Abstract
Hantavirus pulmonary syndrome (HPS) is a rapidly progressing human disease with one of the highest case fatality rates (30 to 50%) of any acute viral disease known. There are no vaccines, effective antiviral drugs, or immunologics to prevent or treat HPS. In an attempt to develop HPS medical countermeasures, we constructed an expression plasmid, pWRG/AND-M, that contains the full-length M genome segment of Andes virus (ANDV), a South American hantavirus. Transfection experiments in cell culture indicated that both the G1 and G2 glycoproteins are expressed from pWRG/AND-M. Rhesus macaques vaccinated by gene gun with pWRG/AND-M developed remarkably high levels of neutralizing antibodies that not only neutralized ANDV but also cross-neutralized other HPS-associated hantaviruses, including Sin Nombre virus. To determine if the antibodies elicited in the monkeys could confer protection, we performed a series of passive-transfer experiments using a recently described lethal HPS animal model (i.e., adult Syrian hamsters develop HPS and die within 10 to 15 days after challenge with ANDV). When injected into hamsters 1 day before challenge, sera from the vaccinated monkeys either provided sterile protection or delayed the onset of HPS and death. When injected on day 4 or 5 after challenge, the monkey sera protected 100% of the hamsters from lethal disease. These data provide a proof of concept for a gene-based HPS vaccine and also demonstrate the potential value of a postexposure immunoprophylactic to treat individuals after exposure, or potential exposure, to these highly lethal hantaviruses.
Hantaviruses are rodent-borne, enveloped RNA viruses in the family Bunyaviridae. These viruses have a trisegmented, negative-sense, single-stranded RNA genome. The three gene segments, L, S, and M, encode the RNA polymerase, nucleoprotein, and envelope glycoproteins (G1 and G2), respectively (27). Hantaviruses cause a spectrum of vascular-leak syndromes in humans ranging from proteinuria and petechia to pulmonary edema and frank hemorrhage (20, 21). New World hantaviruses have been associated with a highly lethal disease, hantavirus pulmonary syndrome (HPS), that is characterized by fever and vascular leakage, resulting in noncardiogenic pulmonary edema followed by shock. Case fatality rates for HPS caused by the most prevalent North American and South American hantaviruses, Sin Nombre virus (SNV) and Andes virus (ANDV), are 30 to 50%. Old World hantaviruses have been associated with a mild-to-severe disease, hemorrhagic fever with renal syndrome (HFRS), that is characterized by fever, vascular leakage resulting in hemorrhagic manifestations, and renal failure. The case fatality rate for HFRS ranges from <0.1% to 15%. The four Old World hantaviruses associated with HFRS include Puumala virus (PUUV), Dobrava virus (DOBV), Seoul virus (SEOV), and Hantaan virus (HTNV).
A need for vaccines against HFRS has been recognized since HTNV was isolated in 1978 (16). Inactivated-virus vaccines based on HTNV, SEOV, and PUUV have been developed in Asia and are currently being evaluated for efficacy in regions of endemicity (12). As an alternative to traditional killed-virus vaccines that require the growth of virus in appropriate containment, chemical inactivation, and formulation with adjuvants, we developed candidate DNA vaccines comprised of a mammalian expression plasmid containing the M genome segment of SEOV or HTNV. These HFRS DNA vaccines express the G1 and G2 glycoproteins and elicit high-titer neutralizing antibodies (NAbs) in rodents and nonhuman primates (11, 13, 15). SEOV and HTNV M genome segment-based DNA vaccines protect against SEOV, HTNV, and DOBV, but not PUUV, in a hamster infection model (11, 13, 15).
Basic research leading to a gene-based vaccine that protects against HPS has been ongoing since the isolation of the first HPS-associated hantavirus in the mid-1990s. There are reports that candidate DNA vaccines comprised of ∼500-nucleotide stretches of the SNV M genome segment, or the full-length S gene, were immunogenic in mice (3) and conferred some protection against infection with SNV in a deer mouse infection model (4). The protection was surmised to be cell mediated because there was no convincing evidence that these constructs elicited a neutralizing, or otherwise protective, antibody response. Here, we describe the development and testing of an ANDV M genome segment-based DNA vaccine that elicited high-titer NAbs in nonhuman primates. In addition, we report that the humoral response elicited by this vaccine was sufficient to confer passive protection on hamsters against lethal HPS even when administered up to 5 days postexposure.
MATERIALS AND METHODS
Viruses, cells, medium, and MAbs.
HTNV strain 76-118 (16), ANDV strain Chile-9717869 (14), Black Creek Canal virus (BCCV) (23), and SNV strain CC107 (25) were propagated in Vero E6 cells (Vero C1008; ATCC CRL 1586). Transient-expression experiments were performed with COS cells (COS-7; ATTC CRL1651). Both cell types were maintained in Eagle's minimal essential medium with Earle's salts containing 10% fetal bovine serum, 10 mM HEPES (pH 7.4), and antibiotics (penicillin [100 U/ml], streptomycin [100 μg/ml], and gentamicin sulfate [50 μg/ml]) at 37°C in a 5% CO2 incubator.
HTNV G2-specific monoclonal antibodies (MAbs) (MAb-23G10, MAb-3D7, MAb-16E6, and MAb-HC02) and HTNV G1-specific MAbs (MAb-2D5, MAb-6D4, MAb-8B6, MAb-3D5, and MAb-10F11) were described previously (1, 24).
Construction of hantavirus M genome segment-based DNA vaccine plasmids.
The construction of the HTNV M DNA vaccine plasmid, pWRG/HTN-M(x), was described previously (11). To construct the ANDV M genome segment-based DNA vaccine plasmid, pWRG/AND-M, viral RNA was isolated from ANDV-infected Vero E6 cells using TRIzol (Invitrogen, Carlsbad, Calif.) by standard methods. The RNA was reverse transcribed using Superscript II reverse transcriptase (Invitrogen) at 50°C for 50 min and then inactivated by incubation at 70°C for 15 min. RNA was removed by digestion with RNase H at 37°C for 20 min. Forward and reverse primers based on the published SNV and PUUV sequences, respectively, were included in the reverse transcription reaction: forward primer, SN-Fj (5′-GGCCGCGGCCGCGGATCTGCAGGAATTCGGCACGAGAGTAGTAGACTCCGCACGAAGAAGC), and reverse primer, PUUM-R (5′-GCGCGGATCCTAGTAGTATGCTCCGCAGGAAC). The forward primer included a NotI restriction site (underlined) and 24 nucleotides upstream of the M genome segment noncoding region that were previously found to be important for expressing G1 in pWRG/HTN-M(x) (reference 11 and unpublished data). The reverse primer included a BamHI restriction site (underlined). cDNA was purified with a PCR purification kit (Qiagen) and used as a template in a PCR. Primers SN-Fj and PUUM-R were included in the PCR, which used Platinum Taq High Fidelity DNA polymerase (Invitrogen): one 3-min cycle at 94°C followed by 30 cycles of 94°C for 30 s and 68°C for 8 min. The PCR product was cut with NotI and BamHI and then ligated into NotI-BglII-cut pWRG7077 vector to produce pWRG/AND-M(1.1), hereafter referred to as pWRG/AND-M. Plasmid DNA was purified using Qiagen Maxiprep DNA purification kits according to the manufacturer's directions. At the time this plasmid was constructed, the ANDV M gene sequence was unknown, so we sequenced the M gene and vector-insert junctions, using a primer-walking technique and an ABI 3100 genetic analyzer.
Immunoprecipitation.
Radioimmunoprecipitation assays (RIPA) using COS cell lysate labeled with Promix ([35S]methionine and [35S]cysteine; Amersham) were performed exactly as described previously (11). ANDV-infected cell lysates were made by infecting Vero E6 monolayers with ANDV at a multiplicity of infection of 0.1. After 72 h, the cells were starved for 30 min in methionine- and cysteine-free medium and then radiolabeled for 17 h in medium containing 600 μCi of Promix per T-75 flask. Lysates were made using 4% Zwittergent 3-14 (Calbiochem-Bering) RIPA lysis buffer as described previously (26). Reduced samples were run on 4 to 12% Bis-Tris sodium dodecyl sulfate-polyacrylamide gel electrophoresis gradient gels with MOPS (morpholinepropanesulfonic acid) running buffer (NuPage) at 200 V of constant voltage.
N-specific ELISA.
