Abstract
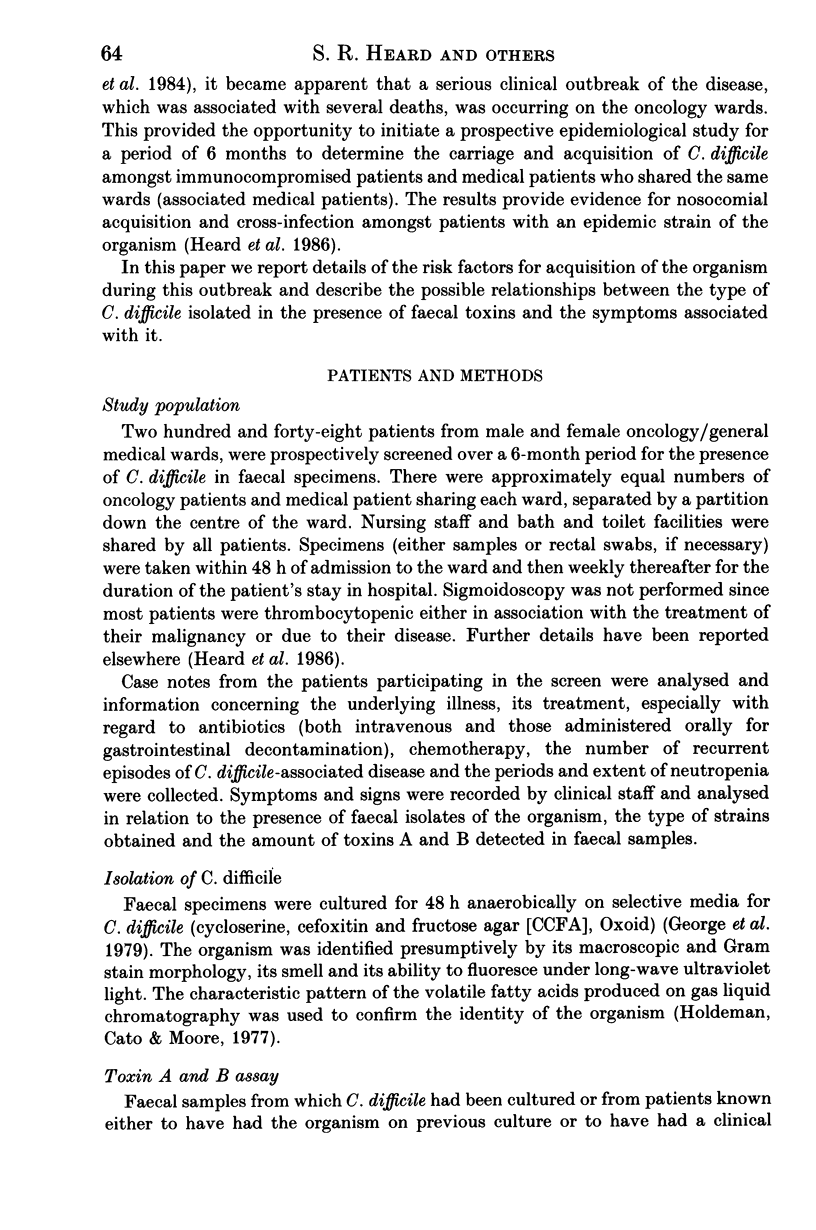
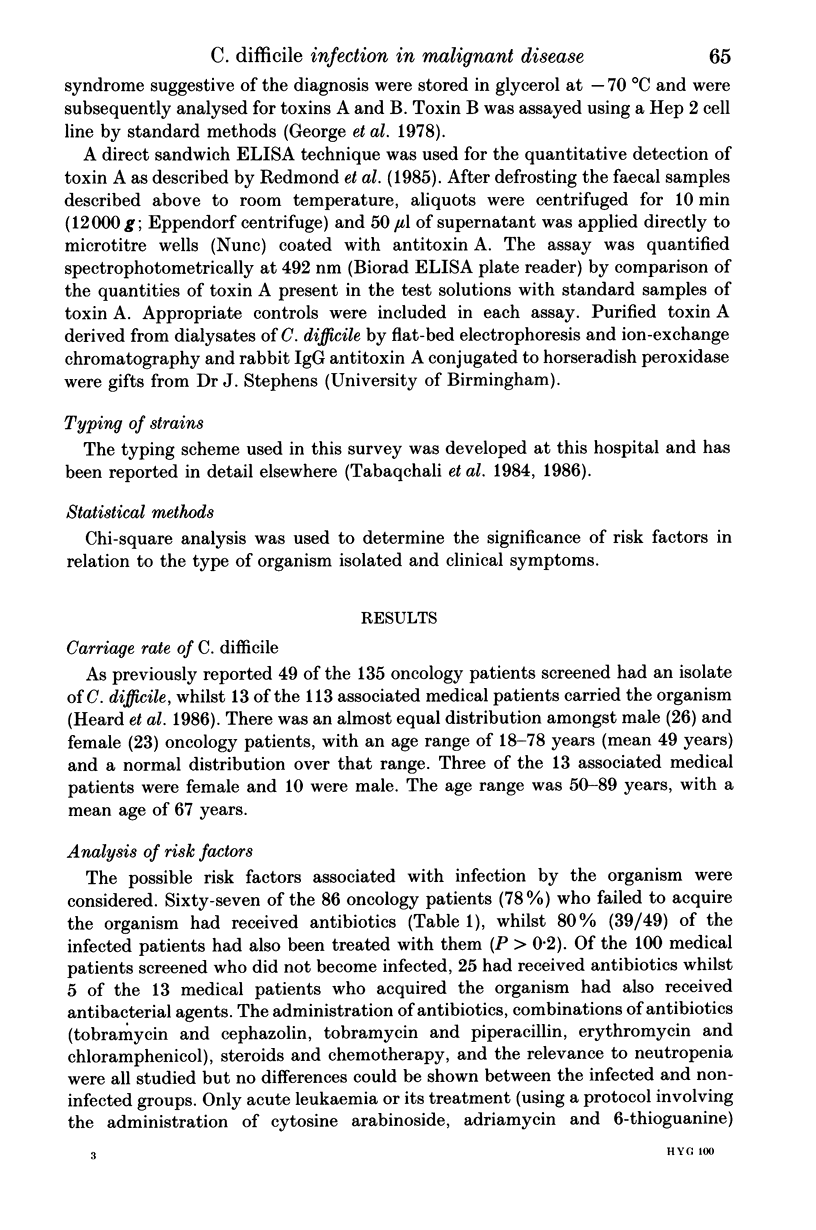
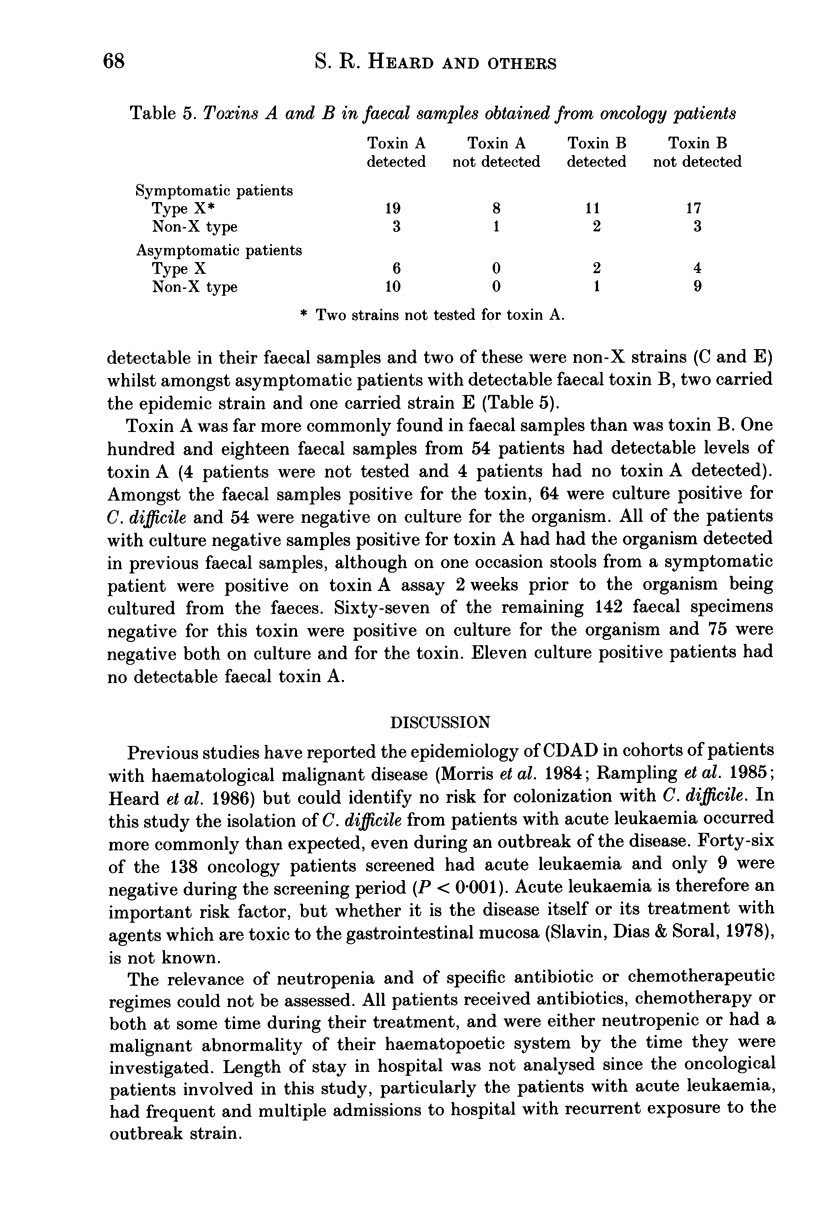
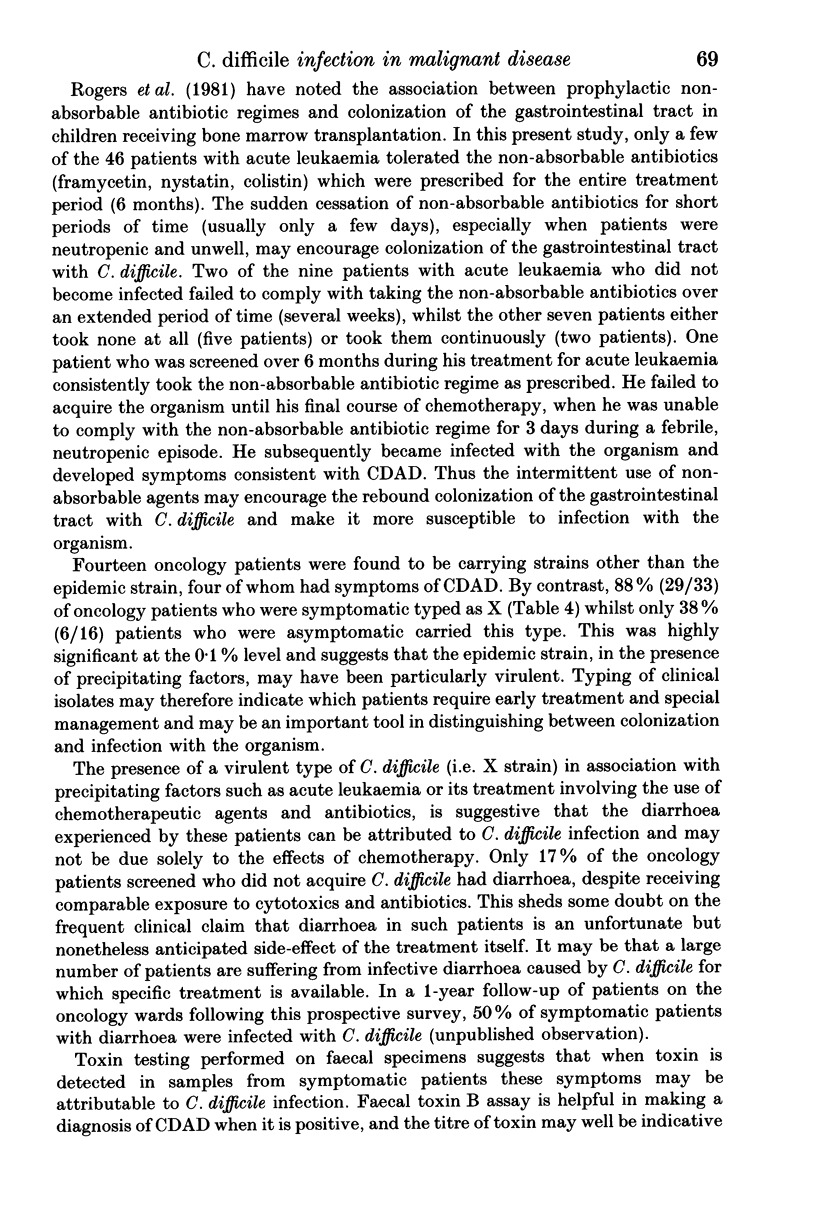
Two hundred and forty-eight patients from shared oncology and general medical wards were prospectively studied over a 6-month period for carriage of Clostridium difficile during an outbreak of clinical disease with an epidemic strain of the organism. Risk factors for infection were assessed. Acute leukaemia and/or its treatment were identified as significantly increasing the risk of infection. The relationship between the type of C. difficile isolated (as defined by a typing system based on the incorporation of [35S]methionine into bacterial proteins followed by gel electrophoresis), the presence of faecal toxins A and B and clinical symptoms were analysed. Carriage of the epidemic strain, type X, had a significant association with symptoms amongst oncology patients, with two thirds of these patients having detectable faecal toxin A and one third detectable faecal toxin B. During an outbreak of C. difficile-associated disease, typing the organism and assaying for both faecal toxins in symptomatic patients may be of benefit in determining which patients require specific, urgent treatment.