Abstract
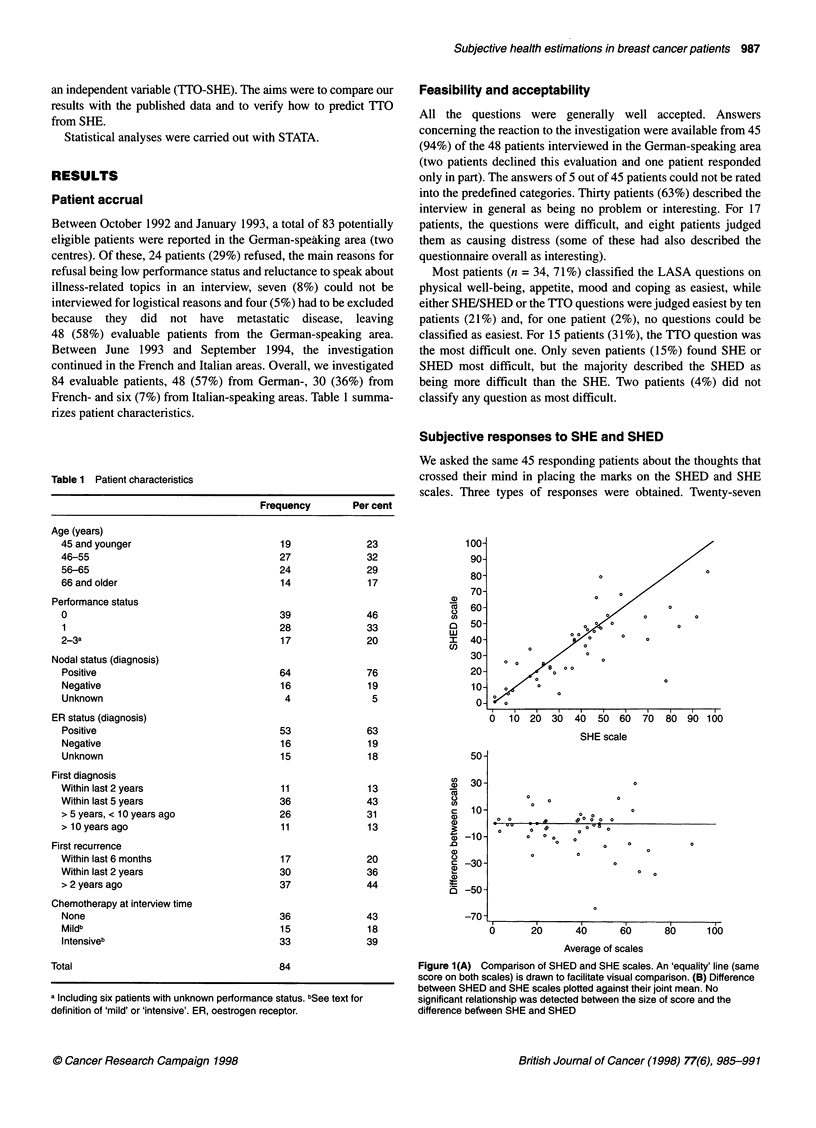
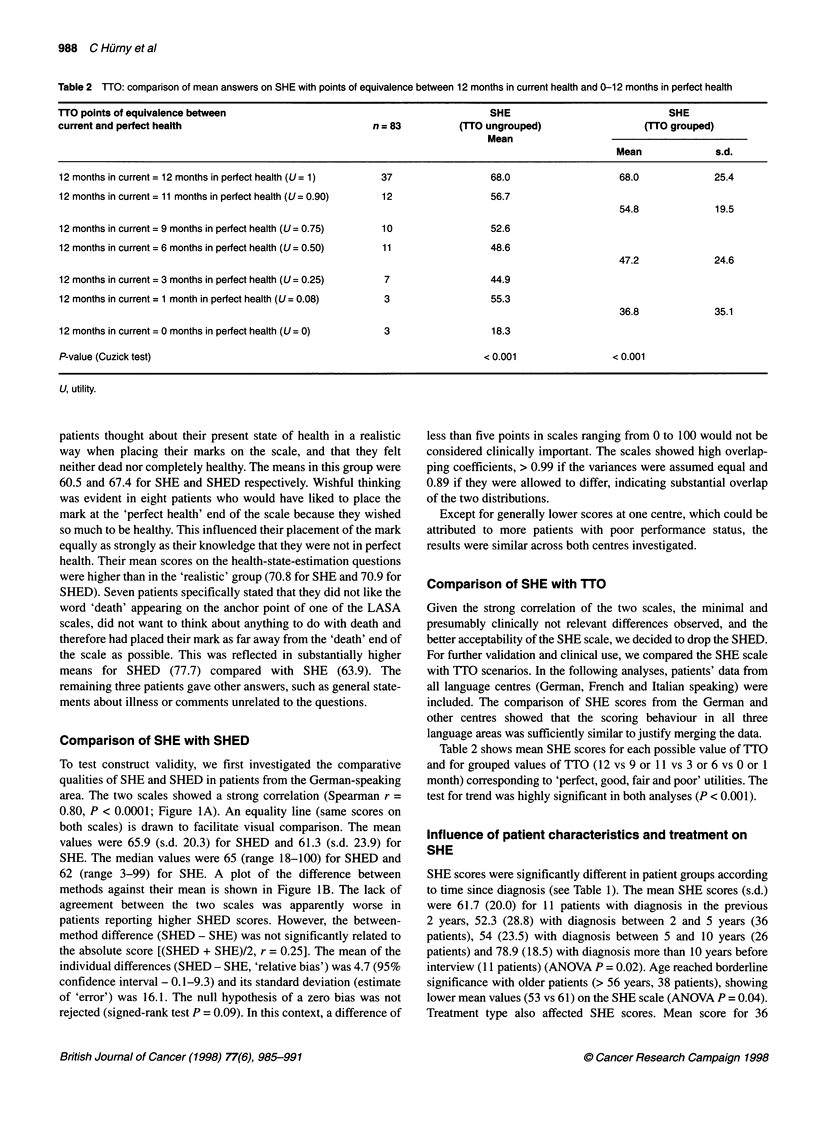
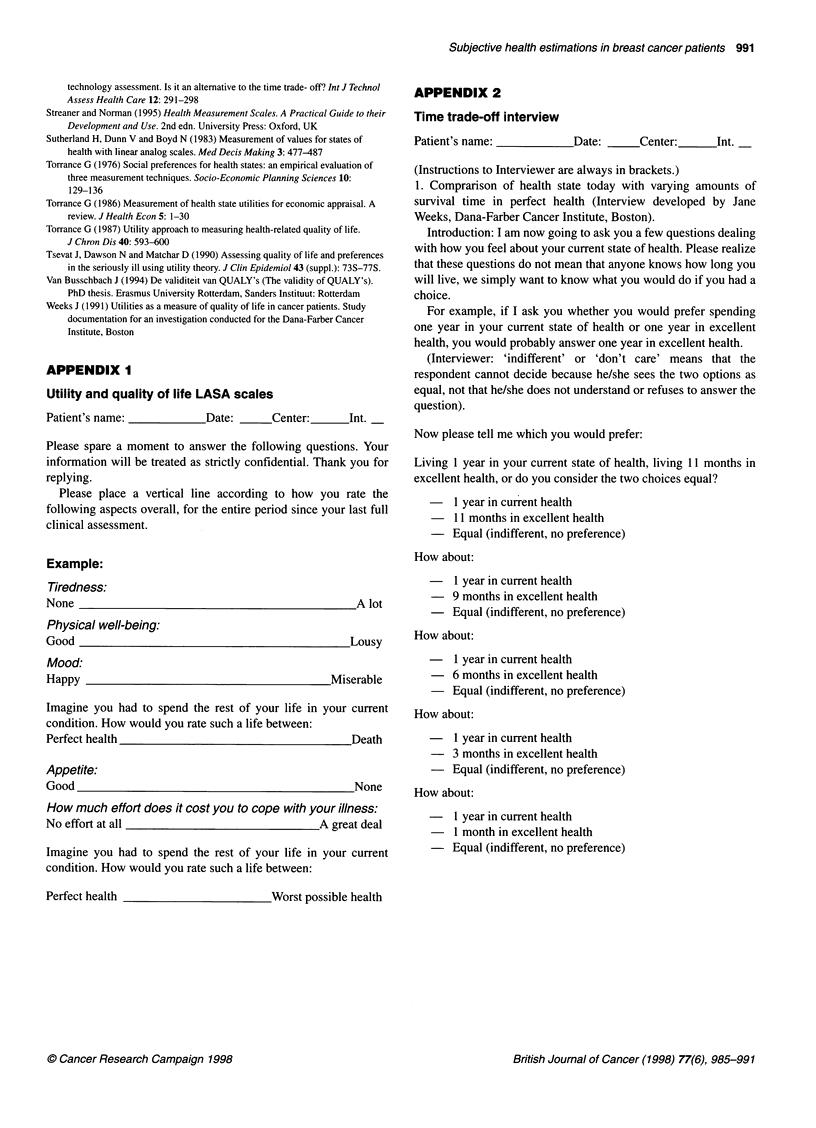
We wished to develop and validate a simple linear analogue self-assessment (LASA) scale to assess utility values in multicentre, multicultural breast cancer trials. We compared two variants of a LASA scale (score range 0-100) with different anchoring points [perfect health to worst possible health (subjective health estimation, SHE) and perfect health to death (SHED)] in 84 patients with advanced breast cancer. Feasibility was explored in the first 48 patients interviewed. Values from the LASA scales were compared with each other and with a time trade off (TTO) interview. Scores from the two LASA scales were highly correlated (r=0.8, P < 0.0001, Spearman). The relationship between TTO interview and SHE was confirmed with tests for trend across ordered groups (linear-trend test P < 0.001). Most patients preferred SHE to SHED. SHE scores (in which high scores indicate high-health-state values) were significantly different by type of treatment, time from diagnosis and age. Thus, significantly different mean SHE scores were obtained from patients receiving no treatment or hormone therapy, mild and intensive chemotherapy (ANOVA P=0.03) and from patients with diagnosis 2 years, 2-5 years, 5-10 years and more than 10 years before interview (ANOVA P=0.02). Older patients (> 56 years) had a lower mean on the SHE scale (53 vs 61; ANOVA P=0.04). We found that the two versions of the LASA scale were equivalent for clinical purposes. SHE appeared to provide a feasible, patient-preferred and valid alternative to lengthy TTO interviews in assessing the value patients attach to their present state of health in large-scale cancer clinical trials.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Ashby J., O'Hanlon M., Buxton M. J. The time trade-off technique: how do the valuations of breast cancer patients compare to those of other groups? Qual Life Res. 1994 Aug;3(4):257–265. doi: 10.1007/BF00434899. [DOI] [PubMed] [Google Scholar]