The enzyme-linked immunosorbent assay (ELISA) used to detect N-specific antibodies was previously described (11, 10, 13). The antigen consisted of either a truncated SEOV N (amino acids 1 to 117) or a truncated PUUV N (amino acids 1 to 117) expressed as a histidine-tagged fusion protein using the pRSET plasmid (Invitrogen) in Escherichia coli BL21(DE3) (Novagen, Inc.) and purified by affinity chromatography on Ni-nitrilotriacetic acid columns (Qiagen). Endpoint titers were determined as the highest dilution that had an optical density greater than the mean optical density of serum samples from negative control wells plus 3 standard deviations. The SEOV N antigen was used to detect HTNV N-specific antibodies, and the PUUV N was used to detect ANDV N-specific antibodies.
PRNT.
Neutralization assays were performed as previously described (11). HTNV, ANDV, and BCCV plaque reduction neutralization tests (PRNT) were stained with neutral red after 1 week, and SNV PRNT were stained after 9 days. Plaques were counted (at 37°C) 2 to 3 days after staining.
IFAT.
Indirect fluorescent antibody tests (IFAT) were a modification of a previously described procedure (12). COS cells grown on 15-mm-diameter glass coverslips in 12-well cell culture plates were transfected with 1 μg of pWRG/AND-M DNA using Fugene6 (Boehringer Mannheim) as described by the manufacturer. Two days after transfection, the coverslips were rinsed once with phosphate-buffered saline (PBS; pH 7.4) and fixed with acetone for 10 min at room temperature. The slides were rinsed three times in PBS and blocked for 10 min in PBS containing 5% fetal bovine serum and 3% goat serum. Hamster sera were diluted 1:100 in blocking buffer and then incubated on the transfected cells for 1 h at 37°C. The coverslips were rinsed three times with PBS and incubated for 1 h at 37°C with biotin-labeled goat anti-hamster immunoglobulin G and immunoglobulin M antibodies (Pharmingen). The coverslips were rinsed as before and incubated for 30 min at 37°C with fluorescein-labeled streptavidin (Kirkegaard & Perry Laboratories). Hoechst stain (1 μg per ml) was included in the streptavidin solution as a counterstain. The coverslips were rinsed three times with PBS and once with deionized water and then placed on a drop of fluorescent mounting medium (DAKO) on glass slides. The cells were observed with a Nikon E600 fluorescence microscope.
Gene gun vaccinations.
Cartridges for the gene gun were prepared as described previously (11, 13). Plasmid DNA was precipitated onto gold beads (3 μg of DNA per mg of gold), and then tubing was coated with the DNA-coated gold beads. Gene gun cartridges consisting of 0.5 mg of gold coated with ∼0.75 μg of plasmid DNA were prepared and stored desiccated at 4°C until they were used. Syrian hamsters were vaccinated with the XR1 particle-mediated epidermal delivery device (gene gun) (Powderject Vaccines, Inc., Madison, Wis.), four administrations per vaccination, at nonoverlapping sites on the shaved abdominal epidermis using 400 lb of helium pressure/in2. Female rhesus macaques (Macaca mulatta) were vaccinated with similar cartridges under the same gene gun conditions used to vaccinate the hamsters; however, the monkeys received eight administrations (four on the abdomen and four over the inguinal lymph nodes) per vaccination. The hamsters and monkeys were anesthetized during the painless gene gun procedure. The only visible effect was mild erythema at the sites of vaccination.
Antibody injections.
Lyophilized human convalescent-phase plasma from a human HPS patient was reconstituted in water and recalcified before use by adding CaCl2 to 0.1 M and incubation at 37°C for 4 h, at 4°C overnight, and at −20°C for 1 h. The treated plasma was thawed and centrifuged at 10,000 × g for 20 min, and the supernatant was collected. Monkey serum from DNA-vaccinated monkeys and human serum (PEL-FREEZ Biologics, Rogers, Ariz.) were heat inactivated (56°C; 30 min). One milliliter of serum or plasma was injected intraperitoneally into hamsters using a 1-ml syringe with a 25-gauge 5/8-in. needle.
Challenge with hantaviruses.
Adult female Syrian hamsters (Mesocricetus auratus) (Charles River) were injected intramuscularly (i.m.) (caudal thigh; 25-gauge 5/8-in. needle) with the appropriate hantavirus diluted in 0.2 ml of sterile PBS (pH 7.4). The challenge dose for ANDV was 2,000 PFU, which is 250 50% lethal doses (LD50) (14). The challenge dose for HTNV was 2,000 PFU, which is ∼1,000 50% infective doses (unpublished data). Work involving ANDV-infected hamsters was performed in a biosafety level 4 laboratory. Work involving HTNV-infected hamsters was performed while wearing a powered air-purifying respirator system and Tyvek coverall in a biosafety level 3 laboratory. The effect of vaccine on the survival outcome was assessed using a logistic regression model. Analysis was conducted using SAS version 8.2 (SAS Institute Inc., Cary, N.C.).
All animal research was conducted in accordance with procedures described in the Guide for the Care and Use of Laboratory Animals (18a). The facilities are fully accredited by the American Association for Accreditation of Laboratory Animal Care.
RESULTS
pWRG/HTN-M(x) partially protects against a lethal ANDV challenge.
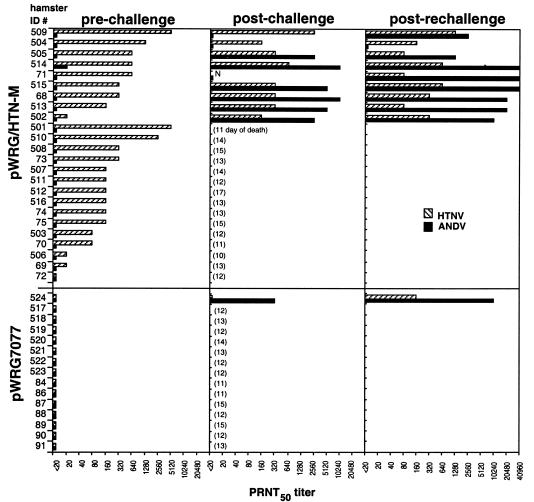
It was previously demonstrated that our HTNV M genome segment-based DNA vaccine, pWRG/HTN-M(x), could cross-protect against three of the four hantaviruses that cause HFRS (14). To determine if this vaccine could protect against the hantavirus that causes HPS, we vaccinated hamsters three times at 3-week intervals with pWRG/HTN-M(x) or a negative control plasmid and then challenged them with ANDV (250 LD50; i.m.) 3 weeks after the last vaccination. Two independent experiments were performed, and the combined results are shown in Fig. 1. The vaccine elicited HTNV NAb (50% neutralization geometric mean titer, 226; range, <20 to 5,120) in all but one hamster. ANDV cross-NAb was not detected, with one exception (no. 514; titer, 20). After challenge, 15 of 24 hamsters vaccinated with pWRG/HTN-M(x) died and 14 of 15 negative controls died. The mean day of death was 13 for both groups. Thus, the protection against a lethal ANDV challenge afforded by vaccination with pWRG/HTN-M(x) was not statistically significant but was suggestive (P = 0.0569). Hamsters that survived challenge were rechallenged with ANDV to ensure that they were exposed to virus. At least one animal (no. 504) had no antibody response after two successive challenges but was clearly protected from lethal disease.
FIG. 1.
Evaluation of HFRS DNA vaccine in ANDV-hamster lethal-disease model. Hamsters were vaccinated with pWRG/HTN-M(x) or the negative control plasmid pWRG7077 and then challenged with ANDV. For animals that succumbed, the day of death is shown in parentheses. Animals that survived the first challenge were rechallenged with ANDV. Sera drawn on the day of challenge (pre-challenge), 4 to 6 weeks after challenge (post-challenge), and 28 to 48 days after a second challenge (post-rechallenge) were tested for HTNV- and ANDV-specific NAbs by PRNT. The bars represent PRNT titers. Hamster identification numbers (ID#) 68 to 91 and 501 to 523 represent two independent experiments. N, not done.
ANDV M genome segment-based DNA vaccine expresses G1 and G2.
Because the level of protection against ANDV afforded by pWRG/HTN-M(x) in our experiments was only 38%, we endeavored to construct an ANDV M genome segment-based DNA vaccine. The full-length M genome segment of ANDV strain Chile-9717869 was cloned by reverse transcription-PCR into pWRG7077 to yield pWRG/AND-M. We sequenced the entire M genome segment open reading frame. The sequence of our cloned M genome segment was almost identical to the published M genome segment sequence of ANDV (GenBank accession number AF291703), which is not surprising because the viral isolates were from the same rodent specimen (18). There were two adenine-to-guanine nucleotide changes. The change at position 1504 was silent, and the change at position 1840 resulted in a threonine-to-alanine substitution at amino acid 597.
