Abstract
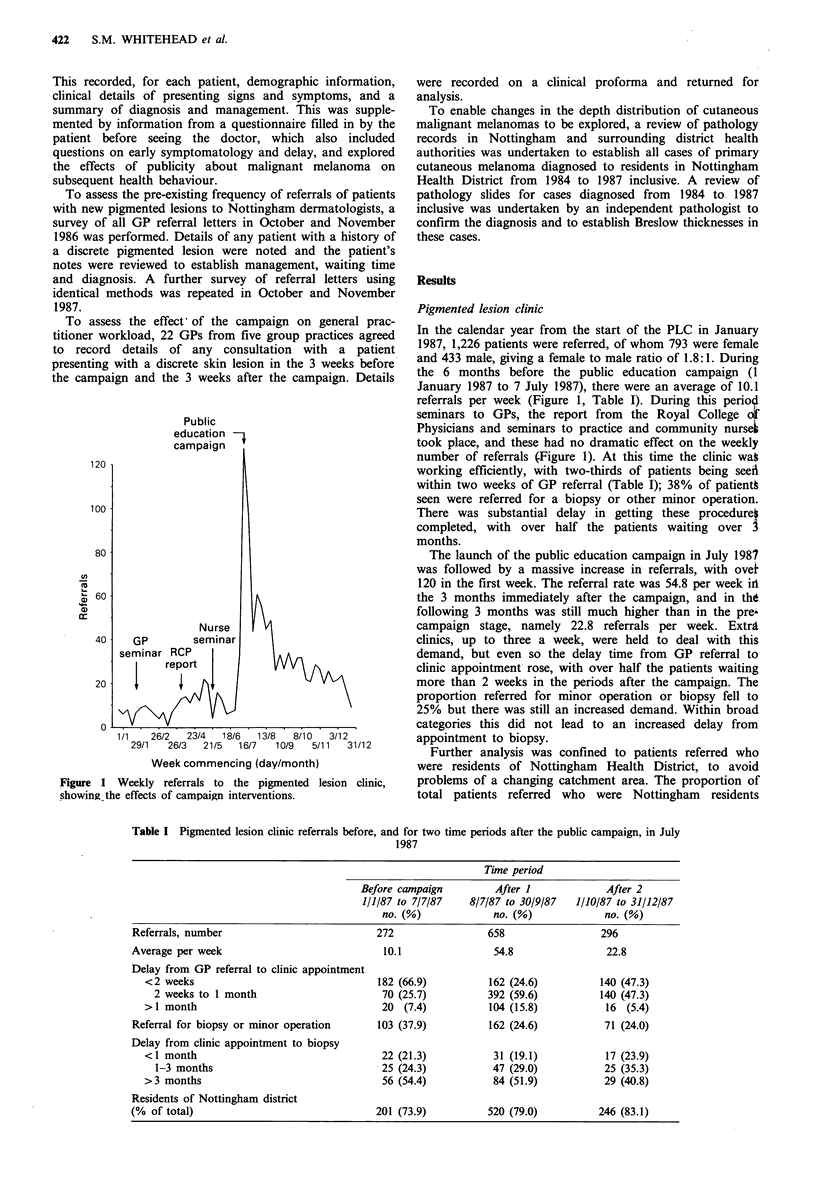
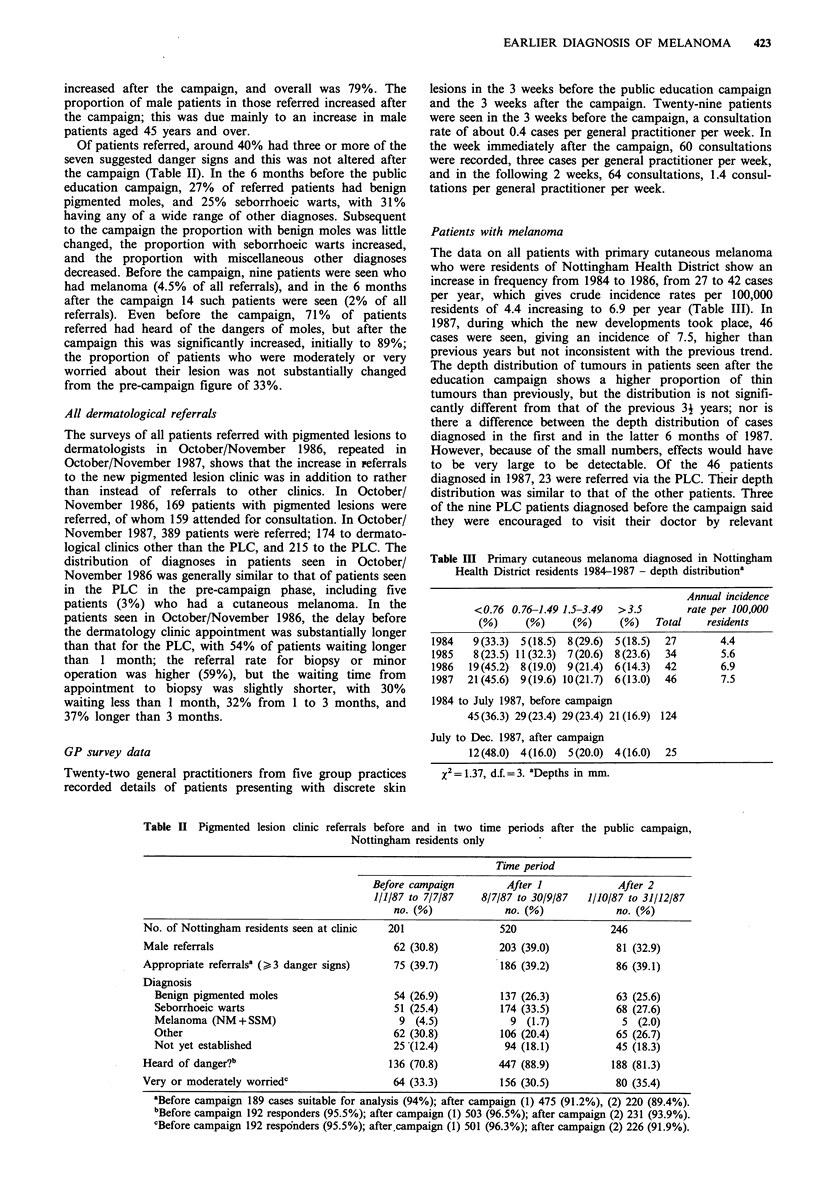
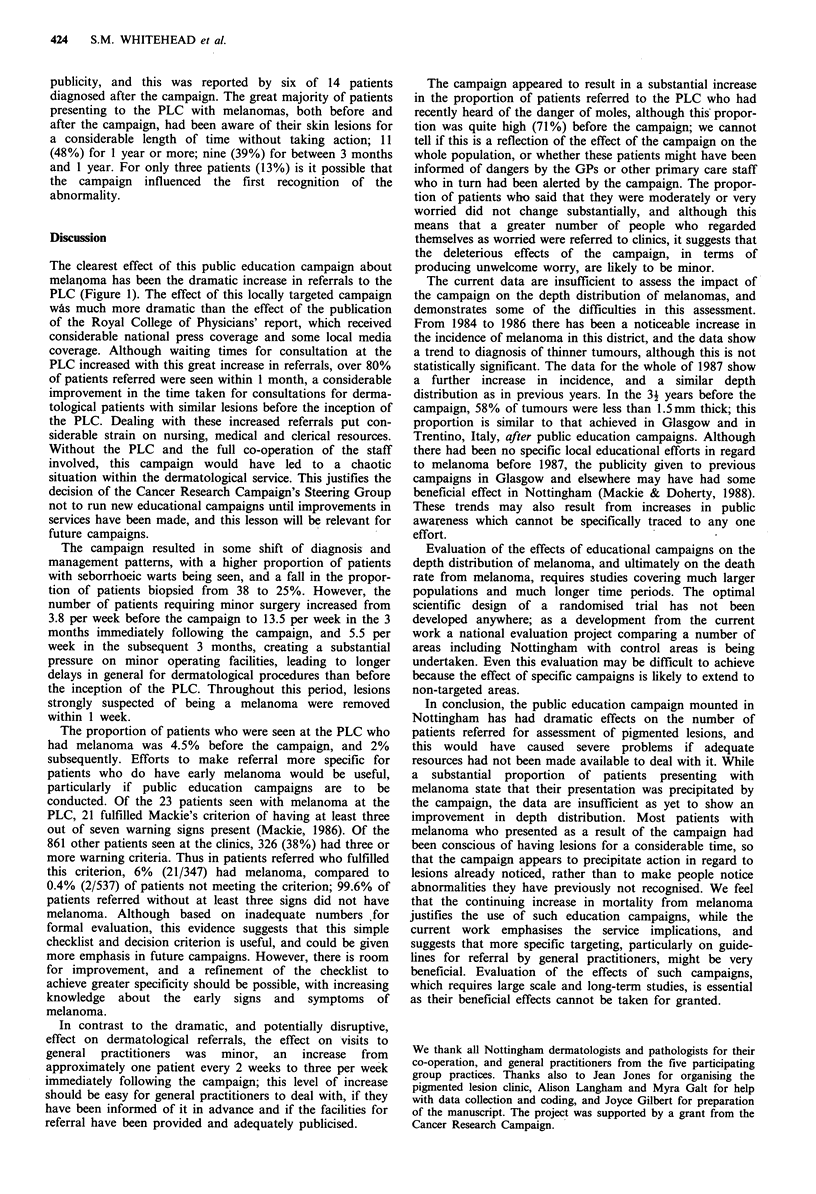
As part of a national campaign to combat the rising incidence of and mortality from cutaneous malignant melanoma, a programme of improved clinical services and professional and public education was set up in Nottingham in January to July 1987. The public education campaign in July led to an immediate increase in the weekly number of referrals to the pigmented lesion clinic from 10 to 54. The effect on general practitioner workload was less dramatic, the weekly number of consultations for discrete pigmented lesions rising from 0.5 to 3. In materials sent to GPs, we recommended that patients with three or more of seven specified signs should be referred for specialist opinion. Only 40% of the patients referred to the pigmented lesion clinic fulfilled