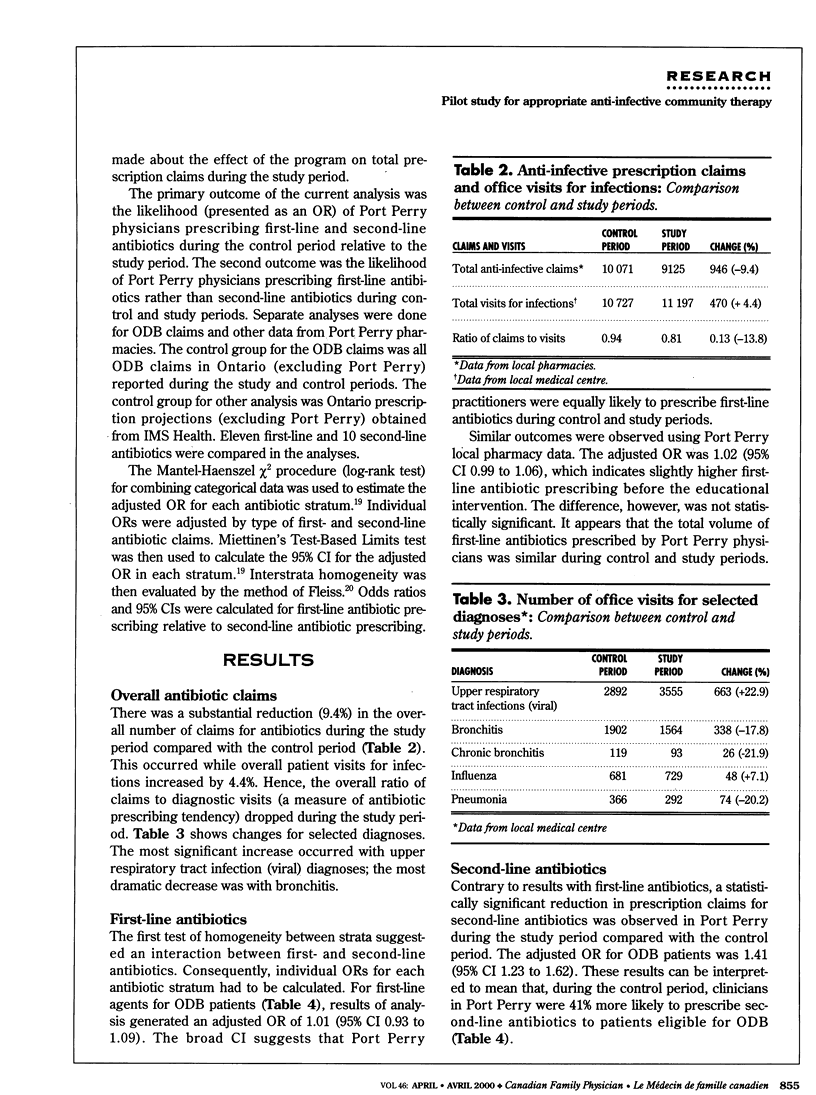
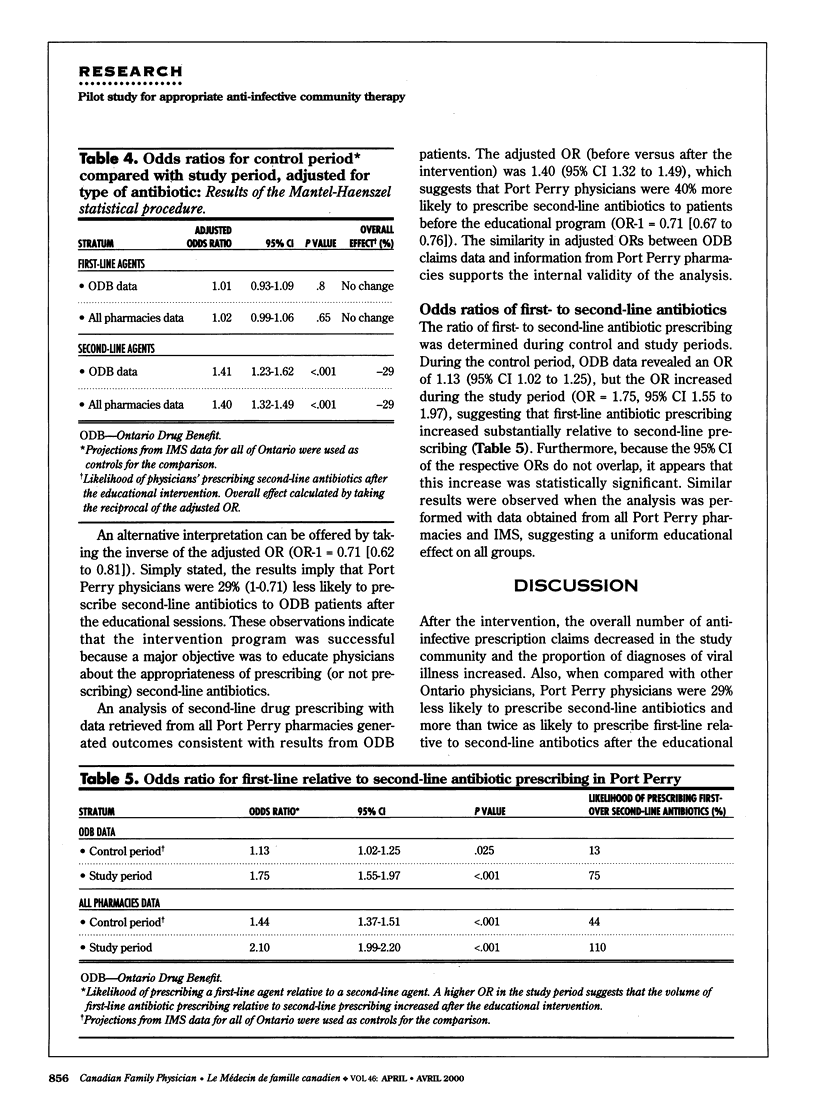
OBJECTIVE: To determine whether a community-wide, multi-intervention educational strategy (CoMPLI model) could enhance adoption of clinical guidelines and improve the use of antibiotics. DESIGN: Before-after trial using baseline and study periods with a control group. SETTING: A small community in central Ontario. PARTICIPANTS: Health professionals, the general public, and the pharmaceutical industry. INTERVENTIONS: The educational strategy (CoMPLI), carried out during 6 winter months, consisted of continuing medical education sessions for health professionals and pharmaceutical representatives and a parallel public education campaign that included town hall meetings and pamphlets distributed by local pharmacists. The two main messages were: do not use antibiotics for viral respiratory infections, and use drugs recommended in the publication, Anti-infective Guidelines for Community-Acquired Infections. MAIN OUTCOME MEASURES: Total number of antibiotic claims and adjusted odds ratios (OR) were used to measure the likelihood of physicians prescribing first- or second-line agents compared with the previous year and compared with control physicians. RESULTS: Claims in the study community decreased by nearly 10% during the 6-month study period compared with the baseline period from the previous year. Study physicians were 29% less likely (OR-1 = 0.71, range 0.67 to 0.76) to prescribe second-line antibiotics during the study period than physicians in the rest of the province. CONCLUSIONS: Physicians participating in the pilot study were more likely to follow drug recommendations outlined in published guidelines.