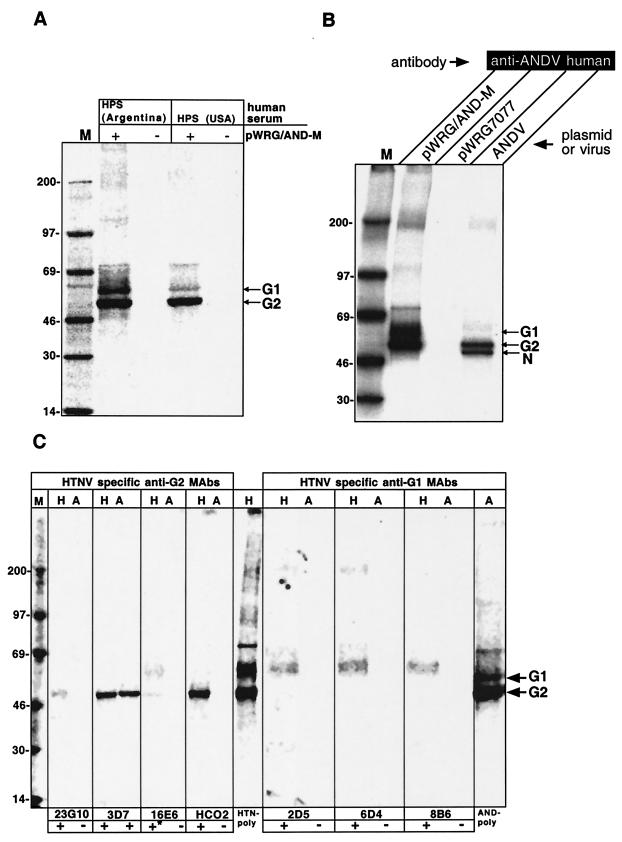
The expression of G1 and G2 in transfected COS cells was evaluated by RIPA. Serum pools from convalescent HPS patients immunoprecipitated polypeptides with the predicted sizes of G1 and G2 from pWRG/AND-M-transfected cells or ANDV-infected cells (Fig. 2A and B). The masses of the expression products were similar to the masses of G1 and G2 of other hantaviruses, which range from 68 to 76 kDa for G1 and 52 to 58 kDa for G2 (27). We presume that the ∼46-kDa protein in the ANDV-infected cells, but not the pWRG/AND-M transfected cells, was the ANDV nucleocapsid protein. To confirm that the polypeptides were G1 and G2, we screened a battery of HTNV G1- and G2-specific MAbs for the capacity to immunoprecipitate the ANDV glycoproteins from cells transfected with pWRG/AND-M or pWRG/HTN-M(x). We were unable to identify HTNV G1-specific MAbs that cross-reacted with the ANDV G1 protein: MAb-2D5, MAb-6D4, MAb-8B6 (Fig. 2C), MAb-10F11, or MAb-3D5 (data not shown). The HTNV G2-specific MAb-23G10, MAb-16E6, and MAb-HCO2 did not immunoprecipitate ANDV G2; however, the HTNV G2-specific MAb-3D7 did immunoprecipitate ANDV G2 from the pWRG/AND-M-transfected cells (Fig. 2C). By deduction, we concluded that the protein with mobility just under the 69-kDa marker that is precipitated by HPS patient sera but not by the G2-specific MAb-3D7 is ANDV G1. The identity of the ∼70-kDa protein remains unknown.
FIG. 2.
Expression from pWRG/AND-M. (A) HPS convalescent-phase sera from Argentina or the United States were used to immunoprecipitate radiolabeled proteins from COS cells transfected with pWRG/AND-M (+) or the empty vector plasmid pWRG7077 (−). (B) HPS convalescent-phase serum from Argentina (anti-ANDV human) was used to immunoprecipitate proteins from COS cells transfected with pWRG/AND-M, pWRG7077, or Vero E6 cells infected with ANDV. (C) The indicated HTNV-specific MAbs, HTNV-specific mouse hyperimmune ascitic fluid (HTN-poly), or HPS convalescent-phase serum from Argentina (AND-poly) was used to immunoprecipitate proteins from COS cells transfected with pWRG/HTN-M(x) (H) or pWRG/AND-M (A). +, G1 or G2 was immunoprecipitated; −, no protein was immunoprecipitated; *, both G1 and G2 were immunoprecipitated. Molecular mass marker (M) sizes in kilodaltons are shown on the left, and the positions of G1, G2, and N are shown on the right.
pWRG/AND-M DNA vaccine is neither immunogenic nor protective in hamsters.
To test the immunogenicity of pWRG/AND-M, we vaccinated 24 hamsters three times at 3-week intervals using a gene gun, collected serum samples, and tested them for NAb by PRNT. ANDV-specific NAbs were not detected (data not shown). Hamsters vaccinated with pWRG/HTN-M(x) on the same days did develop HTNV-specific NAbs with titers as high as 10,240 (data not shown). To determine if vaccination with pWRG/AND-M elicited ANDV G1- or G2-specific nonneutralizing antibodies, we performed IFAT with cells transfected with pWRG/AND-M. No antibody against G1 or G2 was detected in representative sera from hamsters vaccinated with pWRG/AND-M, but antibody was detected in positive control samples, which were sera from hamsters previously infected with ANDV (data not shown). We repeated the entire vaccination experiment on a second group of seven hamsters, and again, no NAb response was detected (data not shown). Because there was a possibility that the vaccinations with pWRG/AND-M elicited nonhumoral, but nevertheless protective, immune responses, we challenged eight hamsters from the first experiment and seven hamsters from the second experiment with 250 LD50 of ANDV. Twelve of the 14 hamsters vaccinated with pWRG/AND-M developed HPS and died. Six of eight unvaccinated hamsters developed HPS and died. The mean days of death were between 12 and 13 for both vaccinated and unvaccinated groups. From these negative data, we concluded that pWRG/AND-M was not immunogenic in Syrian hamsters.
pWRG/AND-M elicits a high-titer NAb response in rhesus macaques.
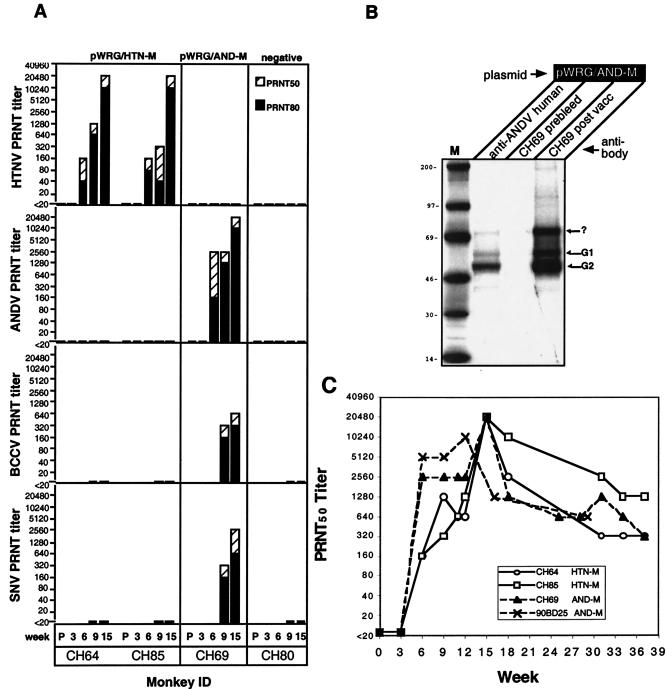
To determine if the lack of immunogenicity of pWRG/AND-M in hamsters was a species-specific phenomenon, we tested the plasmid in a rhesus macaque. The monkey, no. CH69, was vaccinated by gene gun with pWRG/AND-M four times (weeks 0, 3, 6, and 12). As positive controls, two rhesus macaques were vaccinated with pWRG/HTN-M(x), which was previously shown to be immunogenic in nonhuman primates (11). Sera collected before each vaccination and then 3 weeks after the fourth vaccination were tested for the presence of HTNV and ANDV NAbs (Fig. 3A and C). Monkey CH69, vaccinated with pWRG/AND-M, and the positive control monkeys, vaccinated with pWRG/HTN-M(x), developed NAb responses after the second vaccination, and the NAb titers were extraordinarily high after the fourth vaccination (Fig. 3A and C).
FIG. 3.
