Abstract
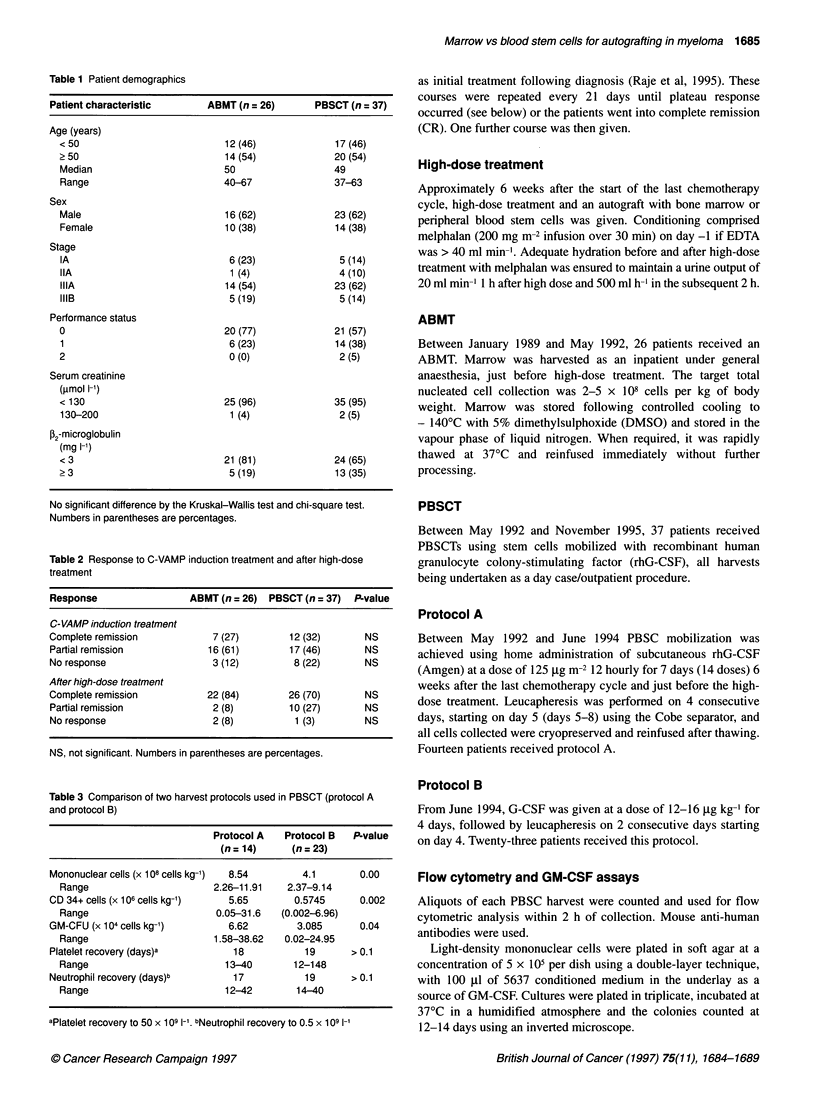
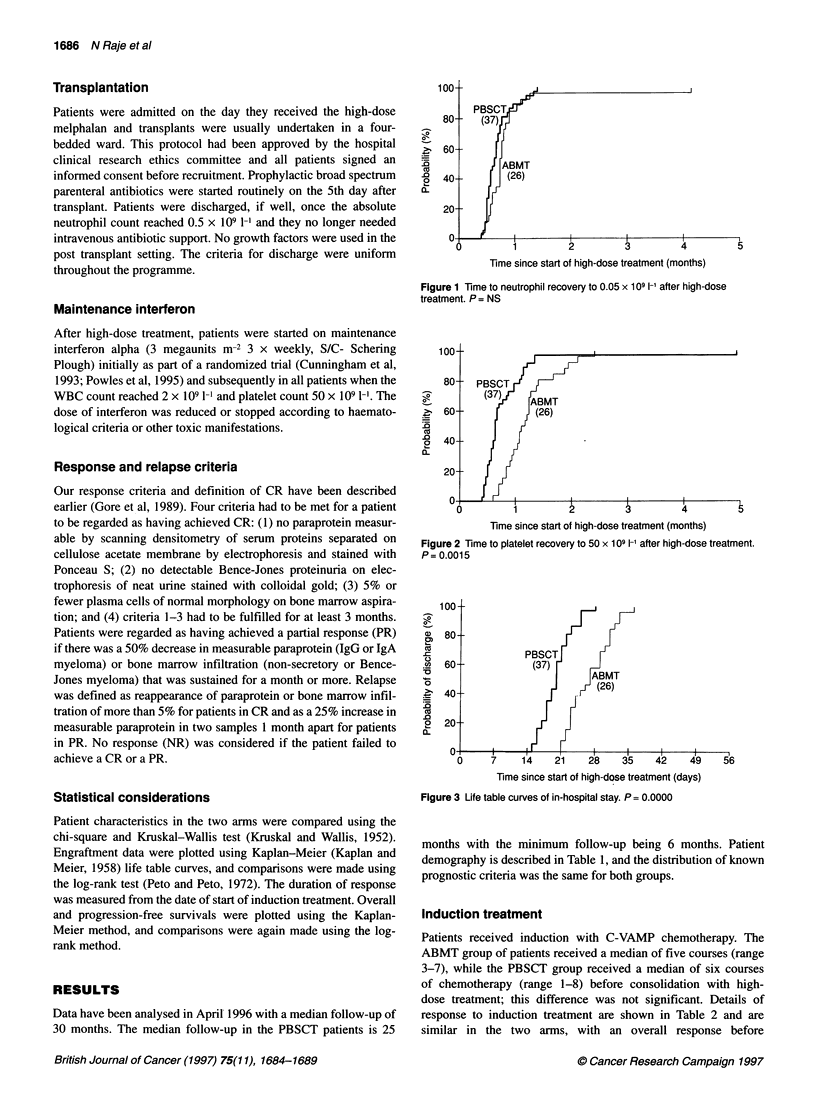
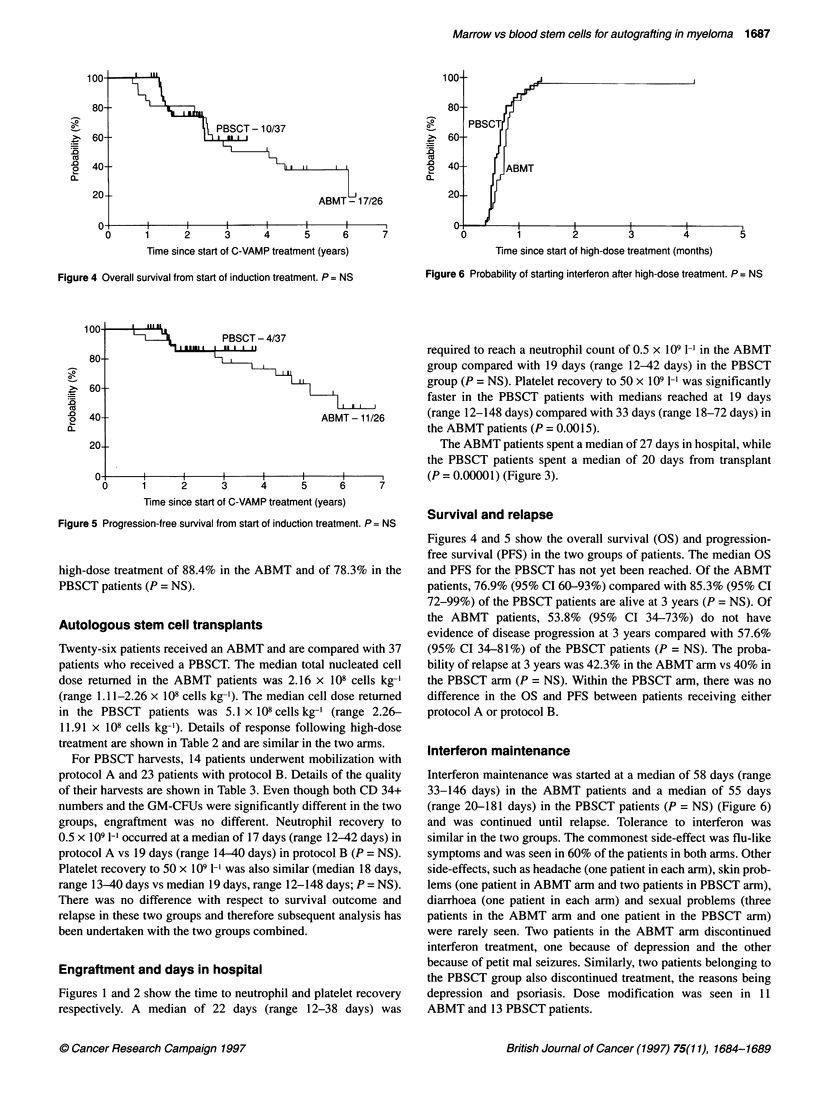
Sixty-three new untreated patients with multiple myeloma under the age of 70 years received C-VAMP induction treatment followed by high-dose intravenous melphalan (200 mg m(-2)) and autologous stem cell transplant, either with marrow [autologous bone marrow transplants (ABMT), n = 26] or with granulocyte colony-stimulating factor (G-CSF)-mobilized stem cells from the blood [peripheral blood stem cell transplants (PBSCT), n = 37]. This was a sequential study and the two groups were not significantly different for all known prognostic variables. The complete remission (CR) rate after high-dose treatment was the same for both groups [ABMT 84% and PBSCT 70%; P = not significant (NS)]. Neutrophil recovery to 0.5 x 10(9) l(-1) occurred at a median of 22 days in the ABMT patients compared with 19 days for the PBSCT patients (P = NS). Platelet recovery to 50 x 10(9) l(-1) was significantly faster in PBSCT patients (19 days vs 33 days; P = 0.0015), and the PBSCT patients spent fewer days in hospital (median 20 vs 27 days; P = 0.00001). There was no difference in the two groups with respect to starting interferon (58 days for ABMT vs 55 days for PBSCT), and tolerance to interferon was identical. The median overall survival (OS) and progression-free survival (PFS) for the PBSCT patients has not yet been reached. The OS in the ABMT patients at 3 years was 76.9% (95% CI 60-93%) compared with 85.3% (95% CI 72-99%) in the