Abstract
Purpose
In patients with advanced colorectal cancer, FOLFIRI is considered as one of the reference first-line treatments. However, only about half of treated patients respond to this bi-therapy, and there is no clinically useful marker that predicts response. A major clinical challenge is to identify the subset of patients who could benefit from this chemotherapy. We aimed at identifying a gene expression profile in primary colon cancer tissue that could predict chemotherapy response.
Patients and Methods
Tumor colon samples from 21 patients with advanced colorectal cancer were analysed for gene expression profiling using Human Genome GeneChip® arrays U133. At the end of the first-line treatment, the best observed response according to WHO criteria, was used to define the responder and non-responder patients. Discriminatory genes were first selected by the significance analysis of microarrays algorithm and the area under the receiver operating characteristic curve. A predictor classifier was then constructed using support vector machines. Finally, leave-one-out cross validation was used to estimate the performance and the accuracy of the output class prediction rule.
Results
We determined a set of 14 predictor genes of response to FOLFIRI. Nine of 9 responders (100% specificity) and 11 of 12 non-responders (92% sensitivity) were correctly classified, for an overall accuracy of 95%.
Conclusion
After validation in an independent cohort of patients, our gene signature could be used as a decision tool to assist oncologists in selecting colorectal cancer patients who could benefit from FOLFIRI chemotherapy, both in the adjuvant and the first-line metastatic setting.
Keywords: Aged, Antineoplastic Combined Chemotherapy Protocols, administration & dosage, therapeutic use, Camptothecin, administration & dosage, analogs & derivatives, Colorectal Neoplasms, drug therapy, genetics, Female, Fluorouracil, administration & dosage, Gene Expression Profiling, Humans, Leucovorin, administration & dosage, Male, Middle Aged
INTRODUCTION
Colorectal cancer (CRC) is one of the most common malignant diseases with 945 000 new cases every year and is the fourth cause of cancer-related deaths worldwide.1 When localized, CRC is often curable by surgery, but the prognosis for patients with metastatic disease remains poor. Curative-intent resections can be performed on only 10–15% of liver metastases. In the majority of metastatic patients, the standard treatment remains palliative chemotherapy. Fluorouracil-based therapy has been the main treatment for metastatic colorectal cancer for the last 40 years. Major progress has been made by the introduction of regimens containing new cytotoxic drugs such as irinotecan2 or oxaliplatin.3 The combinations commonly used, e.g., FOLFIRI (leucovorin, fluorouracil, and irinotecan) and FOLFOX (leucovorin, fluorouracil, and oxaliplatin) can reach an objective response rate of about 50%.4,5 However, these new combinations remain inactive in about half of the patients, and in addition, resistance to treatment appears in almost all patients who were initially responders. More recently, two monoclonal antibodies targeting the vascular endothelial growth factor (bevacizumab) and the epidermal growth factor receptor (cetuximab) have been approved for treatment of metastatic colorectal cancer but only in combination with standard chemotherapy regimens.6,7
A major clinical challenge is to identify a subset of patients who could benefit from chemotherapy, both in metastatic and adjuvant settings. There have been many attempts to determine predictive factors for response. Alterations in gene expression, protein expression and polymorphic variants in genes encoding thymidylate synthase, dihydropyrimidine dehydrogenase, and thymidine phosphorylase have been reported to predict response to fluorouracil.8–10 In addition, microsatellite-instability status could be an independent predictor of fluorouracil-based adjuvant chemotherapy,11 and topoisomerase I expression has been investigated as a predictive factor for response to irinotecan.12 High mRNA expression of excision repair cross-complementing 1 (ERCC1) and thymidylate synthase have shown to be predictive of poor response to treatment of advanced disease with oxaliplatin and fluorouracil.13 However, although predictive factor testing is an exciting field of research, it has not yet been routinely applied in clinical practice.14,15 Furthermore, an in vitro study on prediction of response of colon cancer cells demonstrated that the measurement of multiple rather than single marker genes resulted in a more accurate assessment of drug response.16
Gene expression profiling has become a strategy to predict clinical outcome or to classify molecular tumor subtypes. Several studies have already been conducted, showing the feasibility of identifying genes involved in the progression and the prognosis of colorectal cancer17–21 or for predicting drug-response in other cancer types, notably in breast cancer.22–24 However, no indication on the possible added value of this approach for predicting drug response in colon cancer has been reported.25 Only a recent study showed that gene expression profiling might contribute to the response prediction of rectal adenocarcinomas to preoperative chemoradiotherapy.26
In this report, our objective was to build a predictor classifier for response to FOLFIRI treatment in patients with advanced colorectal using microarray gene expression profiles of primary colon cancer tissue.
PATIENTS AND METHODS
Patients, and sample collection
From January 2000 to June 2004, we enrolled in a prospective study 40 colorectal cancer patients with synchronous and unresectable liver metastases at the Val d’Aurelle Regional Cancer center. The eligibility criteria for inclusion were: histologically proven adenocarcinoma of the colon; advanced and bidimensionally measurable disease; age 18 to 75 years, WHO performance status of 2 or less. All patients were chemonaive. Liver metastases were determined as unresectable when there was an impossibility of performing resection of all the lesions with clear margins or when there was an extrahepatic disease involvement.
Before receiving any chemotherapy, all patients underwent surgery for primary tumor resection independently of their symptomatic status. R0 resection was achieved in all patients. Colon tumor samples were collected at the time of surgery following a standardized procedure in order to obtain high quality RNA.27
The study was approved by our local ethical committee and all participating patients were informed of the study and had to provide signed written informed consent before enrolment.
