Abstract
The recent finding that inhibitors of PI3/Akt can sensitize HIV infected macrophages to oxidative stress-induced cell death suggest a potential new therapeutic approach to targeting HIV reservoirs.
Although antiretroviral therapy has achieved laudable successes in combating HIV, particularly since the advent of protease inhibitors in the mid 1990s, fully successful treatment remains plagued by multiple, clinically latent viral reservoirs largely impervious to antiretroviral drugs. The microbiology of clinical latency is controversial and may involve elements of viral quiescence (expression of no – or a limited subset of – viral genes) as well as low level viral replication in protected cell types or anatomical compartments [1]. Viral persistence has been reported in brain cells (including perivascular macrophages, parenchymal microglial cells and astrocytes), NK cells, renal tubular cells, mononuclear cells from semen, follicular dendritic cells, cells of the monocyte/macrophage lineage (recently infected monocytes and tissue macrophages) and resting CD4+ T cells, with the latter two being the best known reservoirs [2-5].
Attempts at attacking the resting CD4+T cell HIV reservoir have generally involved induction (of presumably quiescent virus) with IL-2, IL-7, phorbol esters, or valproic acid [3,6,7]. Such induction approaches usually assume the activated, HIV producing cells will be killed directly by the induced virus or by the host immune system but some have attempted bolstering these effects by targeting immunotoxins to viral determinants [7]. The risk of a spreading infection by virus newly induced to replicate is generally mitigated in these scenarios by HAART.
Attacking the macrophage HIV reservoir has proven a thornier issue. From the virus's standpoint macrophages are an ideal reservoir cell because they are long lived, because HIV does not kill macrophages by direct lysis, as it does CD4+T cells, and because virus production by chronically infected macrophages tends to be relatively insensitive to a variety of antiretroviral agents [8-13]. Besides hosting a significant virus reservoir, chronically infected macrophages and/or their brain counterparts, microglia, may contribute to pathogenesis through chronic aberrant release of a variety of host and viral cytoactive factors and may be subject to chronic dysregulation through aberrant expression of surface receptors [14-20]. Thus, the recent report that PI3K/Akt inhibitors can drastically sensitize HIV infected macrophages to oxidative-stress-induced cell death [21] is welcome news as delineating a possible novel therapeutic approach.
HIV infection in vivo increases levels of superoxide anion and peroxynitrite, the latter of which can promote HIV replication in macrophages[22]. Recently Chugh et al. [23] reported that HIV infection activated the PI3K/Akt pathway exerting a cytoprotective effect against apoptotic challenge in a microglial cell line and in primary human macrophages. This described a pathway by which HIV could protect certain HIV infected cells against the oxidative stress they typically endure in vivo due to the high levels of nitric oxide (NO) they produce [24-27]. The finding that a variety of PI3K/Akt inhibitors, including wortmannin, Akt inhibitors IV & VIII (Calbiochem) and the clinically available Miltefosine could all promote cell death in cultures of primary human macrophages infected with HIV, but not in uninfected controls, makes therapeutically attacking the HIV macrophage/microglial reservoir a tantalizing possibility.
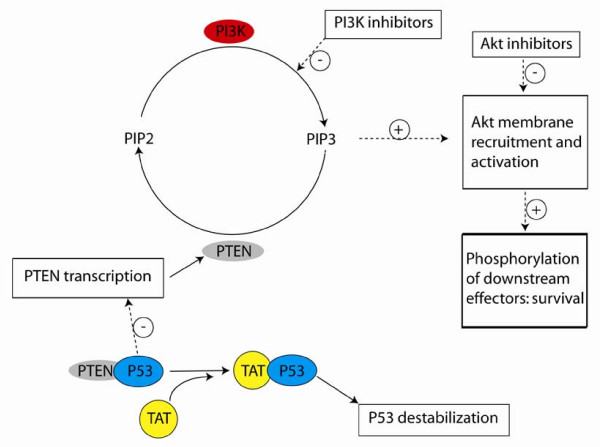
Recent work has contributed significantly to understanding the roles of numerous HIV regulatory proteins in cells of lineages other than the T lineage [22,28,29] and the work highlighted here is no exception. Mechanistic studies determined that the HIV Tat can mediate the activation of the PI3K/Akt pathway, dependent upon the Tat basic domain (a region that binds p53 [21,23]) and that the mediation is associated with a drop in the level of PTEN (phosphatase tensin homolog) protein expression. SIV Tat was also shown to mediate the cytoprotective effect (in a microglial cell line), suggesting an evolutionarily conserved role. The results are consistent with a model in which Tat competes with PTEN for p53 binding, causing p53 destabilization and a consequent reduction in PTEN mRNA and protein levels, relieving the PTEN inhibition of Akt activation (Figure 1).