PBSCT patients (P = NS), and the PFS at 3 years in the ABMT patients was 53.8% (95% CI 34-73%) and in the PBSCT patients was 57.6% (95% CI 34-81%) (P = NS). The probability of relapse at 3 years was 42.3% in the ABMT arm compared with 40% in the PBSCT patients (P = NS). Thus, PBSCT patients had a faster engraftment and a shorter stay in hospital than ABMT; the survival outcome and probability of relapse was the same for both groups.
Full text
PDF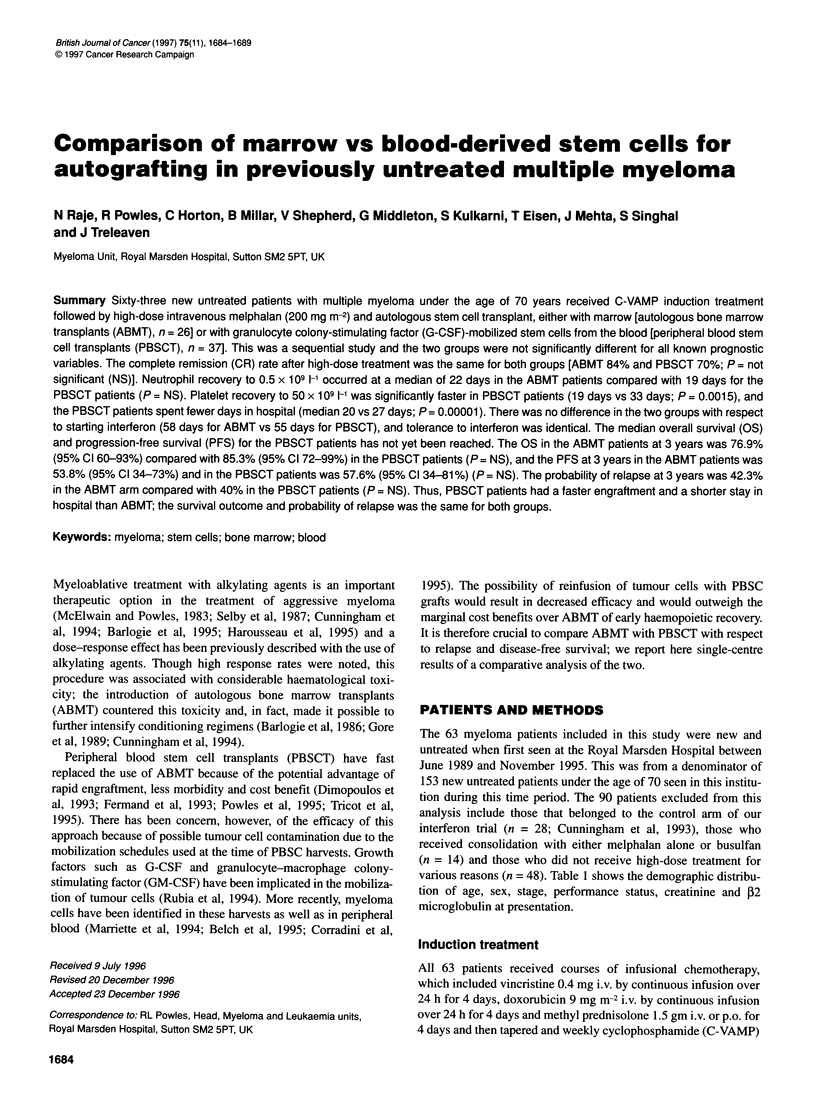

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Barlogie B., Hall R., Zander A., Dicke K., Alexanian R. High-dose melphalan with autologous bone marrow transplantation for multiple myeloma. Blood. 1986 May;67(5):1298–1301. [PubMed] [Google Scholar]
- Bensinger W. I., Longin K., Appelbaum F., Rowley S., Weaver C., Lilleby K., Gooley T., Lynch M., Higano T., Klarnet J. Peripheral blood stem cells (PBSCs) collected after recombinant granulocyte colony stimulating factor (rhG-CSF): an analysis of factors correlating with the tempo of engraftment after transplantation. Br J Haematol. 1994 Aug;87(4):825–831. doi: 10.1111/j.1365-2141.1994.tb06744.x. [DOI] [PubMed] [Google Scholar]
- Corradini P., Voena C., Astolfi M., Ladetto M., Tarella C., Boccadoro M., Pileri A. High-dose sequential chemoradiotherapy in multiple myeloma: residual tumor cells are detectable in bone marrow and peripheral blood cell harvests and after autografting. Blood. 1995 Mar 15;85(6):1596–1602. [PubMed] [Google Scholar]
