Abstract
Background
Attendance for routine asthma reviews is poor. A recent randomised controlled trial found that telephone consultations can cost-effectively and safely enhance asthma review rates; however, concerns have been expressed about the generalisability and implementation of the trial's findings.
Aim
To evaluate the effectiveness of a telephone option as part of a routine structured asthma review service.
Design of study
Phase IV controlled before-and-after implementation study.
Setting
A large UK general practice.
Method
Using existing administrative groups, all patients with active asthma (n = 1809) received one of three asthma review services: structured recall with a telephone-option for reviews versus structured recall with face-to-face-only reviews, or usual-care (to assess secular trends). Main outcome measures were: proportion of patients with active asthma reviewed within the previous 15 months (Quality and Outcomes Framework target), mode of review, enablement, morbidity, and costs to the practice.
Results
A routine asthma review was provided for 397/598 (66.4%) patients in the telephone-option group compared with 352/654 (53.8%) in the face-to-face-only review group: risk difference 12.6% (95% confidence interval [CI] = 7.2 to 17.9, P<0.001). The usual-care group achieved a review rate of 282/557 (50.6%). Morbidity was equivalent in the three groups; however, enablement (P = 0.03) and confidence (P = 0.007) in asthma management were greater in the telephone-option versus face-to-face-only group. The cost per review achieved by providing the telephone-option service was lower than the face-to-face-only service (£10.03 versus £12.74, mean difference £2.71; 95% CI = 1.92 to 3.50, P<0.001); usual-care costs were £11.85 per review achieved.
Conclusion
Routinely offering telephone reviews cost-effectively increased asthma review rates, enhancing patient enablement and confidence with management, with no detriment to asthma morbidity. Practices should consider a telephone option for their asthma review service.
Keywords: access to health care; asthma; clinical trials, phase IV; consultation; intervention studies; telephone
INTRODUCTION
Regular review of people with long-term disease is good clinical practice,1 and is recommended in asthma guidelines internationally.2 Despite significant morbidity,3 attendance for routine asthma reviews is poor: patients commonly judge that their asthma is ‘not serious enough’ to warrant attending an asthma clinic.4,5 Telephone consultations offer alternative access to routine asthma reviews, although a recent UK ruling decreed that the evidence base for this approach in asthma care was ‘insufficient’.6
The Medical Research Council defines a phased approach to evaluating complex interventions that parallels the sequential phases of drug development.7,8 Initial theoretical considerations and exploratory phases allow an intervention to be defined in preparation for the definitive randomised, controlled trial. The final implementation phase evaluates the ‘real world’ feasibility, effectiveness, and sustainability of the intervention.
A phase III randomised, controlled trial, showed that telephone consultations enable 26% more people with asthma to be reviewed, without any apparent clinical disadvantage or loss of patient satisfaction.9 Patients appreciated the convenience of telephone reviews,10 particularly when their asthma was not troublesome, and the shorter duration resulted in cost-efficiencies for primary care.11 Subsequent correspondence highlighted a number of outstanding questions, including the relevance of these findings to the two-thirds of people with asthma who did not agree to participate, and that randomly assigning the intervention ignored the influence of patient preferences.12
This article reports results of a phase IV implementation study7 which evaluated the inclusion of a telephone option as an integral part of a routine asthma review service. Clinically and organisationally important questions were addressed, including the uptake of telephone reviews by patients when offered the choice, the impact on review rates and asthma morbidity, and the cost to the practice of providing a telephone review service. The definitions and standards used in this study are derived from the general medical services (GMS) contract which governs primary care services in the UK.13
METHOD
Setting and participants
The Whitstable Medical Practice (31 000 registered patients, 16 partners, six asthma-trained nurses) operates in three groups from two sites. Two groups at Whitstable Health Centre serve similar populations, share administrative and nursing services, and historically achieve reviews for a similar proportion of people with asthma. The third group at Chestfield Medical Centre, which serves a population with substantially different characteristics, has a largely independent administrative and nursing service, and the proportion of people with asthma reviewed is historically higher. Asthma care was provided by five asthma-trained nurses across the two practice sites. Asthma clinics offered a range of appointment times throughout the week and these were supplemented with opportunistic arrangements to suit patient availability. All patients on the ‘active’ asthma register (defined as patients with a diagnosis of asthma and prescribed asthma medication in the previous year) were included.13
Baseline demographics, review rates in 2003, and data on smoking status and uptake of influenza vaccination were obtained from the practice database.
Randomisation
Two similar Whitstable Health Centre groups were randomised to compare an asthma review service including structured recall with a telephone option for reviews versus a control group providing structured recall with face-to-face-only reviews (Table 1). Allocation to the telephone option was decided by the toss of a coin. Because of the known demographic differences, the Chestfield Medical Centre group were allocated to maintain usual care, thereby allowing researchers to control for secular trends.