Immunogenicities of hantavirus DNA vaccines in nonhuman primates. (A) Rhesus macaques were vaccinated with pWRG/HTN-M(x), pWRG/AND-M, or a negative control plasmid. Sera were collected before the first vaccination (P) and 3 weeks after the first, second, third, and fourth vaccinations (weeks 3, 6, 9, and 15, respectively). HTNV-, ANDV-, BCCV-, and SNV-specific PRNT were performed, and the endpoint 50% (PRNT50) and 80% (PRNT80) titers were determined. (B) Sera from monkey CH69 collected before (prebleed) and after (post-vacc) four vaccinations with pWRG/AND-M were tested by RIPA for G1- and G2-specific antibodies using radiolabeled lysates from cells transfected with pWRG/AND-M. Human HPS patient convalescent-phase serum (anti-ANDV human) was used as a positive control for anti-ANDV antibodies. Molecular mass marker (M) sizes in kilodaltons are shown on the left, and the positions of G1, G2, and a ∼70-kDa protein (identity unknown) (?) are shown on the right. (C) NAb responses in monkeys vaccinated with either pWRG/HTN-M(x) or pWRG/AND-M were determined after each vaccination and then in the indicated weeks after the first vaccination (week 0). Monkeys CH64, CH85, and CH69 were vaccinated in weeks 0, 3, 6, and 12, and monkey 90BD25 was vaccinated in weeks 0, 3, 6, and 9. NAb titers to HTNV (solid lines) or ANDV (dashed line) were determined by PRNT.
We tested sera from the vaccinated monkeys for the capacity to cross-neutralize other HPS-associated hantaviruses. Serum from the monkey vaccinated with pWRG/AND-M, but not pWRG/HTN-M(x), neutralized SNV and BCCV (Fig. 3A). Sera from monkeys vaccinated with pWRG/AND-M or pWRG/HTN-M(x) did not cross-neutralize HTNV or ANDV, respectively.
Pre- and postvaccination (6 weeks after the last vaccination), serum was collected from monkey CH69 and tested by RIPA for the capacity to immunoprecipitate the ANDV glycoproteins. The postvaccination serum, but not the prevaccination serum, immunoprecipitated proteins similar to those immunoprecipitated by human convalescent-phase sera: a strong G2 band, a weak G1 band, and a ∼70-kDa band of unknown identity (Fig. 3B).
To confirm that vaccination with pWRG/AND-M was immunogenic in rhesus macaques, we vaccinated a second animal four times at 3-week intervals. This monkey (no. 90BD25) developed a PRNT50 titer (reciprocal of highest dilution neutralizing 50% of the plaques) of 5,120 after the second vaccination and a titer of 10,240 3 weeks after the fourth vaccination (Fig. 3C). Thus, the capacity of pWRG/AND-M to elicit high-titer NAb in nonhuman primates was reproducible.
To look at the duration of the NAb response in the monkeys vaccinated with the HPS or HFRS DNA vaccine, serum samples were periodically collected for ∼6 months. The monkeys vaccinated with pWRG/AND-M still had PRNT50 titers between 320 (monkey no. 90BD25) and 640 (monkey no. CH69) 20 and 25 weeks after the last vaccination, respectively (Fig. 3C). The two positive control monkeys vaccinated with pWRG/HTN-M(x) still had homologous PRNT50 titers of ≥320 25 weeks after the last vaccination.
Passive transfer of serum from a monkey vaccinated with pWRG/AND-M 1 day before challenge delays or prevents HPS in hamsters.
Having successfully vaccinated rhesus macaques with an HPS DNA vaccine, we were interested in determining if the NAb response elicited by this vaccine could protect hamsters from a lethal ANDV infection. To test this, serum from a monkey vaccinated with pWRG/AND-M, or a monkey vaccinated with a negative control plasmid, was injected into groups of four hamsters. The next day, the animals were challenged with ANDV (250 LD50; i.m.) and observed daily for 4 weeks. All hamsters that received serum containing ANDV NAb survived, and all hamsters that received negative control serum died between 10 and 13 days after challenge (Table 1). PRNT were performed on serum samples collected on the day of challenge (day 0) and collected from survivors on day 28. Hamsters that were injected with the protective monkey serum, which had an ANDV PRNT50 titer of 20,480, had PRNT50 titers between 320 and 1,280 at the time of challenge. Four weeks later, these hamsters had no detectable NAb and no nucleocapsid-specific antibody as measured by ELISA. Thus, these hamsters not only survived, but also, the data suggest that they had sterile immunity to infection from the challenge.
TABLE 1.
Pre- and postchallenge passive transfer of sera from rhesus macaques vaccinated with pWRG/AND-M to Syrian hamsters
| Hamster no. | Antibody
|
Day 0 PRNT titerc | Challenge virusd | Day of deathe | Terminal bleedf
|
% Protection
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Sourcea | Dayb injected | PRNT titerg | ELISA titerh | From lethality | From infectioni | ||||
| 905 | AND-M | −1 | 320 | ANDV | − | <20 | <100 | 50 | 50 |
| 906 | −1 | 640 | ANDV | − | <20 | <100 | |||
| 907 | −1 | 320 | ANDV | − | <20 | <100 | |||
| 908 | −1 | 1,280 | ANDV | − | <20 | <100 | |||
| 105 | −1 | 20 | ANDV | 23 | NA | NA | |||
| 106 | −1 | 40 | ANDV | 23 | NA | NA | |||
| 107 | −1 | 20 | ANDV | 40 | NA | NA | |||
| 108 | −1 | 20 | ANDV | 40 | NA | NA | |||
| 901 | Negative control | −1 | <20 | ANDV | 12 | NA | NA | 0 | 0 |
| 902 | −1 | <20 | ANDV | 13 | NA | NA | |||
| 903 | −1 | <20 | ANDV | 10 | NA | NA | |||
| 904 | −1 | <20 | ANDV | 13 | NA | NA | |||
| 101 | −1 | <20 | ANDV | 10 | NA | NA | |||
| 102 | −1 | <20 | ANDV | 14 | NA | NA | |||
| 103 | −1 | <20 | ANDV | 10 | NA | NA | |||
| 104 | −1 | <20 | ANDV | 11 | NA | NA | |||
| 909 | AND-M | 3 | <20 | ANDV | − | <20 | <100 | 88 | 14 |
| 910 | 3 | <20 | ANDV | − | <20 | 400 | |||
| 911 | 3 | <20 | ANDV | − | 2,560 | 12,800 | |||
| 912 | 3 | <20 | ANDV | − | 160 | 800 | |||
| 109 | 3 | <20 | ANDV | − | >640 | 1,600 | |||
| 110 | 3 | <20 | ANDV | − | 640 | 6,400 | |||
| 111 | 3 | <20 | ANDV | 12 | NA | NA | |||
| 112 | 3 | <20 | ANDV | − | >640 | 3,200 | |||
| 113 | AND-M | 4 | <20 | ANDV | − | 160 | 400 | 100 | 0 |
| 114 | 4 | <20 | ANDV | − | 640 | 400 | |||
| 115 | 4 | <20 | ANDV | − | >640 | 12,800 | |||
| 116 | 4 | <20 | ANDV | − | 320 | 1,600 | |||
| 117 | AND-M | 5 | <20 | ANDV | − | 320 | 1,600 | 100 | 0 |
| 118 | 5 | <20 | ANDV | − | >640 | 1,600 | |||
| 119 | 5 | <20 | ANDV | − | 640 | 800 | |||
| 120 | 5 | <20 | ANDV | − | 160 | 400 | |||
| 121 | AND-M | 6 | <20 | ANDV | 11 | NA | NA | 38 | 0 |
| 122 | 6 | <20 | ANDV | − | 40 | 800 | |||
| 123 | 6 | <20 | ANDV | 13 | NA | NA | |||
| 124 | 6 | <20 | ANDV | 12 | NA | NA | |||
| 913 | 6 | <20 | ANDV | 11 | NA | NA | |||
| 914 | 6 | <20 | ANDV | − | 1,280 | 12,800 | |||
| 915 | 6 | <20 | ANDV | 10 | NA | NA | |||
| 916 | 6 | <20 | ANDV | − | 1,280 | 6,400 | |||
| 917 | AND-M | 9 | <20 | ANDV | 11 | NA | NA | 25 | 0 |
| 918 | 9 | <20 | ANDV | 13 | NA | NA | |||
| 919 | 9 | <20 | ANDV | − | 10,240 | 12,800 | |||
| 920 | 9 | <20 | ANDV | 11 | NA | NA | |||
| 921 | AND-M | −1 | 160 | PBS | − | <20 | <100 | 100 | 100 |
| 922 | −1 | 640 | PBS | − | <20 | <100 | |||
| 923 | −1 | <20 | PBS | − | <20 | <100 | |||
| 924 | −1 | 160 | PBS | − | <20 | <100 | |||
Serum from monkey vaccinated with pWRG/AND-M (AND-M) or negative control sera. The monkey serum used in experiment 1 (no. 909 to 924) had a PRNT50 titer of 20,480, and the serum used in experiment 2 (no. 109 to 124) had a PRNT50 titer of 1,280.