Figure 1.
Proposed pathways [21] describing the effects of Tat and PI3K/Akt inhibitors on macrophage resistance to oxidative stress. Solid lines represent the flux of indicated molecular species. Dashed lines represent stimulatory (+) or inhibitory (-) regulation. Boxes enclose summaries of processes or effects.
Missing from the current in vitro findings is evidence that endogenous production of reactive oxygen species (ROS) in HIV infected macrophages or microglia is sufficient to render them more susceptible than uninfected control cells to oxidative stress-induced cell death [30,31]. Rather, exogenous NO must be provided in vitro (in the form of sodium nitroprusside) [21,23]. Thus, for the suggested approach to succeed clinically, either in vivo levels of ROS in critical local compartments must be sufficient to cause death when the Akt pathway is inhibited – the likelihood of which is undetermined – or such levels of ROS must be induced – which is problematic. Time will tell.
Acknowledgments
Acknowledgements
The author thanks Indira Hewlett for a critical reading of the manuscript. The findings and conclusion in this article have not been formally disseminated by the Food and Drug Administration and should not be construed to represent any Agency determination or policy.
References
- Sedaghat AR, Siliciano RF, Wilke CO. Low-level HIV-1 replication and the dynamics of the resting CD4+ T cell reservoir for HIV-1 in the setting of HAART. BMC Infect Dis. 2008;8:2. doi: 10.1186/1471-2334-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe S, Zhu T, Muller WA. The contribution of monocyte infection and trafficking to viral persistence, and maintenance of the viral reservoir in HIV infection. J Leukoc Biol. 2003;74:635–641. doi: 10.1189/jlb.0503204. [DOI] [PubMed] [Google Scholar]
- Dybul M, Daucher M, Jensen MA, Hallahan CW, Chun TW, Belson M, Hidalgo B, Nickle DC, Yoder C, Metcalf JA, Davey RT, Ehler L, Kress-Rock D, Nies-Kraske E, Liu S, Mullins JI, Fauci AS. Genetic characterization of rebounding human immunodeficiency virus type 1 in plasma during multiple interruptions of highly active antiretroviral therapy. J Virol. 2003;77:3229–3237. doi: 10.1128/JVI.77.5.3229-3237.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Popovic M, Tenner-Racz K, Pelser C, Stellbrink HJ, van Lunzen J, Lewis G, Kalyanaraman VS, Gallo RC, Racz P. Persistence of HIV-1 structural proteins and glycoproteins in lymph nodes of patients under highly active antiretroviral therapy. Proc Natl Acad Sci U S A. 2005;102:14807–14812. doi: 10.1073/pnas.0506857102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhoopat L, Rithaporn TS, Khunamornpong S, Bhoopat T, Taylor CR, Thorner PS. Cell reservoirs in lymph nodes infected with HIV-1 subtype E differ from subtype B: identification by combined in situ polymerase chain reaction and immunohistochemistry. Mod Pathol. 2006;19:255–263. doi: 10.1038/modpathol.3800527. [DOI] [PubMed] [Google Scholar]
- Siliciano JD, Lai J, Callender M, Pitt E, Zhang H, Margolick JB, Gallant JE, Cofrancesco J, Jr., Moore RD, Gange SJ, Siliciano RF. Stability of the latent reservoir for HIV-1 in patients receiving valproic acid. J Infect Dis. 2007;195:833–836. doi: 10.1086/511823. [DOI] [PubMed] [Google Scholar]
- Brooks DG, Hamer DH, Arlen PA, Gao L, Bristol G, Kitchen CM, Berger EA, Zack JA. Molecular characterization, reactivation, and depletion of latent HIV. Immunity. 2003;19:413–423. doi: 10.1016/S1074-7613(03)00236-X. [DOI] [PubMed] [Google Scholar]