- Boyd N. F., Sutherland H. J., Heasman K. Z., Tritchler D. L., Cummings B. J. Whose utilities for decision analysis? Med Decis Making. 1990 Jan-Mar;10(1):58–67. doi: 10.1177/0272989X9001000109. [DOI] [PubMed] [Google Scholar]
- Carr-Hill R. A. Assumptions of the QALY procedure. Soc Sci Med. 1989;29(3):469–477. doi: 10.1016/0277-9536(89)90296-7. [DOI] [PubMed] [Google Scholar]
- Cuzick J. A Wilcoxon-type test for trend. Stat Med. 1985 Jan-Mar;4(1):87–90. doi: 10.1002/sim.4780040112. [DOI] [PubMed] [Google Scholar]
- Feeny D. H., Torrance G. W. Incorporating utility-based quality-of-life assessment measures in clinical trials. Two examples. Med Care. 1989 Mar;27(3 Suppl):S190–S204. doi: 10.1097/00005650-198903001-00016. [DOI] [PubMed] [Google Scholar]
- Feeny D., Furlong W., Barr R. D., Torrance G. W., Rosenbaum P., Weitzman S. A comprehensive multiattribute system for classifying the health status of survivors of childhood cancer. J Clin Oncol. 1992 Jun;10(6):923–928. doi: 10.1200/JCO.1992.10.6.923. [DOI] [PubMed] [Google Scholar]
- Gelber R. D., Cole B. F., Goldhirsch A., Rose C., Fisher B., Osborne C. K., Boccardo F., Gray R., Gordon N. H., Bengtsson N. O. Adjuvant chemotherapy plus tamoxifen compared with tamoxifen alone for postmenopausal breast cancer: meta-analysis of quality-adjusted survival. Lancet. 1996 Apr 20;347(9008):1066–1071. doi: 10.1016/s0140-6736(96)90277-9. [DOI] [PubMed] [Google Scholar]
- Gelber R. D., Goldhirsch A. A new endpoint for the assessment of adjuvant therapy in postmenopausal women with operable breast cancer. J Clin Oncol. 1986 Dec;4(12):1772–1779. doi: 10.1200/JCO.1986.4.12.1772. [DOI] [PubMed] [Google Scholar]