Day antibody injected relative to challenge (day 0).
NAb titer in hamster serum at time of challenge (PRNT50).
2,000 PFU of ANDV (250 LD50) or PBS was injected i.m. on day 0.
−, animal survived.
In experiments 1 and 2, the terminal bleed was obtained on days 28 and 98, respectively.
Reciprocal of highest dilution neutralizing 50% of the plaques; NA, not applicable.
Endpoint ELISA titer. NA, not applicable.
Protection from infection (sterile immunity) indicates no detectable antibody response to nucleocapsid in terminal bleed.
In a second experiment, a different serum pool from a monkey vaccinated with pWRG/AND-M (ANDV PRNT50 titer, 640) was injected into four hamsters. As negative controls, four hamsters were injected with serum from a monkey vaccinated with a negative control plasmid. The hamsters were challenged with ANDV (250 LD50; i.m.) and observed daily for 14 weeks. As expected, all of the hamsters injected with the negative control monkey serum developed HPS and died between days 10 and 14 (Table 1). Whereas in the first experiment all of the hamsters injected with the serum from the monkey vaccinated with pWRG/AND-M were sterilely protected, in the second experiment, two of the hamsters died on day 23 and the other two hamsters died on day 40. Together, the aforementioned experiments indicate that passive transfer of serum from a monkey vaccinated with pWRG/AND-M on the day before challenge can sterilely protect hamsters from a lethal ANDV challenge or significantly delay disease onset and death.
Passive transfer of serum from a monkey vaccinated with pWRG/AND-M to hamsters 4 or 5 days after ANDV challenge completely protects against lethal HPS.
We tested serum from a monkey vaccinated with pWRG/AND-M for protective efficacy when administered to hamsters 3, 4, 5, 6, or 9 days after ANDV challenge (Table 1). Fifteen of the 16 hamsters that received antibody on day 3, 4, or 5 after challenge survived. However, when antibody was administered 6 days after challenge, only three of eight hamsters survived, and when antibody was administered 9 days after challenge, only one of four hamsters survived. All but one of the survivors from the postexposure experiments (no. 909; day 3) were infected with ANDV, as measured by PRNT and nucleocapsid-specific ELISA. Unlike the prechallenge passive-transfer experiments described above, in the postchallenge passive-transfer experiments, we did not observe any late deaths. Thus, immunoprophylaxis with sera from monkeys vaccinated with pWRG/AND-M, up to 5 days after a lethal challenge with ANDV, protected from 88 to 100% of the ANDV-challenged hamsters.
Passive transfer of sera from HTN-M DNA-vaccinated monkeys protects hamsters against HTNV infection.
In earlier studies, it was demonstrated that vaccinating hamsters with pWRG/HTN-M(x) elicited NAbs and protected against infection (11); however, whether the antibodies elicited were, by themselves, sufficient to protect was not tested. To address this question, groups of hamsters either were not injected or were injected with a pool of sera from monkeys vaccinated four times with pWRG/HTN-M(x) (PRNT50 titer, 20,480) or with serum from a monkey vaccinated with a negative control plasmid. One day after passive transfer, the hamsters were bled and challenged with HTNV. Five weeks after challenge, the hamsters were terminally bled, and sera from day 0 and day 35 were tested for HTNV NAbs by PRNT and nucleocapsid-specific antibodies were tested by ELISA (Table 2). All of the hamsters that were injected with the negative control serum or no serum were clearly infected, as indicated by high PRNT and nucleocapsid-specific ELISA titers. In contrast, six of the eight hamsters injected with the sera from the monkeys vaccinated with pWRG/HTN-M(x) failed to develop anti-nucleocapsid antibodies detectable by ELISA. Hamster 495 had a low ELISA titer, indicating a low level of infection. Although hamster 498 was in the group injected with immune serum, no NAb response was detected at the time of challenge, indicating that antibody was not successfully transferred, which explains why this animal was not protected against HTNV infection. Thus, sera from nonhuman primates vaccinated with pWRG/HTN-M(x), administered 1 day before challenge, were sufficient to protect hamsters against infection with HTNV.
TABLE 2.
Passive transfer of sera from rhesus macaques vaccinated with pWRG/HTN-M (x) in a nonlethal Syrian hamster infection model
| Hamster no. | Antibody sourcea | Day 0 PRNT titerb | Challenge virusc | Terminal bleedf
|
Sterile immunityg | |
|---|---|---|---|---|---|---|
| PRNT titerd | ELISA titere | |||||
| 492 | HTN-M | 640 | HTNV | 20 | <100 | Y |
| 493 | 1,280 | HTNV | 80 | <100 | Y | |
| 494 | 640 | HTNV | 20 | <100 | Y | |
| 495 | 1,280 | HTNV | 20 | 200 | N | |
| 496 | 640 | HTNV | <20 | <100 | Y | |
| 497 | 1,280 | HTNV | 1,280 | <100 | Y | |
| 498 | <20 | HTNV | 5,120 | 12,800 | N | |
| 499 | 640 | HTNV | ND | <100 | Y | |
| 484 | Negative control | <20 | HTNV | >640 | >12,800 | N |
| 485 | 20 | HTNV | >640 | >12,800 | N | |
| 486 | <20 | HTNV | >640 | >12,800 | N | |
| 488 | <20 | HTNV | >640 | >12,800 | N | |
| 489 | <20 | HTNV | >640 | >12,800 | N | |
| 490 | <20 | HTNV | >640 | 3,200 | N | |
| 491 | <20 | HTNV | >640 | >12,800 | N | |
| 476 | None | <20 | HTNV | >640 | >12,800 | N |
| 477 | <20 | HTNV | >640 | >12,800 | N | |
| 478 | <20 | HTNV | >640 | >12,800 | N | |
| 479 | <20 | HTNV | >640 | >12,800 | N | |
| 480 | <20 | HTNV | >640 | >12,800 | N | |
| 481 | <20 | HTNV | >640 | >12,800 | N | |
| 482 | <20 | HTNV | >640 | >12,800 | N | |
| 483 | <20 | HTNV | >640 | >12,800 | N | |
HTN-M indicates sera (PRNT50 titer, 20,480) from monkeys vaccinated with pWRG/HTN-M(x); Negative control indicates serum from a negative control monkey vaccinated with irrelevant plasmid; none indicates no passive transfer.
NAb titer (50%) in hamster serum at time of challenge.
2,000 PFU of HTNV (1,000 LD50) was injected i.m. on day 0.
Reciprocal of highest dilution neutralizing 50% of the plaques; ND, not done.
Endpoint ELISA titer.
Terminal bleed was on day 35 after challenge.
Sterile immunity indicates no detectable antibody response to nucleocapsid. Y and N, yes and no, respectively.
Passive transfer of plasma from a human HPS patient.
Having demonstrated that sera from monkeys vaccinated with ANDV M genome segment-based DNA vaccines could protect against a lethal ANDV challenge when administered pre- or postexposure, we investigated the capacity of human convalescent-phase plasma from a Chilean HPS patient (human HPS plasma) to protect in the ANDV-hamster lethal-disease model. Human HPS plasma, with an initial ANDV NAb PRNT50 titer of 10,240, was injected into different groups of hamsters on day −1, 3, 4, or 5. A control group was injected with normal human serum on day −1. On day 0, blood was collected from the hamsters, and then the hamsters were challenged with ANDV (250 LD50; i.m.). As a control for toxicity, three hamsters that were injected with the human HPS plasma on day −1 were not challenged. The hamsters were monitored for 98 days, survivors were terminally bled, and PRNT and ELISA were performed on the day 0 and day 98 serum samples (Table 3). All of the hamsters that received normal human sera died between 10 and 12 days after challenge. Two of the four hamsters that received human HPS plasma on day −1 survived. The other two hamsters in the day −1 group developed HPS and died on days 57 and 68 after challenge. Seven of the 12 hamsters that received antibody on day 3, 4, or 5 after challenge survived. The hamsters that died in those groups did so between 11 and 15 days after challenge. The three hamsters in the toxicity control groups all remained healthy.
TABLE 3.