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Burdon D. W., George R. H., Mogg G. A., Arabi Y., Thompson H., Johnson M., Alexander-Williams J., Keighley M. R. Faecal toxin and severity of antibiotic-associated pseudomembranous colitis. J Clin Pathol. 1981 May;34(5):548–551. doi: 10.1136/jcp.34.5.548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delmee M., Homel M., Wauters G. Serogrouping of Clostridium difficile strains by slide agglutination. J Clin Microbiol. 1985 Mar;21(3):323–327. doi: 10.1128/jcm.21.3.323-327.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fainstein V., Bodey G. P., Fekety R. Relapsing pseudomembranous colitis associated with cancer chemotherapy. J Infect Dis. 1981 Jun;143(6):865–865. doi: 10.1093/infdis/143.6.865. [DOI] [PubMed] [Google Scholar]
- George R. H., Symonds J. M., Dimock F., Brown J. D., Arabi Y., Shinagawa N., Keighley M. R., Alexander-Williams J., Burdon D. W. Identification of Clostridium difficile as a cause of pseudomembranous colitis. Br Med J. 1978 Mar 18;1(6114):695–695. doi: 10.1136/bmj.1.6114.695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- George W. L., Sutter V. L., Citron D., Finegold S. M. Selective and differential medium for isolation of Clostridium difficile. J Clin Microbiol. 