Table 1.
Characteristics of the three groups at baseline.
| Telephone option | Face-to-face only | Usual care | |
|---|---|---|---|
| List size, n | 10 342 | 10 916 | 8926 |
| On asthma register, n (%) | 994 (9.6) | 1190 (10.9) | 840 (9.4) |
| ‘Active’ asthma, n (%) | 554 (55.7) | 659 (55.4) | 515 (61.3) |
| Comorbid COPD diagnosis | 36 (6.5) | 56 (8.5) | 37 (7.2) |
| Female, n (%) | 309 (55.8) | 363 (55.1) | 285 (55.3) |
| Age, mean (SD) | 43.0 (24.8) | 42.3 (24.4) | 45.4 (24.1) |
| Reviewed in previous 15 months, n (%) | 133 (24.0) | 128 (19.4) | 187 (36.3) |
| Morbidity in the previous 12 months, n (%) | |||
| Acute attacks | 185 (33.4) | 211 (32.0) | 183 (35.5) |
| Oral steroid courses | 102 (18.4) | 103 (15.6) | 100 (19.4) |
| Out-of-hours calls | 20 (3.7) | 34 (5.2) | 32 (6.2) |
| Accident and emergency attendances | 7 (1.3) | 8 (1.2) | 6 (1.2) |
| Admissions | 9 (1.4) | 14 (2.1) | 12 (2.3) |
| Influenza vaccination (patients aged ≥16 years) Winter 2003, n (%) | 215/476 (45.2) | 230/512 (44.9) | 231/426 (54.2) |
| Smokers/smoking status recorded (patients aged ≥ 12 years), n (%) | 65/290 (22.4) | 77/324 (23.8) | 59/317 (18.6) |
COPD = chronic obstructive pulmonary disease. SD = standard deviation.
How this fits in
Despite being recommended in national and international asthma guidelines as good clinical practice, attendance for routine review of asthma is poor, although many patients have significant morbidity. In a randomised, controlled trial, telephone consultations enabled 26% more people with asthma to be reviewed without any apparent clinical disadvantage or loss of patient satisfaction; although, there are concerns about the generalisability and implementation of these trial findings into routine clinical care. This controlled implementation study confirms that routinely providing a telephone option for asthma reviews cost-effectively increases access to care, enhancing confidence in self-management without compromising asthma morbidity. While a fifth of patients chose a telephone review, offering a choice of mode of consultation does not increase patient-initiated appointments; however, it does enable clinicians to initiate reviews with patients who do not respond to review invitations. Practices should consider including a telephone option in their asthma review service.
Description of services for the three groups
During the 12-month study patients with active asthma were offered a review service according to the allocation of the group with which they were registered. Additions to and deletions from the active asthma register (for example, new diagnoses, changes in disease status, moves into and away from the practice, and deaths) were included in the allocated service provision of the group with which they were registered.
Telephone-option group
Structured recall
Patients with active asthma not reviewed in the previous year were identified from the practice computer database and sent three invitations (by post or as memos with repeat prescriptions) over the study period.
Review arrangements
Patients were invited to book an appointment for their choice of a telephone or face-to-face review. The nurse phoned patients requesting telephone consultations on the number provided at the pre-arranged time. In addition, patients who did not respond to the three invitations were phoned and reviewed opportunistically.
Face-to-face-only group
In this control arm, the same recall procedure was used as for the telephone-option group, but excluding the option of telephone reviews. No systematic attempt was made to phone non-attenders opportunistically.
Usual-care group
The usual-care control group maintained their well established asthma clinic, and existing procedures (for example, invitations are issued in response to clinical need), but no systematic recall was undertaken.
Group allocation and review content
These services comprised the routine asthma care provided by the five asthma-trained practice nurses throughout 2004. Clinicians could override allocation to meet individual clinical needs, and patients could arrange reviews according to their preference regardless of allocation (including the provision of telephone reviews in the face-to-face-only and usual-care group).
The content of the asthma reviews was in accordance with the clinical needs of the patient and was recorded using practice-agreed Read Codes on a computerised template including fields for recording morbidity (using the Royal College of Physicians' three questions14), current treatment, inhaler technique, provision of self-management education, and discussion of other conditions (specifically allergic rhinitis).
Outcome measures
Proportion reviewed
The primary outcome measure was the proportion of patients with active asthma who had received a dedicated asthma review within the previous 15 months.13 This was assessed by computer searches at the end of the study period.
Asthma morbidity and enablement
Researchers posted the following validated questionnaires, with two reminders, to patients with active asthma in the three groups at the end of the study year (excluding children aged less than 12 years, as the questionnaires are not validated for this age group). The only exclusion criteria were a predominant diagnosis of chronic obstructive pulmonary disease, inability to complete the questionnaire (for example, because of severe dementia), and patients excluded by their GP for significant medical or social reasons.