- Gerard K., Dobson M., Hall J. Framing and labelling effects in health descriptions: quality adjusted life years for treatment of breast cancer. J Clin Epidemiol. 1993 Jan;46(1):77–84. doi: 10.1016/0895-4356(93)90011-o. [DOI] [PubMed] [Google Scholar]
- Goldhirsch A., Gelber R. D., Simes R. J., Glasziou P., Coates A. S. Costs and benefits of adjuvant therapy in breast cancer: a quality-adjusted survival analysis. J Clin Oncol. 1989 Jan;7(1):36–44. doi: 10.1200/JCO.1989.7.1.36. [DOI] [PubMed] [Google Scholar]
- Guyatt G. H., Feeny D. H., Patrick D. L. Measuring health-related quality of life. Ann Intern Med. 1993 Apr 15;118(8):622–629. doi: 10.7326/0003-4819-118-8-199304150-00009. [DOI] [PubMed] [Google Scholar]
- Hürny C., Bernhard J., Bacchi M., van Wegberg B., Tomamichel M., Spek U., Coates A., Castiglione M., Goldhirsch A., Senn H. J. The Perceived Adjustment to Chronic Illness Scale (PACIS): a global indicator of coping for operable breast cancer patients in clinical trials. Swiss Group for Clinical Cancer Research (SAKK) and the International Breast Cancer Study Group (IBCSG). Support Care Cancer. 1993 Jul;1(4):200–208. doi: 10.1007/BF00366447. [DOI] [PubMed] [Google Scholar]
- Hürny C., Bernhard J., Coates A. S., Castiglione-Gertsch M., Peterson H. F., Gelber R. D., Forbes J. F., Rudenstam C. M., Simoncini E., Crivellari D. Impact of adjuvant therapy on quality of life in women with node-positive operable breast cancer. International Breast Cancer Study Group. Lancet. 1996 May 11;347(9011):1279–1284. doi: 10.1016/s0140-6736(96)90936-8. [DOI] [PubMed] [Google Scholar]
- Hürny C., Bernhard J., Gelber R. D., Coates A., Castiglione M., Isley M., Dreher D., Peterson H., Goldhirsch A., Senn H. J. Quality of life measures for patients receiving adjuvant therapy for breast cancer: an international trial. The International Breast Cancer Study Group. Eur J Cancer. 1992;28(1):118–124. doi: 10.1016/0959-8049(92)90399-m. [DOI] [PubMed] [Google Scholar]