1979 Feb;9(2):214–219. doi: 10.1128/jcm.9.2.214-219.1979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heard S. R., O'Farrell S., Holland D., Crook S., Barnett M. J., Tabaqchali S. The epidemiology of Clostridium difficile with use of a typing scheme: nosocomial acquisition and cross-infection among immunocompromised patients. J Infect Dis. 1986 Jan;153(1):159–162. doi: 10.1093/infdis/153.1.159. [DOI] [PubMed] [Google Scholar]
- Keighley M. R., Burdon D. W., Arabi Y., Williams J. A., Thompson H., Youngs D., Johnson M., Bentley S., George R. H., Mogg G. A. Randomised controlled trial of vancomycin for pseudomembranous colitis and postoperative diarrhoea. Br Med J. 1978 Dec 16;2(6153):1667–1669. doi: 10.1136/bmj.2.6153.1667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim K. H., Fekety R., Batts D. H., Brown D., Cudmore M., Silva J., Jr, Waters D. Isolation of Clostridium difficile from the environment and contacts of patients with antibiotic-associated colitis. J Infect Dis. 1981 Jan;143(1):42–50. doi: 10.1093/infdis/143.1.42. [DOI] [PubMed] [Google Scholar]
- Malamou-Ladas H., O'Farrell S., Nash J. Q., Tabaqchali S. Isolation of Clostridium difficile from patients and the environment of hospital wards. J Clin Pathol. 1983 Jan;36(1):88–92. doi: 10.1136/jcp.36.1.