Mini-Asthma Quality-of-Life Questionnaire (mini-AQLQ) measures the physical/emotional impact of asthma on a scale from 1 (greatest impairment) to 7 (responsive to change),15 with a minimum important difference of 0.5.16 The questionnaire is validated for postal administration.17
Asthma Control Questionnaire (ACQ) measures the clinical goals of asthma management on a scale from 0 (good control) to 6 (responsive to change),18 with a minimum important difference of 0.5,19 and is validated for postal use.17
Modified Patient Enablement Instrument (mPEI) reflects enablement in asthma on a scale from 0 to 12.20,21 A difference of 0.8 is regarded as significant when used to assess the impact of a single consultation20 and an asthma self-management programme.21
Asthma Bother Profile: management section (ABPm) reflects quality of asthma care and patients' confidence in their ability to self-manage on a scale from 0 (no confidence) to 5 (full confidence).22
Researchers noted adverse occurrences, both clinical (for example, asthma deaths and near-fatal asthma attacks) and organisational (for example complaints related to the provision of care).
Mode of review, and cost to the practice of providing the service
Details of the consultation, including mode (booked telephone/opportunistic telephone/face-to-face), type of calls (local/long-distance/mobile), non-attenders or abortive calls, and duration of consultation were documented by the nurse at the conclusion of the review using the computerised template. Administrative staff logged the time and resources spent providing the recall service. Costs were estimated using unit costs from published UK sources.23,24
Training and quality control
Senior practice staff were involved in the design of the interventions, and standardised training was provided for all administrative and nursing staff. Quality control, undertaken by an independent organisation (Kent and Medway Primary Care Research Network) that was blinded to allocation, validated a random 5% sample of the data retrieved from records.
Sample size and statistical methods
Proportion reviewed
This was assessed on the whole practice population of ‘active asthmatics’ (approximately 550 in each group) giving 80% power, at the 5% level (two-tailed test) to detect a difference of 10% from 50% to 60%.9
A range of sample size estimates were conducted for questionnaire outcome measures (summarised below), and based on these, the target was to achieve completed responses from at least 200 patients in each group.
Equivalence in Mini-Asthma Quality-of-Life Questionnaire
Assuming a mean score of 5.14 (standard deviation [SD] 1.42),17 the study needed 134 responses in each group to demonstrate equivalence (defined as the ability to detect a difference of 0.5 points)16 with 80% power at the 5% level.
Difference in modified Patient Enablement Instrument
To show a difference in mean score of 0.8 (suggested as clinically important in patients with asthma)21 with 80% power and 95% confidence, responses were needed from 181 patients in each arm.
Analysis
The primary comparison was between the telephone-option and face-to-face-only groups. Categorical and continuous data were analysed on an intention-to-treat basis using SPSS (version 11.5). Normally distributed continuous data were compared using Student's t-test. Non-parametric data were compared using the Mann-Whitney U test. Categorical data were analysed using the χ2 test, and Fisher's exact test was used in the event of small numbers.
In addition, analysis at individual patient level was undertaken for those patients on the active asthma register of the practice throughout 2003 and 2004 (and, therefore, for whom a complete record of their review history was available). Multiple ordinal logistic regression was used to test the significance of the difference in proportion reviewed in 2004 between the face-to-face-only and telephone-option groups after adjusting for age, sex, and number of reviews in 2003.
Healthcare costs were calculated as means and compared with independent sample t-tests. The use of mean costs is recommended for economic evaluations of pragmatic trials because, despite the usual skewness in the distribution of cost data, the arithmetic mean is the most economically meaningful descriptive statistic.25 Standard t-tests and t-test-based confidence intervals (CIs) are adequate in most realistic situations for comparing mean costs.25 A sensitivity analysis was performed based on 95% CI of the recorded duration of the consultation.
