Abstract
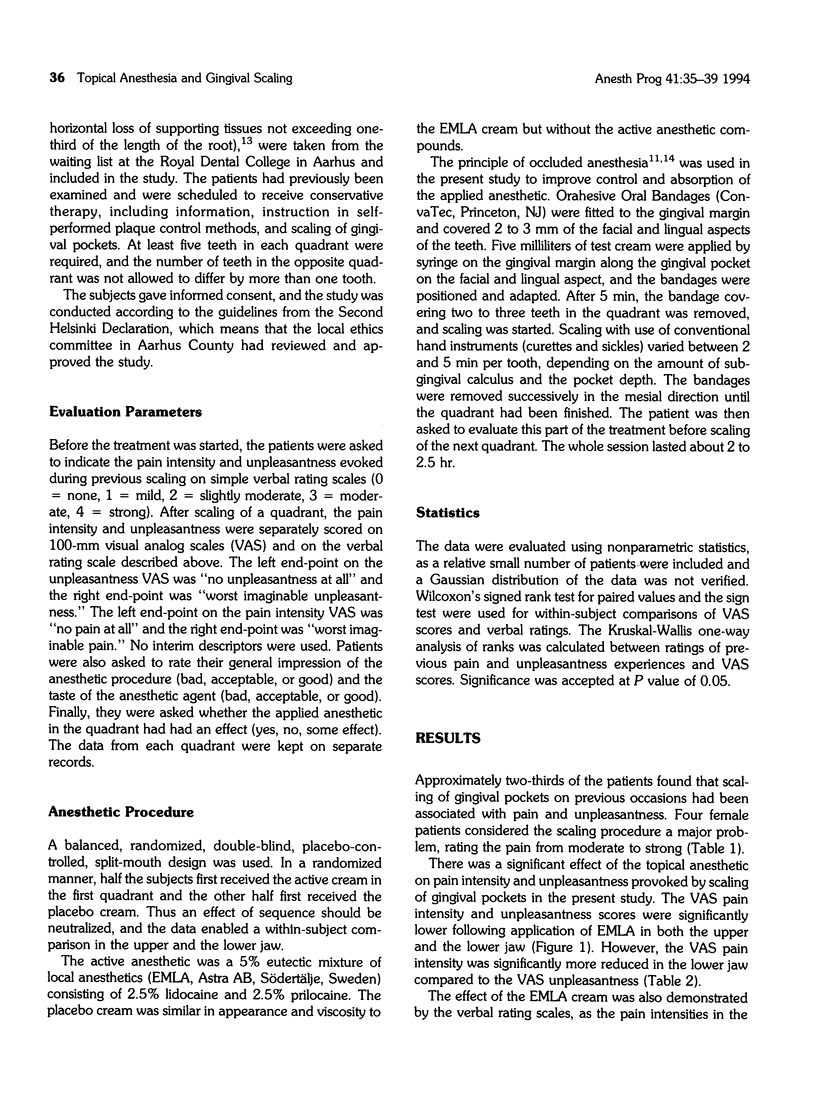
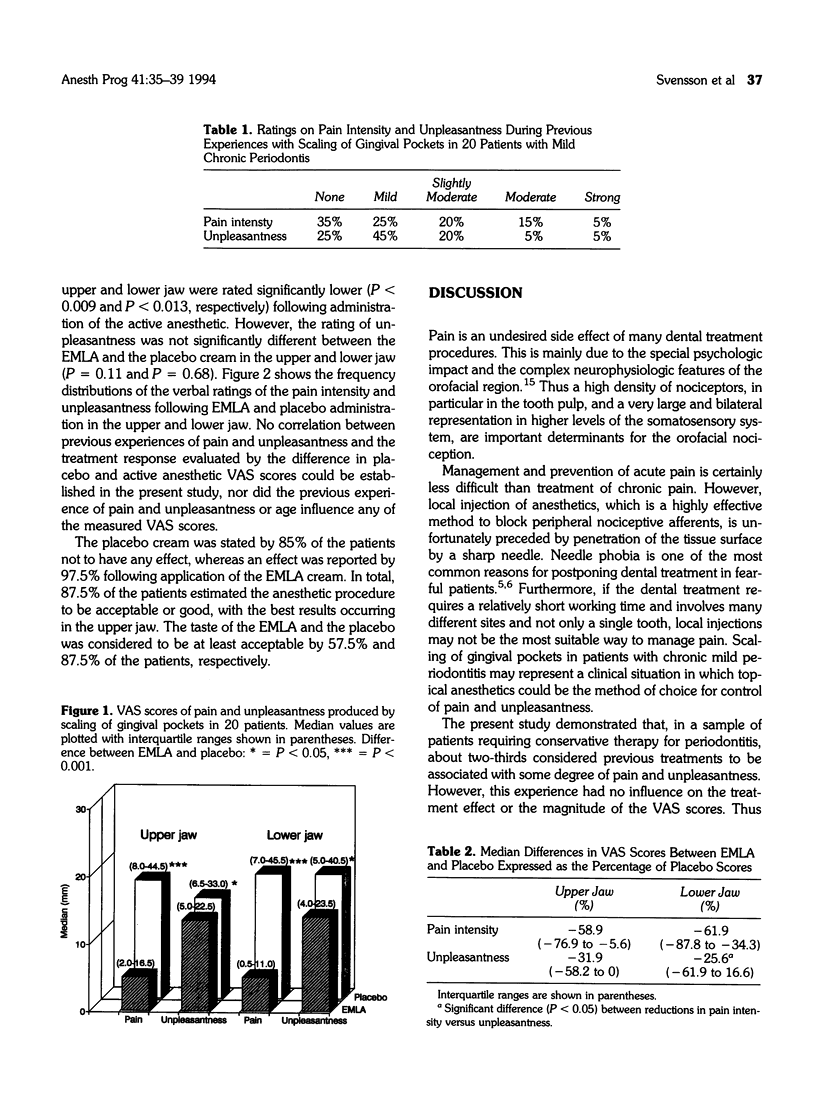
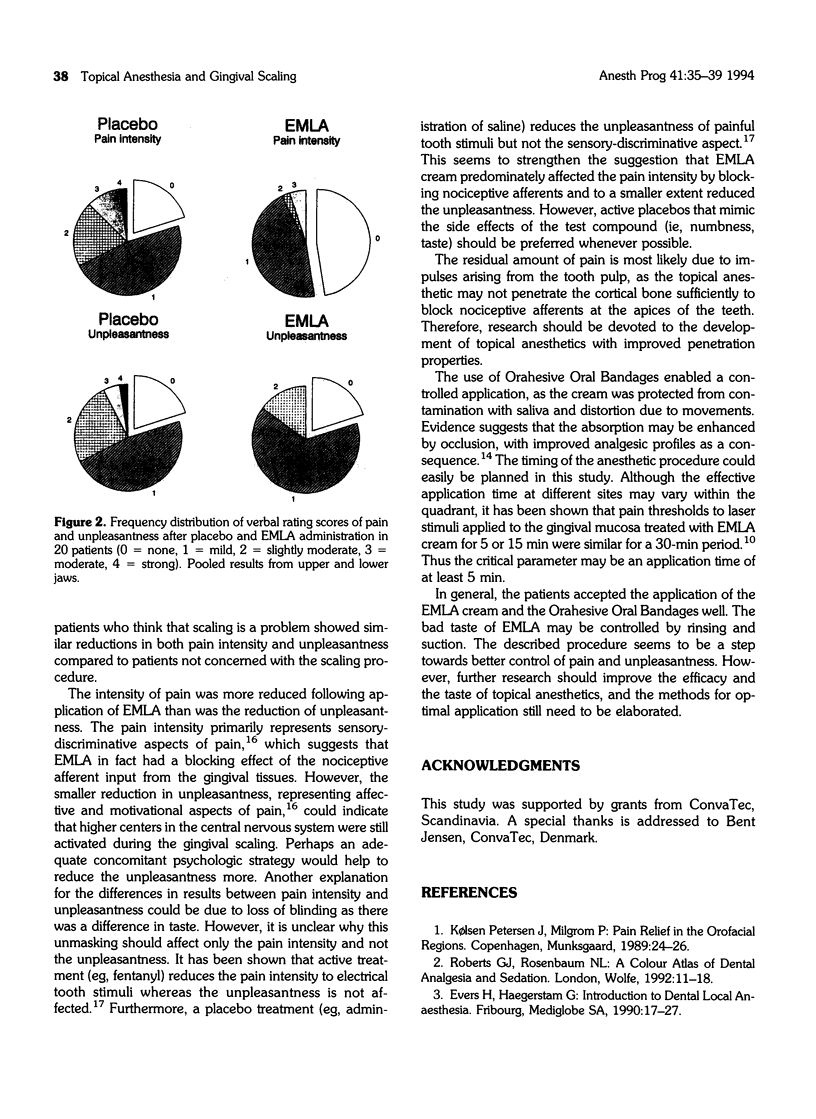
The efficacy of a topical anesthetic on pain and unpleasantness provoked by scaling of gingival pockets was investigated in 20 patients with mild chronic periodontitis. A eutectic mixture of local anesthetics (EMLA) and a placebo cream, both occluded by Orahesive Oral Bandages, were applied in a balanced, randomized, double-blind, split-mouth design, which enabled within-subject comparison of the anesthetic and the placebo in the upper and the lower jaw. Pretreatment interviews showed that approximately two-thirds of the patients considered gingival scaling to be associated with some degree of pain and unpleasantness. Pain intensity and unpleasantness were evaluated on 100-mm visual analog scales (VAS). Application of EMLA reduced both pain intensity and unpleasantness significantly compared to placebo cream. Median reductions in VAS pain intensity in the upper