this criterion, but 6% of these patients had a melanoma, compared to only 0.4% of those who did not meet the criterion. In the 6 months following the campaign, 64% of melanomas diagnosed in Nottingham residents had a Breslow thickness of less than 1.5 mm whereas only four (16%) were greater than 3.5 mm. However, this distribution was not significantly different from that seen in the three and a half years before the campaign. These results suggest that attempts to improve early diagnosis of the disease by health education are justified, but, in view of the service implications, full evaluation of such campaigns by large scale and long-term studies is essential. Future campaigns should give greater stress to referral criteria.
Full text
PDF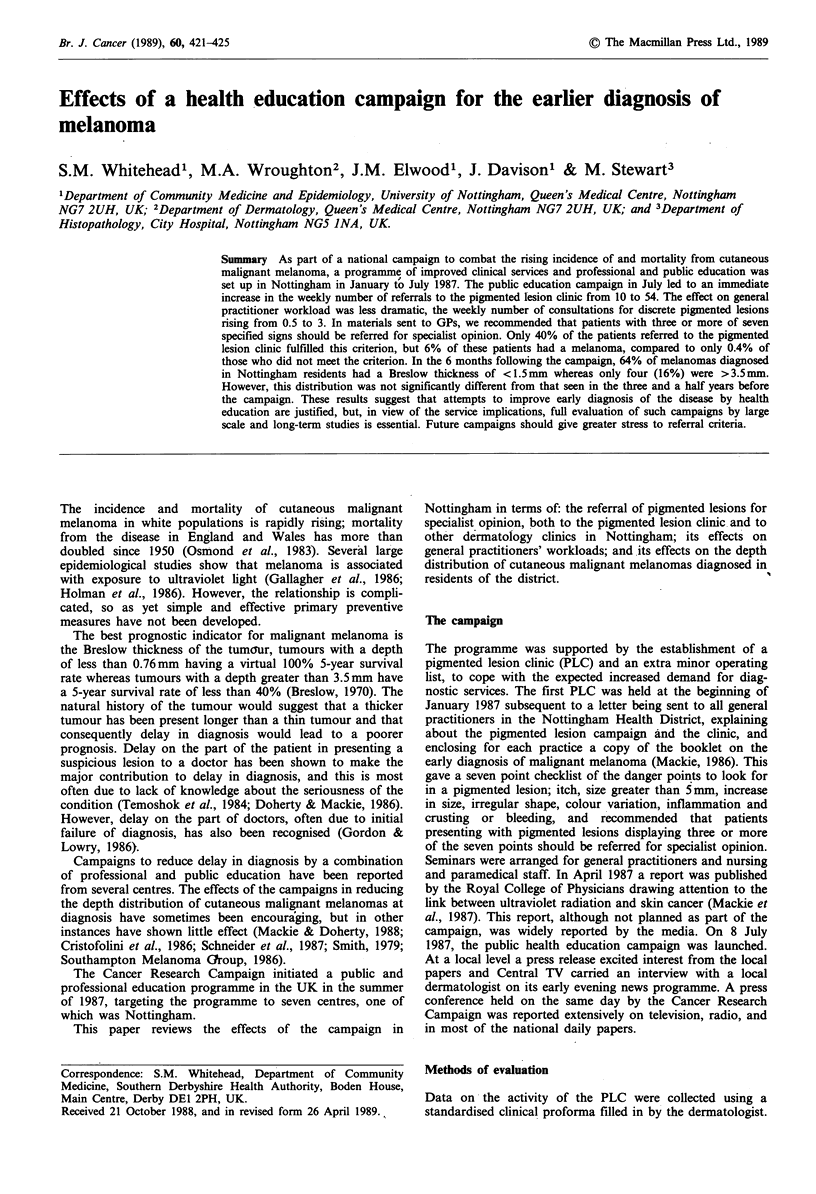