RESULTS
Flow of patients through the study and baseline demographics
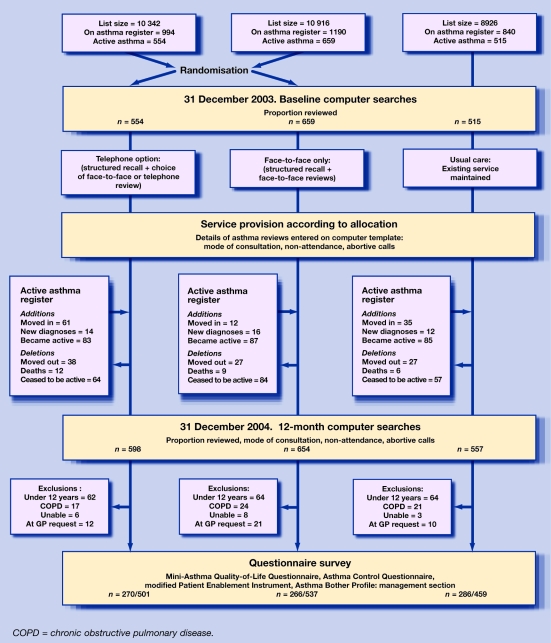
On 31 December 2003, from a practice list size of 30 184 patients, 3024 (10.0%) were on the asthma register, of whom 1728 (57.1%) were ‘actively’ receiving treatment. Baseline characteristics of the three groups are shown in Table 1. At the end of the study year, the list had increased to 31 239 patients: 3090 (9.9%) were on the asthma register of whom 1809 (58.5%) were active. The flow of patients through the study is shown in Figure 1. During the year, the number of eligible patients in the telephone-option group increased from 554 to 598, in the face-to-face-only group fell from 659 to 654, and in the usual-care group increased from 515 to 557.
Figure 1.
Flow of patients through the study.
Proportion reviewed and mode of review
A routine asthma review was provided for 397/598 (66.4%) of patients in the telephone-option group compared with 352/654 (53.8%) in the face-to-face-only group: χ2 = 20.52, P<0.001; risk difference 12.6% (95% CI = 7.2 to 17.9%); number needed to treat = 8.0. This represents increases of 42.4% in the telephone-option group and 34.4% in the face-to-face-only group over their respective baseline review rates. The usual-care group achieved a review rate of 282/557 (50.6%), an increase of 14.3% over their baseline rate.
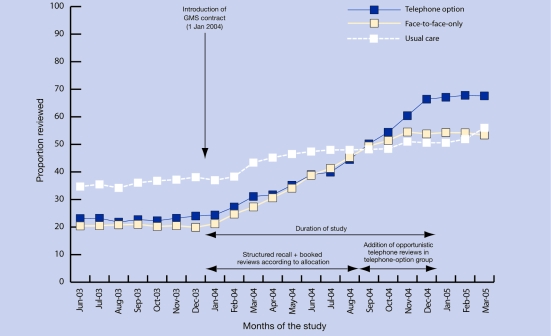
The mode of review was recorded in 977 (94.8%) of the 1031 patients who had a review (Table 2). A similar proportion of patients in each group initiated their consultation by booking an appointment, although a fifth of patients in the telephone-option group chose a telephone consultation. In addition, opportunistic telephone reviews were provided for 110/598 (18.4%) patients in the telephone-option group. Figure 2 illustrates the cumulative proportion of patients reviewed in the three groups on a monthly basis throughout the study.
Table 2.
Proportion reviewed and mode of consultation.
| Telephone option n = 598 | Face-to-face only n = 654 | Telephone option versus face-to-face only | Usual care n = 557 | Face-to-face only versus usual care | |
|---|---|---|---|---|---|
| P-value | P-value | ||||
| Number of patients reviewed, n (%) | 397 (66.4) | 352 (53.8) | <0.001 | 282 (50.6) | 0.27 |
| Mode of consultation | |||||
| Total patient-initiated booked reviews, n (%) | 276 (46.2) | 324 (49.5) | 0.23 | 256 (45.9) | 0.95 |
| Booked face-to-face, n (%) | 220 (79.7) | 316 (97.5) | 242 (94.5) | ||
| Booked telephone, n (%) | 56 (20.3) | 8 (2.5) | 14 (5.5) | ||
| Opportunistic telephone reviews, n (%) | 110 (18.4) | 6 (0.9) | 5 (0.9) | ||
| Additional reviews undertaken opportunistically during routine surgery consultations, n (%) | 38 (6.4) | 86 (13.1) | 61 (11.0) | ||
Figure 2.
Cumulative proportion of patients reviewed in the three groups on a monthly basis.
Analysis of individual patient data
Individual patient data for both 2003 and 2004 were available for 408/712 (57%) of the telephone-option group, and 523/774 (68%) of the face-to-face-only group. After adjusting for potential confounding factors (age, sex, and number of reviews in 2003), the difference in proportion reviewed in 2004 between the face-to-face-only and telephone-option groups remained significant at P<0.001. There was no significant difference between the groups in the total number of patient-initiated reviews after adjusting for other factors (P = 0.23).