- Aquaro S, Bagnarelli P, Guenci T, De Luca A, Clementi M, Balestra E, Calio R, Perno CF. Long-term survival and virus production in human primary macrophages infected by human immunodeficiency virus. J Med Virol. 2002;68:479–488. doi: 10.1002/jmv.10245. [DOI] [PubMed] [Google Scholar]
- Schmidtmayerova H, Nottet HS, Nuovo G, Raabe T, Flanagan CR, Dubrovsky L, Gendelman HE, Cerami A, Bukrinsky M, Sherry B. Human immunodeficiency virus type 1 infection alters chemokine beta peptide expression in human monocytes: implications for recruitment of leukocytes into brain and lymph nodes. Proc Natl Acad Sci U S A. 1996;93:700–704. doi: 10.1073/pnas.93.2.700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meltzer MS, Skillman DR, Gomatos PJ, Kalter DC, Gendelman HE. Role of mononuclear phagocytes in the pathogenesis of human immunodeficiency virus infection. Annu Rev Immunol. 1990;8:169–194. doi: 10.1146/annurev.iy.08.040190.001125. [DOI] [PubMed] [Google Scholar]
- Gartner S, Markovits P, Markovitz DM, Kaplan MH, Gallo RC, Popovic M. The role of mononuclear phagocytes in HTLV-III/LAV infection. Science. 1986;233:215–219. doi: 10.1126/science.3014648. [DOI] [PubMed] [Google Scholar]
- Aquaro S, Calio R, Balzarini J, Bellocchi MC, Garaci E, Perno CF. Macrophages and HIV infection: therapeutical approaches toward this strategic virus reservoir. Antiviral Res. 2002;55:209–225. doi: 10.1016/S0166-3542(02)00052-9. [DOI] [PubMed] [Google Scholar]
- Perno CF, Aquaro S, Rosenwirth B, Balestra E, Peichl P, Billich A, Villani N, Calio R. In vitro activity of inhibitors of late stages of the replication of HIV in chronically infected macrophages. J Leukoc Biol. 1994;56:381–386. doi: 10.1002/jlb.56.3.381. [DOI] [PubMed] [Google Scholar]
- Zhang M, Li X, Pang X, Ding L, Wood O, Clouse K, Hewlett I, Dayton AI. Identification of a potential HIV-induced source of bystander-mediated apoptosis in T cells: upregulation of trail in primary human macrophages by HIV-1 tat. J Biomed Sci. 2001;8:290–296. doi: 10.1007/BF02256603. [DOI] [PubMed] [Google Scholar]
- Zhang M, Drenkow J, Lankford CS, Frucht DM, Rabin RL, Gingeras TR, Venkateshan C, Schwartzkopff F, Clouse KA, Dayton AI. HIV regulation of the IL-7R: a viral mechanism for enhancing HIV-1 replication in human macrophages in vitro. J Leukoc Biol. 2006;79:1328–1338. doi: 10.1189/jlb.0704424. [DOI] [PubMed] [Google Scholar]
- Khati M, James W, Gordon S. HIV-macrophage interactions at the cellular and molecular level. Arch Immunol Ther Exp (Warsz) 2001;49:367–378. [PubMed] [Google Scholar]
- Singh IN, Goody RJ, Dean C, Ahmad NM, Lutz SE, Knapp PE, Nath A, Hauser KF. Apoptotic death of striatal neurons induced by human immunodeficiency virus-1 Tat and gp120: Differential involvement of caspase-3 and endonuclease G. J Neurovirol. 2004;10:141–151. doi: 10.1080/13550280490441103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi B, Raina J, Lorenzo A, Busciglio J, Gabuzda D. Neuronal apoptosis induced by HIV-1 Tat protein and TNF-alpha: potentiation of neurotoxicity mediated by oxidative stress and implications for HIV-1 dementia. J Neurovirol. 1998;4:281–290. doi: 10.3109/13550289809114529. [DOI] [PubMed] [Google Scholar]
- Mattson MP, Haughey NJ, Nath A. Cell death in HIV dementia. Cell Death Differ. 2005;12 Suppl 1:893–904. doi: 10.1038/sj.cdd.4401577. [DOI] [PubMed] [Google Scholar]