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris J. G., Jr, Jarvis W. R., Nunez-Montiel O. L., Towns M. L., Thompson F. S., Dowell V. R., Hill E. O., Vogler W. R., Winton E. F., Hughes J. M. Clostridium difficile. Colonization and toxin production in a cohort of patients with malignant hematologic disorders. Arch Intern Med. 1984 May;144(5):967–969. doi: 10.1001/archinte.144.5.967. [DOI] [PubMed] [Google Scholar]
- Rampling A., Warren R. E., Bevan P. C., Hoggarth C. E., Swirsky D., Hayhoe F. G. Clostridium difficile in haematological malignancy. J Clin Pathol. 1985 Apr;38(4):445–451. doi: 10.1136/jcp.38.4.445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rogers T. R., Petrou M., Lucas C., Chung J. T., Barrett A. J., Borriello S. P., Honour P. Spread of Clostridium difficile among patients receiving non-absorbable antibiotics for gut decontamination. Br Med J (Clin Res Ed) 1981 Aug 8;283(6288):408–409. doi: 10.1136/bmj.283.6288.408-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Slavin R. E., Dias M. A., Saral R. Cytosine arabinoside induced gastrointestinal toxic alterations in sequential chemotherapeutic protocols: a clinical-pathologic study of 33 patients. Cancer. 1978 Oct;42(4):1747–1759. doi: 10.1002/1097-0142(197810)42:4<1747::aid-cncr2820420413>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- Tabaqchali S., Holland D., O'Farrell S., Silman R. Typing scheme for Clostridium difficile: its application in clinical and epidemiological studies. Lancet. 1984 Apr 28;1(8383):935–938. doi: 10.1016/s0140-6736(84)92392-4. [DOI] [PubMed] [Google Scholar]
