Summary points
If patients with asymptomatic inguinal hernia are medically fit, they should be offered repair
Mesh repair is associated with the lowest recurrence rates of hernia
Laparoscopic repair is suggested for recurrent and bilateral inguinal hernias, though it may also be offered for primary inguinal hernia repair
The median absence from work after hernia repair is seven days and may be 14 days for those doing strenuous work
Early complications include bruising, numbness, and wound infection
Chronic pain is the predominant late complication
Abdominal wall hernias are common, with a prevalence of 1.7% for all ages and 4% for those aged over 45 years. Inguinal hernias account for 75% of abdominal wall hernias, with a lifetime risk of 27% in men and 3% in women.1 Repair of inguinal hernia is one of the most common operations in general surgery, with rates ranging from 10 per 100 000 of the population in the United Kingdom to 28 per 100 000 in the United States.2 In 2001-2 about 70 000 inguinal hernia repairs (62 969 primary, 4939 recurrent) were done in England, requiring more than 100 000 hospital bed days. Ninety five per cent of patients presenting to primary care are male, and in men the incidence rises from 11 per 10 000 person years aged 16-24 years to 200 per 10 000 person years aged 75 years or above.3
How do inguinal hernias present?
Inguinal hernias present with a lump in the groin that goes away with minimal pressure or when the patient is lying down. Most cause mild to moderate discomfort that increases with activity. A third of patients scheduled for surgery have no pain, and severe pain is uncommon (1.5% at rest and 10.2% on movement).4
Inguinal hernias are at risk of irreducibility or incarceration, which may result in strangulation and obstruction; however, unlike with femoral hernias, strangulation is rare. National statistics from England identified that 5% of repairs of primary inguinal hernia were emergency operations in 1998-9. Older age and longer duration of hernia and of irreducibility are risk factors for acute complications. Gallegos and colleagues studied the presentation of inguinal hernias with a “working diagnosis of strangulation.” Only 14 of their 22 patients with an acute hernia had compromised tissue at operation, with one of 439 patients requiring bowel resection.5 Though the study numbers are small, these findings emphasise the rarity of strangulation. A recent larger study estimated the lifetime risk of strangulation at 0.27% for an 18 year old man and 0.03% for a 72 year old man.6
How is an inguinal hernia assessed clinically?
A hernia is reducible if it occurs intermittently (such as on straining or standing) and can be pushed back into the abdominal cavity, and irreducible if it remains permanently outside the abdominal cavity. A reducible hernia is usually a longstanding condition, and diagnosis is made clinically, on the basis of typical symptoms and signs. The condition may be unilateral or bilateral and may recur after treatment (recurrent hernia).
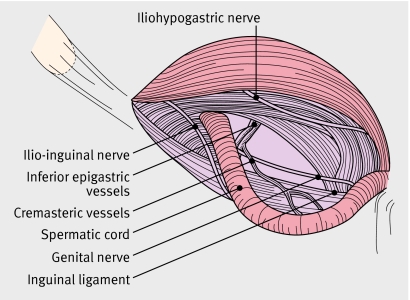
Inguinal hernias are often classified as direct or indirect, depending on whether the hernia sac bulges directly through the posterior wall of the inguinal canal (direct hernia) or passes through the internal inguinal ring alongside the spermatic cord, following the coursing of the inguinal canal (indirect hernia) (fig 1). However, there is no clinical merit in trying to differentiate between direct or indirect hernias. The box outlines important elements in examining patients who have a suspected inguinal hernia.
Fig 1 Anatomy of the inguinal canal
Examination of a patient with a suspected inguinal hernia
Examine the patient first when he or she is standing
Demonstrate lump with cough impulse
Then do an abdominal examination with the patient lying down
No merit in trying to differentiate between direct and indirect hernias
Important differential diagnoses: saphena varix; femoral hernia (may be difficult even for experienced clinicians); hydrocoele (differentiate from inguinoscrotal hernia—can get above a hydrocoele on examination)
How can an inguinal hernia be treated?