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Breslow A. Thickness, cross-sectional areas and depth of invasion in the prognosis of cutaneous melanoma. Ann Surg. 1970 Nov;172(5):902–908. doi: 10.1097/00000658-197011000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristofolini M., Zumiani G., Boi S., Piscioli F. Community detection of early melanoma. Lancet. 1986 Jan 18;1(8473):156–156. doi: 10.1016/s0140-6736(86)92292-0. [DOI] [PubMed] [Google Scholar]
- Doherty V. R., MacKie R. M. Reasons for poor prognosis in British patients with cutaneous malignant melanoma. Br Med J (Clin Res Ed) 1986 Apr 12;292(6526):987–989. doi: 10.1136/bmj.292.6526.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gallagher R. P., Elwood J. M., Hill G. B. Risk factors for cutaneous malignant melanoma: the Western Canada Melanoma Study. Recent Results Cancer Res. 1986;102:38–55. doi: 10.1007/978-3-642-82641-2_4. [DOI] [PubMed] [Google Scholar]
- Gordon L. G., Lowry W. S. Missed malignant melanomas. Br Med J (Clin Res Ed) 1986 Jun 7;292(6534):1524–1525. doi: 10.1136/bmj.292.6534.1524-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schneider J. S., Sagebiel R. W., Moore D. H., 2nd, Lawton G. M. Melanoma surveillance and earlier diagnosis. Lancet. 1987 Jun 20;1(8547):1435–1435. doi: 10.1016/s0140-6736(87)90625-8. [DOI] [PubMed] [Google Scholar]
- Smith T. The Queensland Melanoma Project--an exercise in health education. Br Med J. 1979 Jan 27;1(6158):253–254. doi: 10.1136/bmj.1.6158.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Temoshok L., DiClemente R. J., Sweet D. M., Blois M. S., Sagebiel R. W. Factors related to patient delay in seeking medical attention for cutaneous malignant melanoma. Cancer. 1984 Dec 15;54(12):3048–3053. doi: 10.1002/1097-0142(19841215)54:12<3048::aid-cncr2820541239>3.0.co;2-m. [DOI] [PubMed] [Google Scholar]