- Cunningham D., Paz-Ares L., Milan S., Powles R., Nicolson M., Hickish T., Selby P., Treleavan J., Viner C., Malpas J. High-dose melphalan and autologous bone marrow transplantation as consolidation in previously untreated myeloma. J Clin Oncol. 1994 Apr;12(4):759–763. doi: 10.1200/JCO.1994.12.4.759. [DOI] [PubMed] [Google Scholar]
- Demirer T., Buckner C. D., Gooley T., Appelbaum F. R., Rowley S., Chauncey T., Lilleby K., Storb R., Bensinger W. I. Factors influencing collection of peripheral blood stem cells in patients with multiple myeloma. Bone Marrow Transplant. 1996 Jun;17(6):937–941. [PubMed] [Google Scholar]
- Dimopoulos M. A., Alexanian R., Przepiorka D., Hester J., Andersson B., Giralt S., Mehra R., van Besien K., Delasalle K. B., Reading C. Thiotepa, busulfan, and cyclophosphamide: a new preparative regimen for autologous marrow or blood stem cell transplantation in high-risk multiple myeloma. Blood. 1993 Oct 15;82(8):2324–2328. [PubMed] [Google Scholar]
- Dunbar C. E., Cottler-Fox M., O'Shaughnessy J. A., Doren S., Carter C., Berenson R., Brown S., Moen R. C., Greenblatt J., Stewart F. M. Retrovirally marked CD34-enriched peripheral blood and bone marrow cells contribute to long-term engraftment after autologous transplantation. Blood. 1995 Jun 1;85(11):3048–3057. [PubMed] [Google Scholar]
- Fermand J. P., Chevret S., Ravaud P., Divine M., Leblond V., Dreyfus F., Mariette X., Brouet J. C. High-dose chemoradiotherapy and autologous blood stem cell transplantation in multiple myeloma: results of a phase II trial involving 63 patients. Blood. 1993 Oct 1;82(7):2005–2009. [PubMed] [Google Scholar]