- Jenkins C. D. Assessment of outcomes of health intervention. Soc Sci Med. 1992 Aug;35(4):367–375. doi: 10.1016/0277-9536(92)90329-o. [DOI] [PubMed] [Google Scholar]
- Kiebert G. M., Stiggelbout A. M., Leer J. W., Kievit J., de Haes H. J. Test-retest reliabilities of two treatment-preference instruments in measuring utilities. Med Decis Making. 1993 Apr-Jun;13(2):133–140. doi: 10.1177/0272989X9301300207. [DOI] [PubMed] [Google Scholar]
- Llewellyn-Thomas H., Sutherland H. J., Tibshirani R., Ciampi A., Till J. E., Boyd N. F. The measurement of patients' values in medicine. Med Decis Making. 1982 Winter;2(4):449–462. doi: 10.1177/0272989X8200200407. [DOI] [PubMed] [Google Scholar]
- McQuellon R. P., Muss H. B., Hoffman S. L., Russell G., Craven B., Yellen S. B. Patient preferences for treatment of metastatic breast cancer: a study of women with early-stage breast cancer. J Clin Oncol. 1995 Apr;13(4):858–868. doi: 10.1200/JCO.1995.13.4.858. [DOI] [PubMed] [Google Scholar]
- Mehrez A., Gafni A. Quality-adjusted life years, utility theory, and healthy-years equivalents. Med Decis Making. 1989 Apr-Jun;9(2):142–149. doi: 10.1177/0272989X8900900209. [DOI] [PubMed] [Google Scholar]
- Miyamoto J. M., Eraker S. A. Parameter estimates for a QALY utility model. Med Decis Making. 1985 Summer;5(2):191–213. doi: 10.1177/0272989X8500500208. [DOI] [PubMed] [Google Scholar]
- Read J. L., Quinn R. J., Berwick D. M., Fineberg H. V., Weinstein M. C. Preferences for health outcomes. Comparison of assessment methods. Med Decis Making. 1984;4(3):315–329. doi: 10.1177/0272989X8400400307. [DOI] [PubMed] [Google Scholar]
- Rosser R., Kind P. A scale of valuations of states of illness: is there a social consensus? Int J Epidemiol. 1978 Dec;7(4):347–358. doi: 10.1093/ije/7.4.347. [DOI] [PubMed] [Google Scholar]