Duration of review
Duration of consultation was recorded in 1211 (85.0%) of the 1424 reviews undertaken during the year in the three groups. Because telephone consultations were uncommon in the face-to-face-only and usual-care groups, the duration of consultation was calculated from data combined from the three groups. Face-to-face reviews were longer than booked telephone reviews (14.9 minutes [SD 2.9] versus 6.7 minutes [SD 2.5]: mean difference 8.1 minutes; 95%CI = 7.5 to 8.8; P<0.001). There was weak evidence that opportunistic telephone reviews were shorter than booked telephone reviews (6.7 minutes [SD 2.5] versus 5.9 minutes [SD 2.0]: mean difference 0.8 minutes; 95% CI = 0.14 to 1.42; P = 0.02).
Morbidity and enablement
Questionnaire responses were received from 822 (54.9%) of the 1497 patients aged 12 years and over. Response rate was greater in the usual-care group (286/459; 62.3%) compared with the telephone-option (270/501; 53.8%) and face-to-face-only (266/537; 49.5%) groups. The mini-AQLQ and ACQ scores were equivalent in the telephone-option and face-to-face-only groups; however, the mPEI and ABPm scores, which reflect enablement and confidence in asthma care and self-management were significantly greater in the telephone-option group (Table 3). The difference in the mPEI score exceeded the minimum clinically important difference of 0.8.20 There was no asthma-related adverse occurrence in any group during the course of the study.
Table 3.
Questionnaire responses
| Mean difference (95% CI) | P-value | Mean difference (95% CI) | P-value | ||||
|---|---|---|---|---|---|---|---|
| Telephone option n = 270 | Face-to-face only n = 266 | Telephone-option versus face-to-face-only | Telephone-option versus face-to-face-only | Usual care n = 286 | Face-to-face only versus usual care | Face-to-face only versus usual care | |
| Mini-AQLQ, meana (SD) | 5.29 (1.21) | 5.31 (1.24) | 0.02 (−0.21 to 0.24) | 0.87 | 5.27 (1.16) | 0.04 (−0.18 to 0.26) | 0.72 |
| ACQ, mean (SD) | 1.20 (1.00) | 1.33 (1.13) | 0.12 (−0.06 to 0.31) | 0.19 | 1.24 (0.97) | 0.09 (−0.09 to 0.27) | 0.32 |
| mPEI, mean (SD) | 7.29 (4.26) | 6.43 (4.30) | −0.83 (−1.56 to −0.10) | 0.03 | 6.90 (4.29) | −0.44 (−1.17 to 0.29) | 0.23 |
| ABPm, mean (SD) | 3.99 (0.84) | 3.78 (0.89) | −0.21 (−0.36 to −0.06) | 0.007 | 3.90 (0.88) | −0.12 (−0.27 to 0.04) | 0.14 |
There was no significant difference in any of the four domains of the miniAQLQ. AQLQ = Asthma Quality-of-Life Questionnaire. ACQ = Asthma Control Questionnaire. mPEI = modified Patient Enablement Instrument. ABPm = Asthma Bother Profile: management section.
Workload and costs to the practice of providing the service
The total workload involved in providing the service in each group includes not only reminders and consultations for patients on the active asthma register at the end of the study year, but also services provided for patients who subsequently moved from the practice, or whose asthma became ‘inactive’ during the year. A summary of workload and costs incurred by the practice to provide the services is given in Table 4 (see also Supplementary Tables 1–4). Cost per patient was similar in the telephone-option and face-to-face-only groups, but the cost per patient reviewed was significantly lower in the telephone-option group (telephone option: £10.03 [SD £5.53] versus face-to-face only: £12.74 [SD £5.68]: mean difference £2.71; 95% CI = 1.92 to 3.50; P<0.001).
Table 4.
Total workload and costs of providing the service.
| Telephone option | Face-to-face only | Usual care | |
|---|---|---|---|
| Total number of consultations, n | 509 | 485 | 430 |
| Face-to-face, n (%) | 324 (63.7) | 470 (97.1) | 406 (94.4) |
| Booked telephone, n (%) | 72 (14.1) | 9 (1.7) | 19 (4.4) |
| Opportunistic telephone, n (%) | 113 (22.2) | 6 (1.2) | 5 (1.2) |
| Missed appointments | 83/407 (20.4) | 104/574 (18.1) | 77/430 (17.9) |
| n (% of all face-to-face appointments booked) | |||
| Abortive telephone calls | 274/459 (59.7) | 10/25 (40.0) | 3/27 (11.0) |
| n (% of all telephone calls attempted) | |||
| Total invitations issued, n | 800 | 1068 | 16 |
| Letter, n | 727 | 937 | 15 |
| Memos with prescriptions, n | 73 | 131 | 1 |
| Total service costs, £ sterling | £3982.23 | £4485.50 | £3340.41 |
| Costs per ‘active asthmatic’, mean (SD) | £6.66 (5.30) | £6.86 (5.94) | £6.00 (6.76) |
| Costs per asthmatic reviewed, mean (SD) | £10.03 (5.33) | £12.74 (5.68) | £11.85 (6.45) |
Sensitivity analysis based on the 95% CI of the duration of the consultation confirmed the robustness of these data with costs savings per patient reviewed between £2.58 and £2.83 (Supplementary Table 3).