- Gazitt Y., Reading C. C., Hoffman R., Wickrema A., Vesole D. H., Jagannath S., Condino J., Lee B., Barlogie B., Tricot G. Purified CD34+ Lin- Thy+ stem cells do not contain clonal myeloma cells. Blood. 1995 Jul 1;86(1):381–389. [PubMed] [Google Scholar]
- Gore M. E., Selby P. J., Viner C., Clark P. I., Meldrum M., Millar B., Bell J., Maitland J. A., Milan S., Judson I. R. Intensive treatment of multiple myeloma and criteria for complete remission. Lancet. 1989 Oct 14;2(8668):879–882. doi: 10.1016/s0140-6736(89)91548-1. [DOI] [PubMed] [Google Scholar]
- Mariette X., Fermand J. P., Brouet J. C. Myeloma cell contamination of peripheral blood stem cell grafts in patients with multiple myeloma treated by high-dose therapy. Bone Marrow Transplant. 1994 Jul;14(1):47–50. [PubMed] [Google Scholar]
- McElwain T. J., Powles R. L. High-dose intravenous melphalan for plasma-cell leukaemia and myeloma. Lancet. 1983 Oct 8;2(8354):822–824. doi: 10.1016/s0140-6736(83)90739-0. [DOI] [PubMed] [Google Scholar]
- Powles R., Raje N., Cunningham D., Malpas J., Milan S., Horton C., Mehta J., Singhal S., Viner C., Treleaven J. Maintenance therapy for remission in myeloma with Intron A following high-dose melphalan and either an autologous bone marrow transplantation or peripheral stem cell rescue. Stem Cells. 1995 Aug;13 (Suppl 2):114–117. [PubMed] [Google Scholar]