- Schag C. C., Heinrich R. L., Ganz P. A. Karnofsky performance status revisited: reliability, validity, and guidelines. J Clin Oncol. 1984 Mar;2(3):187–193. doi: 10.1200/JCO.1984.2.3.187. [DOI] [PubMed] [Google Scholar]
- Slevin M. L., Plant H., Lynch D., Drinkwater J., Gregory W. M. Who should measure quality of life, the doctor or the patient? Br J Cancer. 1988 Jan;57(1):109–112. doi: 10.1038/bjc.1988.20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stiggelbout A. M., Eijkemans M. J., Kiebert G. M., Kievit J., Leer J. W., De Haes H. J. The 'utility' of the visual analog scale in medical decision making and technology assessment. Is it an alternative to the time trade-off? Int J Technol Assess Health Care. 1996 Spring;12(2):291–298. doi: 10.1017/s0266462300009648. [DOI] [PubMed] [Google Scholar]
- Stiggelbout A. M., Kiebert G. M., Kievit J., Leer J. W., Stoter G., de Haes J. C. Utility assessment in cancer patients: adjustment of time tradeoff scores for the utility of life years and comparison with standard gamble scores. Med Decis Making. 1994 Jan-Mar;14(1):82–90. doi: 10.1177/0272989X9401400110. [DOI] [PubMed] [Google Scholar]
- Sutherland H. J., Dunn V., Boyd N. F. Measurement of values for states of health with linear analog scales. Med Decis Making. 1983;3(4):477–487. doi: 10.1177/0272989X8300300406. [DOI] [PubMed] [Google Scholar]
- Torrance G. W. Measurement of health state utilities for economic appraisal. J Health Econ. 1986 Mar;5(1):1–30. doi: 10.1016/0167-6296(86)90020-2. [DOI] [PubMed] [Google Scholar]
- Torrance G. W. Utility approach to measuring health-related quality of life. J Chronic Dis. 1987;40(6):593–603. doi: 10.1016/0021-9681(87)90019-1. [DOI] [PubMed] [Google Scholar]
- Tsevat J., Dawson N. V., Matchar D. B. Assessing quality of life and preferences in the seriously ill using utility theory. J Clin Epidemiol. 1990;43 (Suppl):73S–77S. doi: 10.1016/0895-4356(90)90224-d. [DOI] [PubMed] [Google Scholar]