Surgical options for inguinal hernias
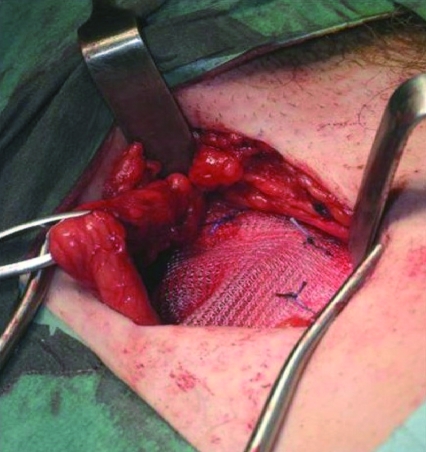
Surgery is the treatment of choice varying from a nylon darn, Shouldice layered, Lichtenstein mesh (fig 2) to a laparoscopic repair. The optimal repair has been assessed by randomised clinical trials and population based studies.
Fig 2 Open mesh repair of an inguinal hernia
Mesh or sutured repair?
A meta-analysis from the EU Hernia Trialists Collaboration compared mesh with sutured techniques from 58 trials comprising in total 11 174 patients.7 Individual patient data were available for 6901 patients. Recurrence was less common after mesh repair (odds ratio 0.43 (95% confidence interval 0.34 to 0.55)). A population based study examining risk of recurrence five years or more after primary mesh (Lichtenstein repair) and sutured inguinal hernia repair in 13 674 patients found that recurrence after mesh repair was a quarter of that after sutured repair (hazard ratio 0.25 (0.16 to 0.40)).8
Open mesh repair is reproducible by non-specialist surgeons, and hence open repair is the preferred repair technique for primary inguinal hernia (by 96% of UK surgeons, 99% of Japanese surgeons, 95% of Danish surgeons, and 86% of US surgeons.9
Open or laparoscopic repair?
Systematic review and meta-analysis of randomised clinical trials have found that, compared with open repair, laparoscopic surgery for hernia is associated with longer operation times but less severe postoperative pain, fewer complications, and a more rapid return to normal activities.10 11 Laparoscopic surgery is associated with higher recurrence rates during the learning curve12 but causes less chronic pain and numbness when assessed by questionnaire up to five years after operation.13 The National Institute for Health and Clinical Excellence (NICE) recently recommended laparoscopic surgery as a treatment option for inguinal hernia and said that patients should be fully informed of the risks and benefits of open and laparoscopic surgery to enable them to choose between procedures.14
Local, general, or regional anaesthesia?
A recent, Swedish, multicentre trial randomised patients to receive local infiltration anaesthesia, regional anaesthesia, or general anaesthesia for repair of inguinal hernia in non-specialist centres. The trial found a significant advantage with local infiltration anaesthesia, which was associated with a shorter hospital stay, less severe postoperative pain, and fewer micturition difficulties.15 Significantly reduced overall costs were found with local anaesthesia owing to shorter total time in theatre, earlier discharge, and equipment requirements.16
Other studies report similar results but with less pronounced differences. This may be the result of a lack of standardisation of general anaesthesia in the Swedish study.17 Many countries, however, still use general or regional anaesthesia for hernia repair, with a minority using local anaesthesia. A recent study in Denmark of 57 505 elective open groin (mainly inguinal) hernia operations found that 64% were via general anaesthetic, 18% regional anaesthetic, and 18% local anaesthetic.18 Regional anaesthesia gives the poorest results and probably has little role in modern inguinal hernia surgery. Poor uptake of local anaesthesia may relate to surgical tradition, surgeon preference, inadequate technical proficiency, and little incentive for cost effective techniques.
What to do with a hernia with minimal or no symptoms
A third of patients have minimal or no symptoms, and, as strangulation is uncommon, whether such hernias should be repaired is unclear. To try to clarify this, two recent randomised trials (from the US and the UK) have compared surgery with observation.19 20 The primary outcome in both studies was pain, as allowing chronic pain in previously asymptomatic patients would be unacceptable. At one and two years (US and UK respectively), no difference between groups existed in either trial. However, in the UK study, patients in the observation group were more likely to cross over to surgery because of pain or discomfort. The likely explanation is that many patients (40%) in the US study had a small inguinal hernia palpable on impulse only. Continued follow-up in both studies should determine whether observation delays rather than prevents surgery. In the meantime we recommend that all medically fit patients with an inguinal hernia should have it repaired.
Is there a role for a hernia truss?
The use of a truss to manage an inguinal hernia has been present from ancient times. The truss has been popular in the UK in the era of long waiting times for surgery; however, it is difficult for the patients to manage and cannot be recommended as a definitive form of treatment.1
What is the recovery period after inguinal hernia surgery?