Offering a telephone option is a cost-effective method of providing reviews for those patients who respond to invitations, saving £1.43 per booked consultation provided. Opportunistic calls, while enabling an additional 110 (18.4%) patients to be reviewed, cost the practice £5.27 per consultation (Supplementary Table 4).
DISCUSSION
Summary of main findings
Including a telephone option as part of a routine review service for people with active asthma increased the proportion reviewed by 12.6% over a clinic-based service, largely because of opportunistic, clinician-initiated telephone calls to non-attenders. Asthma morbidity was similar in all three groups, but confidence in asthma care and self-management was greater in the telephone-option group. Telephone reviews were substantially shorter than face-to-face consultations, resulting in cost efficiencies for the practice.
Strengths and limitations of study
This study, of 12-months‘ duration, included every person with active asthma registered with the practice during 2004, including patients who joined or left the practice list during the year. Incorporating the service into normal practice activity enhanced generalisability. The inclusion of a third ‘usual-care’ group allowed the impact of secular trends, specifically the introduction of the new GMS contract,13 to be assessed. Morbidity data were obtained, using validated instruments, on a range of clinical outcome measures that were adequately powered.
This implementation study was carried out in one very large practice serving the residents of a small town in South East England encompassing a range of demographic profiles, although with no major areas of deprivation, potentially limiting generalisability. However, the important contribution that clinician-initiated opportunistic telephone calls can make to the proportion reviewed is likely to apply to most practices.
As recall of patients is predominantly an administrative function and the two intervention groups shared a common organisational and nursing structure, the study design did not allow for any clustering effects by individual GPs. However, prior to the introduction of the structured recall service, individual GPs' attitudes may have influenced patients' attendance for an asthma review and affected the review rate at baseline. This difference may account for some of the effect on the proportion reviewed; however, the improvement over baseline was 8.0% greater in the telephone-option group suggesting that these findings are robust. In addition, the difference remains significant in the individual patient level analysis (P<0.001) after controlling for age, sex, and number of reviews in the previous year.
Only two groups were randomised, so it is possible that other confounding factors could be responsible for these findings. For example, the larger number of new patients registering in the telephone-option group may have reduced the impact of the intervention. Differences in disease severity or patient profile may have influenced uptake of reviews, although demographics and asthma morbidity were similar in the two intervention groups at baseline.
Data recording was integrated into normal service delivery, raising the possibility that some data may have been omitted or incorrectly coded. However, use of a computer template and standardised training should have minimised such errors. Furthermore, a number of checks of accuracy were included (for example, nurses' estimate of consultation duration were compared with timings recorded by the computer appointment system). Discrepancies detected were minor and would not have altered the study's conclusions.
The nurses undertaking the reviews and recording data about the consultations were, of necessity, aware of allocation potentially introducing bias. However, quality control checks, blinded to allocation, confirmed accuracy of data transfer.
Comparison with existing literature
This phase IV implementation study7 echoes and extends findings of the previously published randomised, controlled trial9,11 by providing evidence that telephone asthma reviews can effectively contribute to asthma care. The effect size is approximately half that observed in the randomised trial, reflecting the challenge of providing care as part of the normal practice workload for a population of about 1800 people with asthma, with a 20% turnover during the study year. These findings emphasise the importance of the implementation phase in evaluating the impact of complex interventions to provide meaningful evidence for practices delivering routine care.
The present study coincided with the introduction of the UK GMS contract in January 2004 which rewards practices who achieve clinical standards, including a target of 70% for the annual review of people with ‘active’ asthma.13 The impact of this was seen in the usual-care group which increased the review rate by 14% without a structured recall service. Other models of service may be considered which reduce the need for routine reminder letters; for example: supplementing computer alerts for clinicians with opportunistic telephone calls to screen non-attenders, and offering face-to-face review to those with poor control.26
Despite the acknowledged convenience,10 offering a telephone option did not increase the proportion of patients who initiated a consultation by booking an appointment. A large UK survey observed that 45% of people with asthma neither had, nor wanted a regular asthma review, suggesting that this is a characteristic of asthma populations.5 Telephone consultations increased the proportion reviewed by providing an opportunity for clinicians to initiate the consultation. Under the terms of the GMS contract, practices may exclude patients from their target if they do not respond to three written invitations.13 These data suggest that providing an opportunistic telephone review is a practical and cost-effective option for enhancing access rather than accepting non-response as an exclusion criterion.27
About four-fifths of the patients in the telephone-option group who responded to the reminder letter chose to book a face-to-face consultation. The shorter duration of telephone reviews echoes previous findings,8 and may not only reflect the different dynamics of telephone consulting,28 but may also be the consequence of patients with milder, less troublesome asthma opting for the convenience of telephone reviews.10
This implementation study, while confirming equivalence of asthma control and quality of life, showed a significant difference in validated scores, which reflected confidence in the practice asthma care, in patients' self-management skills, and evidence of increased enablement. Routine reviews are provided for patients in the stable ‘maintenance’ phase of monitoring, during which self-monitoring assumes precedence.29 A key function of professional reviews is to support self-management, an effect that may be better reflected in enablement and confidence scores, rather than asthma control or quality of life.