Full text
PDF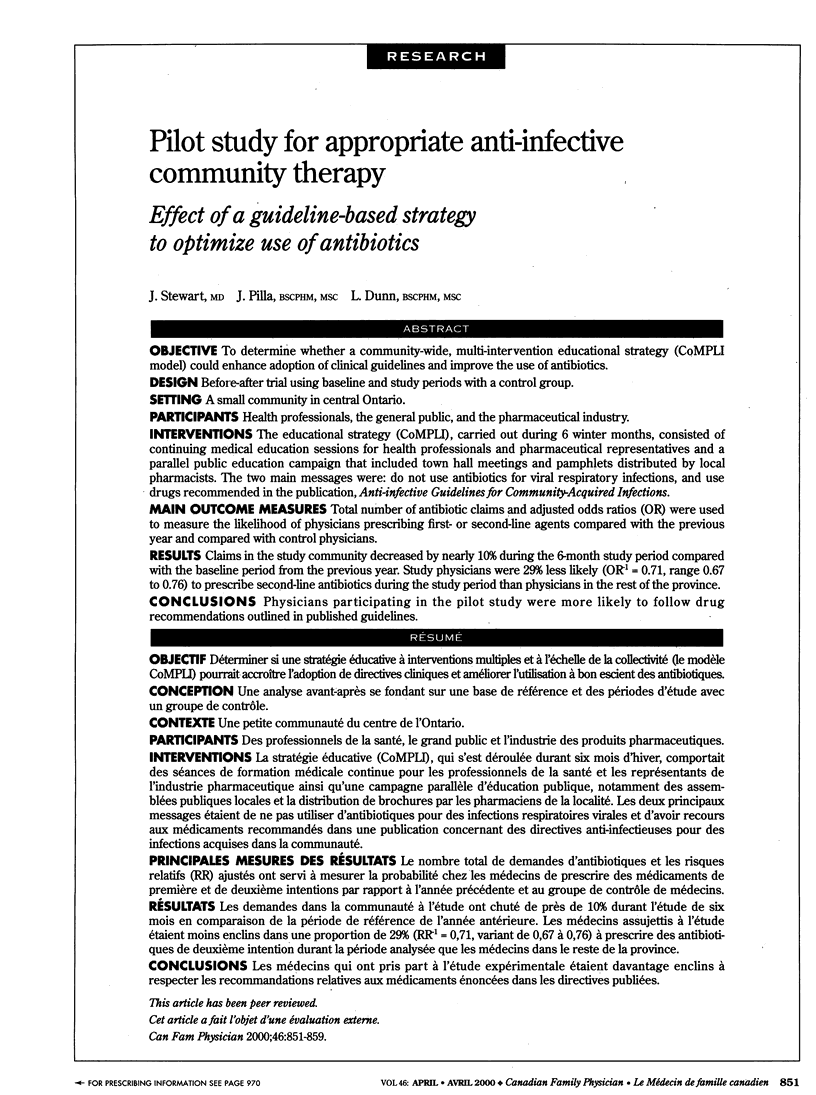



Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Avorn J., Soumerai S. B. Improving drug-therapy decisions through educational outreach. A randomized controlled trial of academically based "detailing". N Engl J Med. 1983 Jun 16;308(24):1457–1463. doi: 10.1056/NEJM198306163082406. [DOI] [PubMed] [Google Scholar]
- Davies H. D., McGeer A., Schwartz B., Green K., Cann D., Simor A. E., Low D. E. Invasive group A streptococcal infections in Ontario, Canada. Ontario Group A Streptococcal Study Group. N Engl J Med. 1996 Aug 22;335(8):547–554. doi: 10.1056/NEJM199608223350803. [DOI] [PubMed] [Google Scholar]
- Davis D. A., Taylor-Vaisey A. Translating guidelines into practice. A systematic review of theoretic concepts, practical experience and research evidence in the adoption of clinical practice guidelines. CMAJ. 1997 Aug 15;157(4):408–416. [PMC free article] [PubMed] [Google Scholar]
- Davis D. A., Thomson M. A., Oxman A. D., Haynes R. B. Evidence for the effectiveness of CME. A review of 50 randomized controlled trials. JAMA. 1992 Sep 2;268(9):1111–1117. [PubMed] [Google Scholar]
- Domenighetti G., Luraschi P., Casabianca A., Gutzwiller F., Spinelli A., Pedrinis E., Repetto F. Effect of information campaign by the mass media on hysterectomy rates. Lancet. 1988 Dec 24;2(8626-8627):1470–1473. doi: 10.1016/s0140-6736(88)90943-9. [DOI] [PubMed] [Google Scholar]