Convalescence is of socioeconomic importance. Single centre studies suggest that for most repairs five to eight days should be adequate, although studies are difficult to integrate owing to different definitions of convalescence. Recently Bay-Nielsen and colleagues examined convalescence after Lichtenstein repair in a case-control study using data from the Danish hernia database.21 The median length of absence from work was seven days (sedentary work 4.5 days, strenuous work 14 days). The study found that a single day of convalescence was feasible without increasing recurrences. Pain was the most common cause of a delay in returning to work (60%), followed by wound problems (20%).
What can go wrong after inguinal hernia surgery?
Early complications
Death
For elective hernia repair, the mortality rate is lower than or similar to the population standardised mortality rate. Bay-Nielsen and colleagues published results from the prospective Danish hernia database of 26 304 hernia repairs. Four per cent of all groin hernia repairs were emergencies. A 30 day mortality rate of 0.02% in patients aged under 60 years and 0.48% in those aged 60 years and over was observed after elective surgery.22 Acute surgery had a 7% mortality rate, similar to the rate on the Swedish hernia register23; the data from the Scottish Audit of Surgical Mortality give an overall mortality rate of 0.2% for inguinal hernia repair, with most deaths in the elderly population with an ASA (American Association of Anaesthesiologists) grade of three and above.24
Wound complications and surgical site infections
Bruising and haematoma are common after hernia repair, and wound infection rates vary between 1% and 7%. Recent meta-analyses from a Cochrane review and from another review suggest that prophylactic antibiotics do not reduce the rate of surgical site infections.25 26 In the Cochrane Review, three of the eight randomised controlled trials used prosthetic material, whereas the remaining studies did not. No difference in the rate of surgical site infections between groups was identified; subgroup analysis, however, showed that in mesh repair a protective effect might exist, but the sample size was inadequate.
Late complications
Hernia recurrence
Large cohort studies from specialist centres find very low recurrence rates after open mesh repair, and a meta-analysis of randomised clinical trials has found lower recurrence rates with mesh repair.8 Butters and colleagues recently reported the long term follow-up of a trial comparing three techniques (the Shouldice, Lichtenstein, and transabdominal pre-peritoneal techniques) in a single German institution.27 Recurrence rates were higher in the Shouldice arm of the study, with equally low rates in the other two arms. Population based studies also confirm reduced recurrences with mesh repair; these studies use reoperation rates as surrogate markers for recurrence, however, and so may underestimate true recurrences. Thirty per cent to 50% of patients with a recurrent hernia will either be unaware of a recurrence or will not wish to have another repair.
Chronic pain
Chronic pain is pain that persists or occurs after normal tissue healing has taken place and can reasonably be defined as pain persisting three months after inguinal hernia repair. About 30% of patients when asked, or on completion of a confidential questionnaire, report long term pain or discomfort at the hernia repair site. When asked at the clinic, 10% report pain that is usually mild but may be moderate to severe in 3% of patients, interfering with work and leisure activities.28
Chronic pain is the most serious long term complication of hernia repair and may persist for several years. The cause of the pain is poorly understood and is more likely in younger patients who have been in severe pain from their hernia in the first instance. Regression analysis from population based studies identified four factors as independent predictors of chronic pain: a high level of pain preoperatively; age; an anterior surgical approach; and a postoperative complication.29 30
Patients are best treated by referral to a pain clinic, where a multidisciplinary approach can be instigated. Surgical exploration with nerve excision and mesh removal is reserved for those in whom medical treatment fails.
Infertility
Infertility incidence after inguinal hernia repair is higher than in the general population. Injury to the vas deferens at the time of surgery is estimated to be 0.3% for adults and 0.8-2.0% for children.31 Injury to the testis leading to atrophy may occur in 0.5% of primary hernia repairs, with a 10-fold increase for recurrent repairs.31. Hence a reduction in recurrences using mesh repair may reduce testicular loss and infertility.
Future directions
Chronic pain is the most common and serious long term problem after repair of an inguinal hernia. Many questions remain unanswered in this area. These include the effect of the repair on sexual function/dysejaculation; the identification of preoperative risk factors that may reliably predict chronic pain; whether intraoperative events such as nerve handling or unintentional nerve injury contribute; and whether other aspects of surgical technique (such as mesh-type or fixation technique) are implicated.