Pre- and postchallenge passive transfer of plasma from a Chilean HPS patient to Syrian hamsters
| Hamster no. | Antibody
|
Day 0 PRNT titerc | Challenge virusd | Day of deathe | Terminal bleedf
|
% Protection
|
|||
|---|---|---|---|---|---|---|---|---|---|
| Sourcea | Dayb injected | PRNT titerg | ELISA titerh | From lethality | From infectioni | ||||
| 125 | Normal | −1 | <20 | ANDV | 12 | NA | NA | 0 | 0 |
| 126 | <20 | ANDV | 10 | NA | NA | ||||
| 127 | <20 | ANDV | 11 | NA | NA | ||||
| 128 | <20 | ANDV | 12 | NA | NA | ||||
| 129 | HPS | −1 | 640 | ANDV | − | <20 | <100 | 50 | 50 |
| 130 | 1,280 | ANDV | 57 | NA | NA | ||||
| 131 | 640 | ANDV | 68 | NA | NA | ||||
| 132 | 1,280 | ANDV | − | <20 | <100 | ||||
| 133 | HPS | 3 | <20 | ANDV | − | >640 | 3,200 | 75 | 0 |
| 134 | <20 | ANDV | − | 160 | 800 | ||||
| 135 | <20 | ANDV | − | 80 | 800 | ||||
| 136 | <20 | ANDV | 12 | NA | NA | ||||
| 137 | HPS | 4 | <20 | ANDV | 12 | NA | NA | 50 | 0 |
| 138 | <20 | ANDV | 15 | NA | NA | ||||
| 139 | <20 | ANDV | − | 320 | 1,600 | ||||
| 140 | <20 | ANDV | − | 320 | 3,200 | ||||
| 141 | HPS | 5 | <20 | ANDV | − | >640 | 6,400 | 50 | 0 |
| 142 | <20 | ANDV | − | 40 | <100 | ||||
| 143 | <20 | ANDV | 11 | NA | NA | ||||
| 144 | <20 | ANDV | 11 | NA | NA | ||||
| 145 | HPS | −1 | 40 | None | − | <20 | <100 | 100 | 100 |
| 146 | 640 | None | − | <20 | <100 | ||||
| 147 | 320 | None | − | <20 | <100 | ||||
HPS indicates plasma (PRNT50, 10,240) from a human HPS patient; normal indicates normal human serum.
Day antibody injected (1 ml; intraperitoneal) relative to challenge (day 0).
NAb titer in hamster serum at time of challenge (PRNT50).
2,000 PFU of ANDV (250 LD50) was injected i.m. (ANDV) or no treatment (None).
−, animal lived.
Terminal bleed on day 98.
Reciprocal of highest dilution neutralizing 50% of the plaques; NA, not applicable.
Endpoint ELISA titer. NA, not applicable.
Protection from infection (sterile immunity) indicates no detectable antibody response to nucleocapsid in terminal bleed.
Serology results from the postchallenge sera indicate that the two hamsters that were injected with human HPS plasma on day −1 and survived were protected from infection (i.e., they did not produce anti-nucleocapsid antibodies) (Table 3). All but one of the hamsters that received the human HPS plasma after challenge and survived were nevertheless infected, because they all produced anti-nucleocapsid antibodies. Thus, human HPS plasma protected at least half the challenged hamsters when administered on day −1, 3, 4, or 5. Hamsters that received the plasma on day −1 were either protected from infection or survived more than four times longer than the controls.
DISCUSSION
Presently, there are no vaccines, effective antiviral drugs, or immunologics to protect against or treat HPS. This is disconcerting, because HPS afflicts previously healthy individuals in all age groups, disease progression is rapid, and the case fatality rate is one of the highest for any acute viral disease known. Reports of person-to-person transmission of ANDV-associated HPS in southern Argentina and Chile make development of countermeasures against this highly lethal disease more urgent (19, 29, 30). Here, we report the development of a candidate HPS DNA vaccine that elicits high-titer NAbs in nonhuman primates. Moreover, we report that the antibodies elicited by this vaccine can protect hamsters from lethal HPS, even when administered 5 days after challenge.
This is the first study in which a hantavirus disease model in an adult laboratory animal has been used to evaluate the protective efficacy of a candidate vaccine, drug, or immunoprophylactic. Previous studies used hantavirus infection models involving mice, hamsters, or bank voles to evaluate vaccines and immunoprophylactics or a suckling mouse neurologic-disease model to evaluate drugs (12, 27). Here, we used a recently described ANDV-hamster lethal-disease model (14). We confirmed that ANDV causes lethal HPS in adult Syrian hamsters and determined that the challenge had a relatively consistent outcome. Of the 35 hamsters that were negative controls in the active-vaccination or passive-transfer experiments, 100% of the ANDV-challenged hamsters were infected and 91% developed fatal HPS (mean day of death, 12; range; 10 to 15 days). The shortest time between challenge and the first symptoms of illness (e.g., dyspnea) was 9 days. The progression of clinical disease was rapid, and death usually occurred within 24 h after onset.
In an earlier study, we demonstrated that previous infection with HTNV, SEOV, DOBV, PUUV, or SNV could protect hamsters against a lethal ANDV challenge (14). From this, we reasoned that it might be possible to use our HTNV M genome segment-based DNA vaccine, pWRG/HTN-M(x), to protect hamsters against ANDV challenge. We tested this possibility and found that pWRG/HTN-M(x) protected 9 of 24 hamsters from a lethal ANDV challenge. This level of protection was not statistically significant (P = 0.0569) but did suggest that the vaccine was eliciting some immunity against ANDV. It is possible that the pWRG/HTN-M(x) vaccine would afford a higher level of protection against a challenge dose of <250 LD50 or against a different challenge route (e.g., an aerosol or oral route). There were essentially no ANDV cross-neutralizing antibodies either in the sera of pWRG/HTN-M(x)-vaccinated hamsters (Fig. 1) or in the HTNV-infected hamsters that were protected in an earlier work (14). This suggests that the cross-protection observed in previously infected hamsters was due to cell-mediated immunity targeting both nucleocapsid and glycoproteins whereas the partial cross-protection observed in the pWRG/HTN-M(x)-vaccinated hamsters was likely due to cell-mediated immunity targeting only the glycoproteins. It is theoretically possible that the product of the L genome segment could play a role in the protection observed in previously infected hamsters; however, there is presently no evidence that the viral polymerase elicits humoral or cell-mediated immunity. Cross-protection after infection with HTNV, but not after inoculation with the HTNV glycoproteins, suggests that vaccination with a plasmid(s) expressing both the HTNV nucleocapsid and glycoproteins might mimic HTNV infection and cross-protect against ANDV.
In an alternative approach to developing an HPS vaccine, we constructed a plasmid designed to specifically protect against viruses that cause HPS. The plasmid, pWRG/AND-M, contains the complete ANDV M gene open reading frame and expresses both the G1 and G2 glycoproteins in cell culture. To our knowledge, the BCCV M gene is the only other complete HPS hantavirus M gene that has been successfully cloned and expressed (22).
Vaccination with pWRG/AND-M elicited a potent NAb response in rhesus macaques. This is the first candidate HPS vaccine shown to unequivocally elicit a NAb response in any laboratory animal. Not only were NAbs produced in the monkeys, but also (i) NAbs were detected after only two vaccinations; (ii) NAb titers were very high (i.e., titers were as high as those found in HPS patient convalescent-phase serum); (iii) the NAbs cross-neutralized at least two other HPS-associated hantaviruses, SNV and BCCV; and (iv) NAbs were still detected 6 months after the last vaccination. The neutralization of SNV suggests that the pWRG/AND-M vaccine would protect against the major HPS hantaviruses in South America and North America, ANDV and SNV, respectively. The neutralization of BCCV suggests that vaccination with pWRG/AND-M might protect against a wide range of HPS-associated hantaviruses. These data, coupled with the HFRS DNA vaccine data (11), indicate that a vaccine comprised of both pWRG/HTN-M(x) and pWRG/AND-M could conceivably protect against several major hantaviruses known to be highly lethal to humans.
One of the more perplexing results we obtained during the course of this study was the failure of pWRG/AND-M to elicit a detectable immune response in hamsters. In two independent experiments, hamsters vaccinated three times with pWRG/AND-M failed to produce antibodies detectable by PRNT or IFAT and were not protected against a lethal ANDV challenge. In contrast, rhesus macaques vaccinated as few as two times with pWRG/AND-M developed a detectable NAb response. Although unlikely, it is possible that the DNA vaccine was nonimmunogenic in hamsters for technical reasons. Before exploring the mechanism by which pWRG/AND-M might fail to generate an immune response in hamsters, and whether this phenomenon is related to the highly lethal nature of ANDV in Syrian hamsters, it would be prudent to evaluate the pWRG/AND-M vaccine in hamsters and nonhuman primates in a side-by-side experiment using the same vaccine lot and vaccination schedule for both species. For the present study, the important point is that pWRG/AND-M is highly immunogenic in nonhuman primates.