- Powles R., Raje N., Horton C., Mehta J., Singhal S., Hickish T., Viner C., Milan S., Treleaven J., Cunningham D. Comparison of interferon tolerance after autologous bone marrow or peripheral blood stem cell transplants for myeloma patients who have responded to induction therapy. Leuk Lymphoma. 1996 May;21(5-6):421–427. doi: 10.3109/10428199609093439. [DOI] [PubMed] [Google Scholar]
- Schiller G., Vescio R., Freytes C., Spitzer G., Sahebi F., Lee M., Wu C. H., Cao J., Lee J. C., Hong C. H. Transplantation of CD34+ peripheral blood progenitor cells after high-dose chemotherapy for patients with advanced multiple myeloma. Blood. 1995 Jul 1;86(1):390–397. [PubMed] [Google Scholar]
- Selby P. J., McElwain T. J., Nandi A. C., Perren T. J., Powles R. L., Tillyer C. R., Osborne R. J., Slevin M. L., Malpas J. S. Multiple myeloma treated with high dose intravenous melphalan. Br J Haematol. 1987 May;66(1):55–62. doi: 10.1111/j.1365-2141.1987.tb06890.x. [DOI] [PubMed] [Google Scholar]
- Singhal S., Powles R., Milan S., Raje N., Viner C., Treleaven J., Raymond J., Cunningham D., Mehta J. Kinetics of paraprotein clearance after autografting for multiple myeloma. Bone Marrow Transplant. 1995 Oct;16(4):537–540. [PubMed] [Google Scholar]
- Tricot G., Jagannath S., Vesole D., Nelson J., Tindle S., Miller L., Cheson B., Crowley J., Barlogie B. Peripheral blood stem cell transplants for multiple myeloma: identification of favorable variables for rapid engraftment in 225 patients. Blood. 1995 Jan 15;85(2):588–596. [PubMed] [Google Scholar]
- de la Rubia J., Bonanad S., Palau J., Sanz G. F., Sanz M. A. Rapid progression of multiple myeloma following G-CSF mobilization. Bone Marrow Transplant. 1994 Sep;14(3):475–476. [PubMed] [Google Scholar]