Additional educational resources
For patients
BestTreatments (www.besttreatments.co.uk)—Information based on the latest research evidence, including inguinal hernias.
For doctors
PatientUK (www.patient.co.uk/showdoc/40000295/)—Information on inguinal hernias
WeBSurg (www.websurg.com)—Collection of educational programmes in laparoscopic surgery, including inguinal hernia repair
Sources and selection criteria
We used several databases to identify studies for this review (Medline (1966 to September 2006); Embase (1980 to September 2006); the Cochrane Library), and we searched the websites of the NHS Centre for Reviews and Dissemination; Database of Abstracts of Reviews of Effects; Health Technology Assessment; the National Institute for Health and Clinical Excellence (for clinical guidelines); and of national hernia databases. We searched for information on the symptoms, complications, and treatment of inguinal hernia. In addition, we used PJOD’s extensive understanding and experience of hernia surgery and research.
Contributors: JTJ did the literature search. Both authors wrote the review.
Competing interests: None declared.
Provenance and peer review: Commissioned; externally peer reviewed.
References
- 1.Kingsnorth A, LeBlanc K. Hernias: inguinal and incisional. Lancet 2003;362:1561-71. [DOI] [PubMed] [Google Scholar]
- 2.Devlin HB. Trends in hernia surgery in the land of Astley Cooper. In: Soper NJ, ed. Problems in general surgery Vol 12. Philadelphia, PA: Lippincott-Raven, 1995:85-92.
- 3.Chow A, Purkayastha S, Athanasiou T, Tekkis P, Darzi A. Inguinal hernia. BMJ Clin Evid 2007;4:1-20. [PMC free article] [PubMed] [Google Scholar]
- 4.Page B, Paterson C, Young D, O’Dwyer PJ. Pain from primary inguinal hernia and the effect of repair on pain. Br J Surg 2002;89:1315-8. [DOI] [PubMed] [Google Scholar]
- 5.Gallegos NC, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg 1991;78:1171-3. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgibbons Jr RJ, Jonasson O, Gibbs J, Dunlop DD, Henderson W, Reda D, et al. The development of a clinical trial to determine if watchful waiting is an acceptable alternative to routine herniorraphy for patients with minimal or no hernia symptoms. J Am Coll Surg 2003;196:737-42. [DOI] [PubMed] [Google Scholar]
- 7.EU Hernia Trialists Collaboration. Repair of groin hernia with synthetic mesh, meta-analysis of randomized controlled trials. Ann Surg 2002;235:322-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bisgaard T, Bay-Nielsen M, Christensen IJ, Kehlet H. Risk of recurrence 5 years or more after primary Lichtenstein mesh and sutured inguinal hernia repair. Br J Surg 2007;94:1038-40. [DOI] [PubMed] [Google Scholar]
- 9.Kingsnorth A. Controversial topics in surgery: the case for open repair. Ann R Coll Surg Engl 2005;87:59-60. [PMC free article] [PubMed] [Google Scholar]
- 10.EU Hernia Trialists Collaboration. Laparoscopic compared with open methods of groin hernia repair: systematic review of randomised controlled trials. Br J Surg 2000;37:860-7. [DOI] [PubMed] [Google Scholar]
- 11.Memon MA, Cooper NJ, Memon B, Memon MI, Abrams KR. Meta-analysis of randomised clinical trials comparing open and laparoscopic inguinal hernia repair. Br J Surg 2003;90:1479-2. [DOI] [PubMed] [Google Scholar]
- 12.Neumayer L, Giobbie-Hurder A, Jonasson O, Fitzgibbons R Jr, Dunlop D, Gibbs J, et al. Open versus laparoscopic mesh repair of inguinal hernia. N Engl J Med 2004;350:1819-27. [DOI] [PubMed] [Google Scholar]
- 13.Grant AM, Scott NW, O’Dwyer PJ, for the MRC Laparoscopic Hernia Trial Group. Pain and numbness after laparoscopic and open repair of a groin hernia: five year follow-up of a randomized trial. Br J Surg 2005;91:1570-4. [DOI] [PubMed] [Google Scholar]