and lower jaw were 58.9% and 61.9%, and corresponding reductions in VAS unpleasantness were 31.9% and 25.6%, respectively. Generally, the patients accepted the anesthetic procedure well. The residual perception of pain and unpleasantness following topical anesthesia may be dependent on activation of nonanesthetized nociceptive fibers in the tooth pulp. However, the present study clearly demonstrates the efficacy of a topical anesthetic in a clinical situation, which may be recommended as a simple pharmacologic strategy to reduce pain and unpleasantness during scaling procedures.
Full text
PDF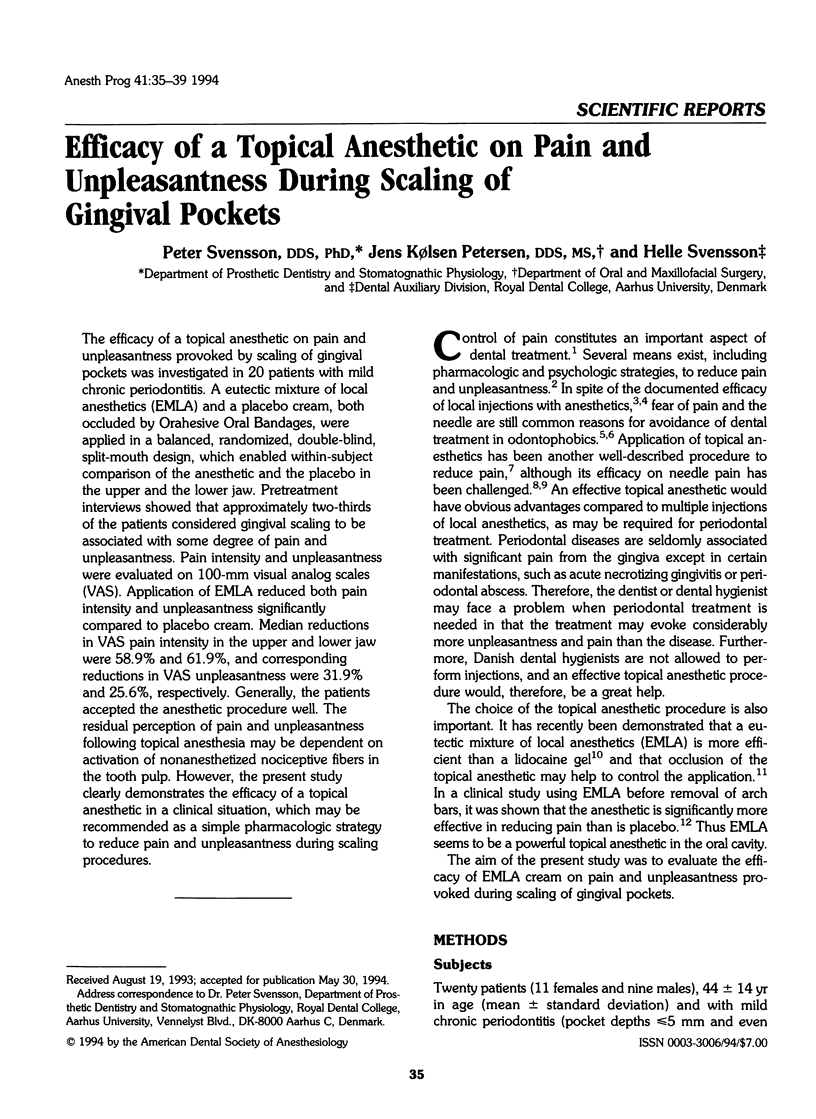
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Gill C. J., Orr D. L., 2nd A double-blind crossover comparison of topical anesthetics. J Am Dent Assoc. 1979 Feb;98(2):213–214. doi: 10.14219/jada.archive.1979.0476. [DOI] [PubMed] [Google Scholar]