In previous studies, it was demonstrated that DNA vaccines expressing the glycoproteins of SEOV or HTNV elicited NAbs in mice, hamsters, and nonhuman primates, and it was demonstrated that the presence of NAbs in vaccinated hamsters correlated with protection against infection (11, 13, 15). Here, we demonstrate for the first time that the humoral response elicited by DNA vaccination with pWRG/HTN-M(x) is sufficient to protect against infection with HTNV. Specifically, we demonstrated that passive transfer of serum from a monkey vaccinated with pWRG/HTN-M(x) 1 day before challenge provided sterilizing protection in six of eight hamsters challenged with HTNV. The two hamsters that were not protected either had a limited infection (hamster 495), as shown by a very low postchallenge anti-nucleocapsid titer, or did not receive a proper injection of serum (hamster 498), as shown by the absence of detectable NAb on the day of challenge. It is possible that a similar passive-transfer assay could be used as part of a clinical study to evaluate sera from humans vaccinated with pWRG/HTN-M(x) and to predict the efficacy of the vaccine.
Presently, there is no treatment for individuals exposed, or potentially exposed, to HPS hantaviruses. Reports that high NAb titers in patients admitted to hospitals correlated with a favorable clinical course suggested that NAbs might ameliorate disease, and therefore, that immunotherapy could be a viable treatment option for persons exposed to HPS viruses (5). For HFRS-associated hantaviruses, passive transfer of infected-rat immune serum or mouse MAbs conferred protection against infection in hamsters or neurologic disease in newborn rats or suckling mice (2, 17, 28, 31). For HPS hantaviruses, there have been no reports of the passive transfer of protective immunity. The discovery of the ANDV-hamster lethal-disease model has allowed us, for the first time, to evaluate the capacities of antibodies to protect against a hantavirus disease that resembles the disease in humans. Using this model, we demonstrated that passive transfer of serum from a monkey vaccinated with pWRG/AND-M protected 100% of challenged hamsters from a lethal ANDV infection when administered on day 4 or 5 after exposure. This finding indicates that it should be possible to develop a product [e.g., polyclonal immunoglobulin from primates, including humans, vaccinated with pWRG/AND-M and/or pWRG/HTN-M(x) or MAbs that neutralize ANDV and/or HTNV] that could be used to treat laboratory workers exposed to hantaviruses, family members or other close contacts of HFRS or HPS patients or medical personnel treating HPS patients, especially in South America, where there is evidence of person-to-person transmission of HPS (19, 29, 30).
HPS patient convalescent-phase plasma was essentially equivalent to the monkey serum when administered on day 3 postexposure (75 versus 88% protection) but protected only 50% of the hamsters when administered on day 4 or 5 postexposure. Due to low sample numbers, this difference could be an artifact. Alternatively, it is possible that the human NAbs were cleared more rapidly than the rhesus macaque NAbs, resulting in a lower effective NAb titer at the time of challenge. We have not evaluated the kinetics by which the monkey or human hantavirus-specific NAbs are cleared from hamsters.
Passive transfer of sera from monkeys vaccinated with pWRG/AND-M, or HPS patient plasma, administered 1 day before challenge either protected hamsters against a lethal ANDV challenge with sterile immunity or delayed disease onset and death by 1 to 8 weeks. In the experiments involving passive transfer of serum containing ANDV NAb (Tables 1 and 3), the only hamsters that died late were those that were injected with serum 1 day before challenge. The six hamsters died on days 23, 23, 40, 40, 57, and 68, for a mean day of death of 42. This was a significant delay in death, because the 12 hamsters that were injected with negative control serum (monkey or human) all died between days 10 and 14 (mean day of death, 12). Necropsies were performed on hamsters that died on day 40 or later. Three of the four hamsters died from HPS (no. 107 was the exception), as diagnosed from large volumes of fluid in the pleural cavity (data not shown). Infectious virus was isolated from the lungs and liver of hamster 130, which died from HPS 57 days after challenge (data not shown). It is possible that the late deaths of the hamsters injected with antibody on day −1 were the result of clearance of heterologous monkey or human ANDV-specific NAb and subsequent amplification of viruses that had escaped neutralization by the passively transferred primate antibody. We hypothesize that late deaths were not observed in hamsters that received serum postexposure because the challenged hamsters had mounted an active immune response to the challenge virus. This active immunity would normally be insufficient to protect the hamsters against lethal HPS; however, passively transferred immunity (e.g., NAbs in sera from monkeys vaccinated with pWRG/AND-M) administered on days 3 through 5 would suppress the infection and allow survival (22 of 28 survived [Tables 2 and 3]). The active immune response would persist and protect the hamster when, and if, the hamster was reexposed to ANDV after clearance of the heterologous antibody. In support of this, all but one (no. 902 [Table 1]) of the 26 survivors that received passively transferred antibody on day 3, 4, 5, 6, or 9 were nevertheless infected, as indicated by an anti-nucleocapsid and/or NAb response detectable several weeks after challenge. These data suggest that a post-hantavirus exposure prophylaxis treatment regimen might require repeated administrations of antibody or both passive transfer of antibodies and active vaccination. A passive-active vaccination approach for postexposure prophylaxis is routinely used to prevent other viral diseases, including hepatitis A, hepatitis B, and rabies (6, 7, 8).
We have not tested the capacities of passively transferred NAbs to reverse HPS in hamsters; however, the failure of NAbs to protect when administered on day 6 or 9 after challenge makes effectiveness after the onset of illness unlikely. In a previous study, NAbs were not detected in the sera of hamsters challenged with ANDV until after day 8 (14). Moreover, NAbs were detected in the sera and pleural fluids of hamsters that succumbed to HPS, indicating that the presence of actively produced NAbs was insufficient to protect against lethality (14). Others have reported that the small-molecule drug ribavirin might have been ineffective for treating HPS because, for most patients, drug treatment was initiated after the onset of clinical symptoms (9). The critical pathogenic juncture where damage caused by the infection is irreversible and prophylaxis is impossible has not been defined. Future studies characterizing the time course of HPS in the ANDV-hamster lethal-disease model will provide insights into the pathogenesis of HPS and should allow us to formulate strategies for pre- and postexposure prophylaxis and therapy.
Acknowledgments
The gene gun (Powderject XR1 particle-mediated epidermal delivery device) and pWRG7077 were kindly provided by Powderject Vaccine, Inc., Madison, Wis. Plasmids used to prepare N-specific ELISA antigen, pSEOSXdelta and pPUUSXdelta, were kindly provided by F. Elgh, Swedish Institute for Infectious Disease Control, Solona, Sweden. Sera from HPS patients in Argentina and the United States that were used in immunoprecipitations were provided by P. Padula, Instituto Nacional de Enfermedades Infecciosas, Bueno Aires, Argentina, and B. Hjelle, University of New Mexico School of Medicine, Albuquerque, N.Mex., respectively. Necropsies on late-onset cases were performed by Tom Larsen, USAMRIID.
Opinions, interpretations, conclusions, and recommendations are those of the author and are not necessarily endorsed by the U.S. Army or the Department of Defense.
The research described here was sponsored by the Military Infectious Disease Research Program, U.S. Army Medical Research and Material Command, Project no. ATOOO2_02_RD and TOOO2_01_RD.