Implications for clinical practice
Health service policy increasingly advocates respecting patient choice to improve access to healthcare; although telephone consultations are increasingly seen as a means of achieving this,30,31 the evidence base from controlled clinical studies in patients with long-term diseases remains relatively weak.32 This study strengthens the previous finding that offering telephone reviews increases the proportion of people with asthma reviewed with no detriment to asthma morbidity, and suggests benefit to patient enablement and confidence with asthma management.
Including a telephone option as part of a review service for people with asthma is a practical and cost-effective strategy for enhancing access, which has an impact on the recognised reluctance of people with asthma to respond to invitations for routine asthma reviews. These findings have direct clinical implications and also policy implications for those setting standards for the Quality and Outcomes Framework of the UK GMS contract.6,13
Supplementary Material
Acknowledgments
Partners, nursing, and administrative staff of the Whitstable Medical Practice and the people with asthma registered with the practice. Specifically, Christa Norman, Toni Bowey, and Paula Jones who helped with the study administration; Kathy Ellis, Bridget Hailwood, Lorna Doyle, and Doreen Kalideen who helped Caroline Snellgrove and Suzanne Gaskin undertake the asthma reviews, and helped with extracting data from records. Victoria Madden was the lay advisor to the study. Kirstie Coxon, Manager of the Kent and Medway Primary Care Research Network undertook a quality control check. Rob Elton provided statistical advice, and Chris Griffiths who commented on earlier drafts of the paper.
Supplementary information
Additional information accompanies this article at http://www.rcgp.org.uk/bjgp-suppinfo
Funding body
Scientific Foundation Board of the Royal College of General Practitioners (SFB/2003/45)
Ethics committee
The study was undertaken with approval from East Kent Local Research Ethics Committee (001/01/04) and governance approval from Canterbury and Coastal Primary Care Trust
Competing interests
The authors have stated that there are none
REFERENCES
- 1.General Medical Council. Good medical practice. 3rd edn. London: General Medical Council; 2001. [Google Scholar]
- 2.The British Thoracic Society: Scottish Intercollegiate Guideline Network. British guideline on the management of asthma. Thorax. 2003;58(Suppl 1):i1–94. doi: 10.1136/thorax.58.suppl_1.1i. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Haughney J, Barnes G, Partridge M, Cleland J. The Living & Breathing study: a study of patients' views of asthma and its treatment. Prim Care Respir J. 2004;(13)(1):28–35. doi: 10.1016/j.pcrj.2003.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gruffydd-Jones K, Nicholson I, Best L, Connell E. Asthma in general practice. Why don't patients attend the asthma clinic? Asthma Gen Pract. 1999;7:36–39. [Google Scholar]
- 5.Price D, Wolfe S. Delivery of asthma care: patient's use of and views on healthcare services, as determined from a nationwide interview survey. Asthma J. 2000;5:141–144. [Google Scholar]
- 6.Implementation Co-ordination Group. Joint statement from NHS Employers and the General Practitioners Committee about telephone reviews of asthma patients. London: British Medical Association; 2006. [Google Scholar]
- 7.Campbell M, Fitzpatrick R, Haines A, et al. Framework for design and evaluation of complex intervention to improve health. BMJ. 2000;321:694–696. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Campbell N, Murray E, Darbyshire J, et al. Designing and evaluating complex interventions to improve health care. BMJ. 2007;334:455–459. doi: 10.1136/bmj.39108.379965.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pinnock H, Bawden R, Proctor S, et al. Accessibility, acceptability and effectiveness of telephone reviews for asthma in primary care: randomised controlled trial. BMJ. 2003;326:477–479. doi: 10.1136/bmj.326.7387.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pinnock H, Snellgrove C, Madden V, Sheikh A. Telephone or surgery asthma reviews? Preferences of participants in a primary care randomised controlled trial. Prim Care Respir J. 2005;14:42–46. doi: 10.1016/j.pcrj.2004.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pinnock H, McKenzie L, Price D, Sheikh A. Cost effectiveness of telephone or surgery asthma reviews: health economic analysis of a pragmatic primary care randomised controlled trial. Br J Gen Pract. 2005;55:119–124. [PMC free article] [PubMed] [Google Scholar]