- Gonzales R., Steiner J. F., Sande M. A. Antibiotic prescribing for adults with colds, upper respiratory tract infections, and bronchitis by ambulatory care physicians. JAMA. 1997 Sep 17;278(11):901–904. [PubMed] [Google Scholar]
- Griffin M. R., Ray W. A., Schaffner W. Nonsteroidal anti-inflammatory drug use and death from peptic ulcer in elderly persons. Ann Intern Med. 1988 Sep 1;109(5):359–363. doi: 10.7326/0003-4819-109-5-359. [DOI] [PubMed] [Google Scholar]
- Neu H. C. The crisis in antibiotic resistance. Science. 1992 Aug 21;257(5073):1064–1073. doi: 10.1126/science.257.5073.1064. [DOI] [PubMed] [Google Scholar]
- Nyquist A. C., Gonzales R., Steiner J. F., Sande M. A. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998 Mar 18;279(11):875–877. doi: 10.1001/jama.279.11.875. [DOI] [PubMed] [Google Scholar]
- Schaffner W., Ray W. A., Federspiel C. F., Miller W. O. Improving antibiotic prescribing in office practice. A controlled trial of three educational methods. JAMA. 1983 Oct 7;250(13):1728–1732. [PubMed] [Google Scholar]
- Seppälä H., Klaukka T., Vuopio-Varkila J., Muotiala A., Helenius H., Lager K., Huovinen P. The effect of changes in the consumption of macrolide antibiotics on erythromycin resistance in group A streptococci in Finland. Finnish Study Group for Antimicrobial Resistance. N Engl J Med. 1997 Aug 14;337(7):441–446. doi: 10.1056/NEJM199708143370701. [DOI] [PubMed] [Google Scholar]
- Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA. 1996 Jan 17;275(3):175–175. [PubMed] [Google Scholar]
- Willcox S. M., Himmelstein D. U., Woolhandler S. Inappropriate drug prescribing for the community-dwelling elderly. JAMA. 1994 Jul 27;272(4):292–296. [PubMed] [Google Scholar]