- Kruman. Nath A, Mattson MP. HIV-1 protein Tat induces apoptosis of hippocampal neurons by a mechanism involving caspase activation, calcium overload, and oxidative stress. Exp Neurol. 1998;154:276–288. doi: 10.1006/exnr.1998.6958. [DOI] [PubMed] [Google Scholar]
- Chugh P, Bradel-Tretheway B, Monteiro-Filh CMR, Planelles V, Maggirwar SB, Dewhurst S, Kim B. Akt inhibitors as an HIV-1 infected macrophage-specific anti-viral therapy. Retrovirology. 2008;5:11. doi: 10.1186/1742-4690-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aquaro S, Muscoli C, Ranazzi A, Pollicita M, Granato T, Masuelli L, Modesti A, Perno CF, Mollace V. The contribution of peroxynitrite generation in HIV replication in human primary macrophages. Retrovirology. 2007;4:76. doi: 10.1186/1742-4690-4-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chugh P, Fan S, Planelles V, Maggirwar SB, Dewhurst S, Kim B. Infection of human immunodeficiency virus and intracellular viral Tat protein exert a pro-survival effect in a human microglial cell line. J Mol Biol. 2007;366:67–81. doi: 10.1016/j.jmb.2006.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kan H, Xie Z, Finkel MS. HIV gp120 enhances NO production by cardiac myocytes through p38 MAP kinase-mediated NF-kappaB activation. Am J Physiol Heart Circ Physiol. 2000;279:H3138–43. doi: 10.1152/ajpheart.2000.279.6.H3138. [DOI] [PubMed] [Google Scholar]
- Polazzi E, Levi G, Minghetti L. Human immunodeficiency virus type 1 Tat protein stimulates inducible nitric oxide synthase expression and nitric oxide production in microglial cultures. J Neuropathol Exp Neurol. 1999;58:825–831. doi: 10.1097/00005072-199908000-00005. [DOI] [PubMed] [Google Scholar]
- Zhao ML, Kim MO, Morgello S, Lee SC. Expression of inducible nitric oxide synthase, interleukin-1 and caspase-1 in HIV-1 encephalitis. J Neuroimmunol. 2001;115:182–191. doi: 10.1016/S0165-5728(00)00463-X. [DOI] [PubMed] [Google Scholar]
- Reynolds A, Laurie C, Mosley RL, Gendelman HE. Oxidative stress and the pathogenesis of neurodegenerative disorders. Int Rev Neurobiol. 2007;82:297–325. doi: 10.1016/S0074-7742(07)82016-2. [DOI] [PubMed] [Google Scholar]
- Goujon C, Riviere L, Jarrosson-Wuilleme L, Bernaud J, Rigal D, Darlix JL, Cimarelli A. SIVSM/HIV-2 Vpx proteins promote retroviral escape from a proteasome-dependent restriction pathway present in human dendritic cells. Retrovirology. 2007;4:2. doi: 10.1186/1742-4690-4-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jacquot G, le Rouzic E, David A, Mazzolini J, Bouchet J, Bouaziz S, Niedergang F, Pancino G, Benichou S. Localization of HIV-1 Vpr to the nuclear envelope: Impact on Vpr functions and virus replication in macrophages. Retrovirology. 2007;4:84. doi: 10.1186/1742-4690-4-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palamara AT, Perno CF, Aquaro S, Bue MC, Dini L, Garaci E. Glutathione inhibits HIV replication by acting at late stages of the virus life cycle. AIDS Res Hum Retroviruses. 1996;12:1537–1541. doi: 10.1089/aid.1996.12.1537. [DOI] [PubMed] [Google Scholar]
- Garaci E, Aquaro S, Lapenta C, Amendola A, Spada M, Covaceuszach S, Perno CF, Belardelli F. Anti-nerve growth factor Ab abrogates macrophage-mediated HIV-1 infection and depletion of CD4+ T lymphocytes in hu-SCID mice. Proc Natl Acad Sci U S A. 2003;100:8927–8932. doi: 10.1073/pnas.1332627100. [DOI] [PMC free article] [PubMed] [Google Scholar]