- Gracely R. H., Dubner R., McGrath P. A. Narcotic analgesia: fentanyl reduces the intensity but not the unpleasantness of painful tooth pulp sensations. Science. 1979 Mar 23;203(4386):1261–1263. doi: 10.1126/science.424753. [DOI] [PubMed] [Google Scholar]
- Kincheloe J. E., Mealiea W. L., Jr, Mattison G. D., Seib K. Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int. 1991 Apr;22(4):311–315. [PubMed] [Google Scholar]
- Moore R., Brødsgaard I., Birn H. Manifestations, acquisition and diagnostic categories of dental fear in a self-referred population. Behav Res Ther. 1991;29(1):51–60. doi: 10.1016/s0005-7967(09)80007-7. [DOI] [PubMed] [Google Scholar]
- Pere P., Iizuka T., Rosenberg P. H., Lindqvist C. Topical application of 5% eutectic mixture of lignocaine and prilocaine (EMLA) before removal of arch bars. Br J Oral Maxillofac Surg. 1992 Jun;30(3):153–156. doi: 10.1016/0266-4356(92)90146-a. [DOI] [PubMed] [Google Scholar]
- Sessle B. J. The neurobiology of facial and dental pain: present knowledge, future directions. J Dent Res. 1987 May;66(5):962–981. doi: 10.1177/00220345870660052201. [DOI] [PubMed] [Google Scholar]
- Smith T., Milgrom P., Weinstein P. Evaluation of treatment at a dental fears research clinic. Spec Care Dentist. 1987 May-Jun;7(3):130–134. doi: 10.1111/j.1754-4505.1987.tb00622.x. [DOI] [PubMed] [Google Scholar]
- Svensson P., Arendt-Nielsen L., Bjerring P., Kaaber S. Oral mucosal analgesia quantitatively assessed by argon laser-induced thresholds and single-evoked vertex potentials. Anesth Pain Control Dent. 1993 Summer;2(3):154–161. [PubMed] [Google Scholar]
- Svensson P., Bjerring P., Arendt-Nielsen L., Kaaber S. Hypoalgesic effect of EMLA and lidocaine gel applied on human oral mucosa: quantitative evaluation by sensory and pain thresholds to argon laser stimulation. Anesth Prog. 1992;39(1-2):4–8. [PMC free article] [PubMed] [Google Scholar]
- Svensson P., Petersen J. K. Anesthetic effect of EMLA occluded with Orahesive oral bandages on oral mucosa. A placebo-controlled study. Anesth Prog. 1992;39(3):79–82. [PMC free article] [PubMed] [Google Scholar]