- 12.McKinstry B, Heaney D, Walker J, Wyke S. Routine telephone review of asthma: further investigation is required. BMJ. 2003;326:1267. doi: 10.1136/bmj.326.7401.1267-b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.NHS Confederation, British Medical Association. New GMS contract 2003: investing in general practice. London: BMA; 2003. [Google Scholar]
- 14.Pearson MG, Bucknall CE, editors. Measuring clinical outcome in asthma: a patient-focused approach. London: Royal College of Physicians; 1999. [Google Scholar]
- 15.Juniper EF, Guyatt GH, Cox FM, et al. Development and validation of the Mini Asthma Quality of Life Questionnaire. Eur Respir J. 1999;14:32–38. doi: 10.1034/j.1399-3003.1999.14a08.x. [DOI] [PubMed] [Google Scholar]
- 16.Juniper EF, Guyatt GH, Willan A, Griffith LE. Determining a minimal important change in a disease-specific quality of life questionnaire. J Clin Epidemiol. 1994;47:81–87. doi: 10.1016/0895-4356(94)90036-1. [DOI] [PubMed] [Google Scholar]
- 17.Pinnock H, Sheikh A, Juniper E. Concordance between supervised and postal administration of the MiniAQLQ and ACQ is very high. J Clin Epidemiol. 2005;58:809–814. doi: 10.1016/j.jclinepi.2005.01.010. [DOI] [PubMed] [Google Scholar]
- 18.Juniper EF, O'Byrne PM, Roberts JN. Measuring asthma control in group studies: do we need airway calibre and rescue beta2-agonist use? Resp Med. 2001;95:319–323. doi: 10.1053/rmed.2001.1034. [DOI] [PubMed] [Google Scholar]
- 19.Juniper EF, Ståhl E, O'Byrne PM. Minimal important difference for the asthma control questionnaire. Am J Respir Crit Care Med. 2001;163:A642. [Google Scholar]
- 20.Howie JGR, Heaney DJ, Maxwell M, Walker JJ. A comparison of patient enablement instrument against two established satisfaction scales as an outcome measure of primary care consultations. Fam Pract. 1998;15:165–171. doi: 10.1093/fampra/15.2.165. [DOI] [PubMed] [Google Scholar]
- 21.Price D, Haughney J, Rosen J-P, et al. Validation of a modified patient enablement instrument. Eur Respir J. 2003;22(S45):259s. [Google Scholar]
- 22.Hyland ME, Ley A, Fisher DW, Woodward V. Measurement of psychological distress in asthma and asthma management programmes. Br J Clin Psychology. 1995;34:601–611. doi: 10.1111/j.2044-8260.1995.tb01494.x. [DOI] [PubMed] [Google Scholar]
- 23.Netten A, Dennett J, Knight J. Unitcosts of health and social care 2004. University of Kent at Canterbury: Personal Social Services Research Unit; 2004. [Google Scholar]
- 24.British Telecom. Call charges for 2004. http://www.serviceview.bt.com/list/public/homepage.htm (accessed 8 Aug2007)
- 25.Thompson SG, Barber JA. How should cost data in pragmatic randomised trials be analysed? BMJ. 2000;320:1197–2000. doi: 10.1136/bmj.320.7243.1197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gruffydd-Jones K, Hollinghurst S, Ward S, Taylor G. Targeted routine asthma care in general practice using telephone triage. Br J Gen Pract. 2005;55:918–923. [PMC free article] [PubMed] [Google Scholar]
- 27.Fernando B, Pinnock H, Sheikh A. Telephone reviews of chronic illnesses. Br J Gen Pract. 2006;56:141. [PMC free article] [PubMed] [Google Scholar]
- 28.Innes M, Skelton J, Greenfield S. A profile of communication in primary care physician telephone consultations: application of the Roter Interaction Analysis System. Br J Gen Pract. 2006;56:363–368. [PMC free article] [PubMed] [Google Scholar]
- 29.Glasziou P, Irwig L, Mant D. Monitoring in chronic disease: a rational approach. BMJ. 2005;330:644–648. doi: 10.1136/bmj.330.7492.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Pinnock H, Hoskins G, Neville R, Sheikh A. Triage and remote consultations: moving beyond the rhetoric of access and choice. Br J Gen Pract. 2005;55:910–911. [PMC free article] [PubMed] [Google Scholar]
- 31.Department of Health. Building on the best: choice, responsiveness and equity in the NHS. London: Department of Health; 2003. [Google Scholar]
- 32.Car J, Sheikh A. Telephone consultations. BMJ. 2003;326:966–969. doi: 10.1136/bmj.326.7396.966. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.