- 14.National Institute for Health and Clinical Excellence. Laparoscopic surgery for inguinal hernia repair. 2004. www.nice.org.uk/guidance/index.jsp?action=download&o=32924
- 15.Nordin P, Zetterstrom H, Gunnarsson U, Nilsson E. Local, regional or general anaesthesia in groin hernia repair: multicentre randomised trial. Lancet 2003;362:853-8. [DOI] [PubMed] [Google Scholar]
- 16.Nordin P, Zetterstrom H, Carlsson P, Nilsson E. Cost-effectiveness analysis of local, regional and general anaesthesia for inguinal hernia repair using data from a randomised trial. Br J Surg 2007;94:500-5. [DOI] [PubMed] [Google Scholar]
- 17.O’Dwyer PJ, Serpell MG, Millar K, Paterson C, Young D, Hair A, et al. Local or General anaesthesia for open hernia repair: a randomized trial. Annals of Surgery 2003;237:574-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kehlet H, Bay-Nielsen M. Anaesthetic practice for groin hernia repair—a nation-wide study in Denmark 1998-2003. Acta Anaesthesiol Scand 2005;49:143-6. [DOI] [PubMed] [Google Scholar]
- 19.Fitzgibbons RJ, Giobbie-Hurder A, Gibbs JO, Dunlop DD, Reda DJ, McCarthy M Jr, et al. Watchful waiting vs repair of inguinal hernia in minimally symptomatic men: a randomised clinical trial. JAMA 2006;295:285-92. [DOI] [PubMed] [Google Scholar]
- 20.O’Dwyer PJ, Norrie J, Alani A, Walker A, Duffy F, Horgan P. Observation or operation for patients with an asymptomatic inguinal hernia. Ann Surg 2006;244:167-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bay-Nielsen M, Thomsen H, Heidemann Andersen F, Bendix JH, Sørensen OK, Skovgaard N, et al. Convalescence after inguinal herniorraphy. Br J Surg 2004;91:362-7. [DOI] [PubMed] [Google Scholar]
- 22.Bay-Nielsen M, Kehlet H, Strand L, Malmstrøm J, Andersen FH, Wara P, et al. Quality assessment of 26 304 herniorrhaphies in Denmark: a prospective nationwide study. Lancet 2001;358:1124-8. [DOI] [PubMed] [Google Scholar]
- 23.Haapaniemi S, Sandblom G, Nilsson E. Mortality after elective and emergency surgery for inguinal and femoral hernia. Hernia 1999;4:205-8. [Google Scholar]
- 24.McGugan E, Burton H, Nixon SJ, Thompson AM. Deaths following hernia surgery: room for improvement. J R Coll Surg Edinb 2000;45:183-6. [PubMed] [Google Scholar]
- 25.Sanchez-Manuel FJ, Seco-Gil JL. Antibiotic prophylaxis for hernia repair. Cochrane Database Syst Rev 2004;(4):CD003769. [DOI] [PubMed] [Google Scholar]
- 26.Aufenacker TJ, Koelemay MJW, Gouma DJ, Simons MP. Systematic review and meta-analysis of the effectiveness of antibiotic prophylaxis in prevention of wound infection after mesh repair of abdominal wall hernia. Br J Surg 2006;93:5-10. [DOI] [PubMed] [Google Scholar]
- 27.Butters M, Redecke J, Koninger J. Long-term results of a randomised clinical trial of Shouldice, Lichtenstein and transabdominal preperitoneal repairs. Br J Surg 2007;94:562-5. [DOI] [PubMed] [Google Scholar]
- 28.Berndsen FH, Peterson V, Arvidsson D, Leijonmarck C-E, Rudberg C, Smedberg S, et al. Discomfort five years after laparoscopic and Shouldice inguinal hernia repair: a report from the SMIL Study Group. Hernia 2007;11:307-13. [DOI] [PubMed] [Google Scholar]
- 29.Franneby U, Sandblom G, Nordin P, Nyren O, Gunnarsson U. Risk factors for long-term pain after hernia surgery. Ann Surg 2006;244:212-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bay-Nielsen M, Perkins FM, Kehlet H. Pain and functional impairment 1 year after inguinal herniorraphy: a nationwide questionnaire study. Ann Surg 2001;233:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fitzgibbons Jr RJ. Can we be sure that polypropylene mesh causes infertility? Ann Surg 2005;241:559-61. [DOI] [PMC free article] [PubMed] [Google Scholar]