REFERENCES
- 1.Arikawa, J., A. L. Schmaljohn, J. M. Dalrymple, and C. S. Schmaljohn. 1989. Characterization of Hantaan virus envelope glycoprotein antigenic determinants defined by monoclonal antibodies. J. Gen. Virol. 70:615-624. [DOI] [PubMed] [Google Scholar]
- 2.Arikawa, J., J. S. Yao, K. Yoshimatsu, I. Takashima, and N. Hashimoto. 1992. Protective role of antigenic sites on the envelope protein of Hantaan virus defined by monoclonal antibodies. Arch. Virol. 126:271-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bharadwaj, M., C. R. Lyons, I. A. Wortman, and B. Hjelle. 1999. Intramuscular inoculation of Sin Nombre hantavirus cDNAs induces cellular and humoral immune responses in BALB/c mice. Vaccine 17:2836-2843. [DOI] [PubMed] [Google Scholar]
- 4.Bharadwaj, M., K. Mirowsky, C. Ye, J. Botten, B. Masten, J. Yee, C. R. Lyons, and B. Hjelle. 2002. Genetic vaccines protect against Sin Nombre hantavirus challenge in the deer mouse (Peromyscus maniculatus). J. Gen. Virol. 83:1745-1751. [DOI] [PubMed] [Google Scholar]
- 5.Bharadwaj, M., R. Nofchissey, D. Goade, F. Koster, and B. Hjelle. 2000. Humoral immune responses in the hantavirus cardiopulmonary syndrome. J. Infect. Dis. 182:43-48. [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control. 1991. Hepatitis B virus: a comprehensive strategy for eliminating transmission in the United States through universal childhood vaccination. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb. Mortal. Wkly. Rep. 40(RR-13):1-19. [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. 1999. Human rabies prevention—United States, 1999. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb. Mortal. Wkly. Rep. 48(RR-1):1-21. [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 1999. Prevention of hepatitis A through active or passive immunization. Recommendations of the Advisory Committee on Immunization Practices (ACIP). Morb. Mortal. Wkly. Rep. 48(RR-12):1-37. [PubMed]
- 9.Chapman, L. E., G. J. Mertz, C. J. Peters, H. M. Jolson, A. S. Khan, T. G. Ksiazek, F. T Koster, K. F. Baum, P. E. Rollin, A. T. Pavia, R. C. Holman, J. C. Christenson, P. J. Rubin, R. E. Behrman, L. J. Bell, G. L. Simpson, and R. F. Sadek. 1999. Intravenous ribavirin for hantavirus pulmonary syndrome: safety and tolerance during 1 year of open-label experience. Antivir. Ther. 4:211-219. [DOI] [PubMed] [Google Scholar]
- 10.Elgh, F., A. Lundkvist, O. A. Alexeyev, H. Stenlund, T. Avsic-Zupanc, B. Hjelle, H. W. Lee, K. J. Smith, R. Vainionpaa, D. Wiger, G. Wadell, and P. Juto. 1997. Serological diagnosis of hantavirus infections by an enzyme-linked immunosorbent assay based on detection of immunoglobulin G and M responses to recombinant nucleocapsid proteins of five viral serotypes. J. Clin. Microbiol. 35:1122-1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hooper, J. W., D. Custer, E. Thompson, and C. S. Schmaljohn. 2001. DNA vaccination with the Hantaan virus M gene protects hamsters against three of four HFRS hantaviruses and elicits a high-titer neutralizing antibody response in rhesus monkeys. J. Virol. 75:8469-8477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hooper, J. W., and D. Li. 2001. Vaccines against hantaviruses, p. 171-191. In C. S. Schmaljohn and S. T. Nichol (ed.), Hantaviruses. Springer-Verlag, Berlin, Germany.
- 13.Hooper, J. W., K. I. Kamrud, F. Elgh, D. Custer, and C. S. Schmaljohn. 1999. DNA vaccination with hantavirus M segment elicits neutralizing antibodies and protects against Seoul virus infection. Virology 255:269-278. [DOI] [PubMed] [Google Scholar]
- 14.Hooper, J. W., T. Larsen, D. Custer, and C. S. Schmaljohn. 2001. A lethal disease model for hantavirus pulmonary syndrome. Virology 289:6-14. [DOI] [PubMed] [Google Scholar]
- 15.Kamrud, K. I., J. W. Hooper, F. Elgh, and C. S. Schmaljohn. 1999. Comparison of the protective efficacy of naked DNA, DNA-based Sindbis replicon, and packaged Sindbis replicon vectors expressing Hantavirus structural genes in hamsters. Virology 263:209-219. [DOI] [PubMed] [Google Scholar]
- 16.Lee, H. W., P. W. Lee, and K. M. Johnson. 1978. Isolation of the etiologic agent of Korean hemorrhagic fever. J. Infect. Dis. 137:298-308. [DOI] [PubMed] [Google Scholar]
- 17.Liang, M., Y. K. Chu, and C. Schmaljohn. 1996. Bacterial expression of neutralizing mouse monoclonal antibody Fab fragments to Hantaan virus. Virology 217:262-271. [DOI] [PubMed] [Google Scholar]
- 18.Meissner, J. D., J. E. Rowe, M. K. Borucki, and S. C. St. Jeor. 2002. Complete nucleotide sequence of a Chilean hantavirus. Virus Res. 89:131-143. [DOI] [PubMed] [Google Scholar]
- 18a.National Institutes of Health. 1996. Guide for the care and use of laboratory animals. National Institutes of Health, Bethesda, Md.
- 19.Padula, P. J., A. Edelstein, S. D. L. Miguel, N. M. Lopez, C. M. Rossi, and R. D. Rabinovich. 1998. Hantavirus pulmonary syndrome (HPS) outbreak in Argentina: molecular evidence for person-to-person transmission of Andes virus. Virology 241:323-330. [DOI] [PubMed] [Google Scholar]
- 20.Peters, C. J., and A. S. Khan. 2002. Hantavirus pulmonary syndrome: the new American hemorrhagic fever. Clin. Infect. Dis. 34:1224-1231. [DOI] [PubMed] [Google Scholar]
- 21.Peters, C. J., G. L. Simpson, and H. Levy. 1999. Spectrum of hantavirus infection: hemorrhagic fever with renal syndrome and hantavirus pulmonary syndrome. Annu. Rev. Med. 50:531-545. [DOI] [PubMed] [Google Scholar]
- 22.Ravkov, E. V., S. T. Nichol, C. J. Peters, and R. W. Compans. 1998. Role of actin microfilaments in Black Creek Canal virus morphogenesis. J. Virol. 72:2865-2870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rollin, P. E., T. G. Ksiazek, L. H. Elliott, E. V. Ravkov, M. L. Martin, S. Morzunov, W. Monroe, G. Glass, S. Ruo, et al. 1995. Isolation of Black Creek Canal virus, a new hantavirus from Sigmodon hispidus in Florida. J. Med. Virol. 46:35-39. [DOI] [PubMed] [Google Scholar]
- 24.Ruo, S. L., A. Sanchez, L. H. Elliott, L. S. Brammer, J. B. McCormick, and S. P. Fisher-Hoch. 1991. Monoclonal antibodies to three strains of hantaviruses: Hantaan, R22, and Puumala. Arch. Virol. 119:1-11. [DOI] [PubMed] [Google Scholar]
- 25.Schmaljohn, A. L., D. Li, D. L. Negley, D. S. Bressler, M. J. Turell, G. W. Korch, M. S. Ascher, and C. S. Schmaljohn. 1995. Isolation and initial characterization of a new found hantavirus from California. Virology 206:963-972. [DOI] [PubMed] [Google Scholar]
- 26.Schmaljohn, C., L. Vanderzanden, M. Bray, D. Custer, B. Meyer, D. Li, C. Rossi, D. Fuller, J. Fuller, J. Haynes, and J. Huggins. 1997. Naked DNA vaccines expressing the prM and E genes of Russian spring summer encephalitis virus and Central European encephalitis virus protect mice from homologous and heterologous challenge. J. Virol. 71:9563-9569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Schmaljohn, C. S., and J. W. Hooper. 2001. Bunyaviridae: the viruses and their replication, p. 1581-1602. In D. M. Knipe et al. (ed.), Fields virology, 4th ed. Lippincott Williams and Wilkins, Philadelphia, Pa.
- 28.Schmaljohn, C. S., Y. K. Chu, A. L. Schmaljohn, and J. M. Dalrymple. 1990. Antigenic subunits of Hantaan virus expressed by baculovirus and vaccinia virus recombinants. J. Virol. 64:3162-3170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Toro, J., J. D. Vega, A. S. Khan, J. N. Mills, P. Padula, W. Terry, Z. Yadon, R. Valderrama, B. A. Ellis, C. Pavletic, R. Cerda, S. Zaki, W. J. Shieh, R. Meyer, M. Tapia, C. Mansilla, M. Baro, J. A. Vergara, M. Concha, G. Calderon, D. Enria, C. J. Peters, and T. G. Ksiazek. 1998. An outbreak of hantavirus pulmonary syndrome, Chile, 1997. Emerg. Infect. Dis. 4:687-694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wells, R. M., E. S. Sosa, Z. E. Yadon, D. Enria, P. Padula, N. Pini, et al. 1997. An unusual hantavirus outbreak in southern Argentina: person-to-person transmission? Emerg. Infect. Dis. 3:171-174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zhang, X.-K., I. Takashima, and N. Hashimoto. 1989. Characteristics of passive immunity against hantavirus infection in rats. Arch. Virol. 105:235-246. [DOI] [PubMed] [Google Scholar]