- Tabaqchali S., O'Farrell S., Holland D., Silman R. Method for the typing of Clostridium difficile based on polyacrylamide gel electrophoresis of [35S]methionine-labeled proteins. J Clin Microbiol. 1986 Jan;23(1):197–198. doi: 10.1128/jcm.23.1.197-198.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tedesco F. J. Pseudomembranous colitis: pathogenesis and therapy. Med Clin North Am. 1982 May;66(3):655–664. doi: 10.1016/s0025-7125(16)31413-4. [DOI] [PubMed] [Google Scholar]
- Viscidi R., Willey S., Bartlett J. G. Isolation rates and toxigenic potential of Clostridium difficile isolates from various patient populations. Gastroenterology. 1981 Jul;81(1):5–9. [PubMed] [Google Scholar]
- Wilkins T., Krivan H., Stiles B., Carman R., Lyerly D. Clostridial toxins active locally in the gastrointestinal tract. Ciba Found Symp. 1985;112:230–241. doi: 10.1002/9780470720936.ch13. [DOI] [PubMed] [Google Scholar]
- Wilson K. H., Sheagren J. N. Antagonism of toxigenic Clostridium difficile by nontoxigenic C. difficile. J Infect Dis. 1983 Apr;147(4):733–736. doi: 10.1093/infdis/147.4.733. [DOI] [PubMed] [Google Scholar]