Chemotherapy
Patients were treated with a combination of irinotecan with an LV5FU2 regimen (FOLFIRI), as first-line treatment. Ten patients participated in a multicenter phase II clinical trial aimed at assessing whether increasing the dose of irinotecan (from 180 to 260 mg/m2) in the FOLFIRI regimen would benefit patients with metastatic colorectal cancer. The remaining patients received a FOLFIRI regimen with a standard dose of irinotecan (180 mg/m2). For one patient, intravenous 5-FU was replaced by an oral form of 5-FU (uracil/ftorafur or UFT).
Tumor response was evaluated according to WHO recommendations for the evaluation of cancer treatment in solid tumors.28 The size of the metastatic lesions was estimated from bidimensional measurements (the product of the longest diameter and the longest perpendicular diameter) using computed tomography scanning. Patients were evaluated for response before and after every 4 cycles of chemotherapy for a regimen of 3-week cycles and after every 6 cycles of chemotherapy for a regimen of 2-week cycles, to calculate the percent change from baseline. Best observed response was then used to classify patients into two groups. Patients with a decrease ≥ 50% of the metastatic lesion were classified as responders (R), and patients with a decrease < 50% or with an increase in size of lesions were classified as non-responders (NR).
RNA preparation and assessment of RNA quality
All tissue samples were maintained at −180°C (liquid nitrogen) until RNA extraction and were weighed before homogenization. Tissue samples were then disrupted directly into a lysis buffer using Mixer Mill® MM 300 (Qiagen, Valencia, CA). Total RNA was isolated from tissue lysates using the RNeasy® mini Kit (Qiagen), and additional DNAse digestion was performed on all samples during the extraction process (RNase-Free DNase Set™ Protocol for DNase treatment on RNeasy® Mini Spin Columns, Qiagen). After each extraction, a small fraction of the total RNA preparation was taken to determine the quality of the sample and the yield of total RNA. Controls were performed by UV spectroscopy and analysis of total RNA profile using the Agilent RNA 6000 Nano LabChip® Kit with the Agilent 2100 Bioanalyser (Agilent Technologies, Palo Alto, CA) to determine RNA purity, quantity, and integrity.
Gene expression analysis
First strand cDNA synthesis was generated using a T7-linked oligo-dT primer, followed by second strand synthesis. Labeled cRNA probes were then generated by reverse transcription followed by in vitro transcription, incorporating biotin labeling, as part of the standard Affymetrix protocol. For each sample, the probes were then hybridized to human genome U133 chips (Affymetrix Inc., Santa Clara, CA) containing over 45 000 qualifiers, corresponding to genes and expressed sequence tags (EST). After hybridization, the probes were scanned using a laser scanner, and signal intensity for each transcript and detection call (present, absent, or marginal) were determined using MAS 5.0 Software (Affymetrix). Inter-array normalization was performed using a set of internal standard genes (normalization set + internal controls) leading to the determination of a scaling factor.
Statistical analysis
To assess differences in clinicopathological features between responder and non-responder patients, Fisher’s exact test was used for qualitative variables with discrete categories and the Wilcoxon test was used for continuous variables. The Kaplan Meier method was used to calculate overall survival from the treatment start date to the date of death, or the date that the surviving patients were last seen.
To determine gene signature, we kept only gene called present in at least 50% of the patients from any one group. Data analysis was performed on the 19 365 expressed genes. Differentially expressed genes between responders and non-responders were detected by means of the significance analysis of microarrays algorithm (SAM).29 This approach calculates a d-score, which corresponds to a Student’s t statistic with a small positive constant added to the denominator. This value was chosen to minimize the coefficient of variation.
These genes were then classified according to this score and their statistical significance. A set of genes with a false discovery rate (FDR) of 20% were then selected.
The genes selected by the SAM algorithm were then ranked by computing the empirical area under the receiver operating characteristic (ROC) curve (AUC) and the empirical partial AUC (pAUC), which is restricted to a clinically relevant pertinent range of false-positive rates.30 The pAUC is an index of discrimination, and the chosen false positive rate interval allows considering a high specificity in order to particularly well detect the responder population. Then, the classification rule was defined with the support vector machines (SVM) algorithm.31 Two parameters were required, the radial basis function kernel method and the magnitude of the penalty for violating the soft margin. Finally, leave-one-out cross validation (LOOCV) was used to estimate the performance and accuracy of the output class prediction rule. With LOOCV, one sample is left out, and the remaining samples are used to construct a predictor classifier, which is used to classify the left-out sample.
RESULTS
Patients and clinical response
Of the 40 enrolled patients, only 27 were evaluable for tumor response to FOLFIRI as we excluded either patient who received another treatment or died before the first evaluation. Furthermore, five colon tumor samples were excluded on the basis of poor quality RNA (2), low quantity RNA (1), and poor chip expression quality (2). Two other samples were excluded from one patient who presented two different primary tumor sites. Of the 21 eligible patients, 9 (43%) were considered sensitive to FOLFIRI treatment and showed a size reduction of metastatic lesion ranging from 52% to 94% whereas 12 (57%) were considered as non-responders, with a tumor size decrease of not more than 44 % or a tumor size increase of up to 25% from nadir (table 1).
Table 1.
Evaluation of tumor response
| Identification of patients | % change in indicator lesion size | Response evaluation * | Status** |
|---|---|---|---|
| 130-YL | −94 | PR | R |
| 149-JG-I | −86 | PR | R |
| 016-MV | −84 | PR | R |
| 044-MB | −80 | PR | R |
| 022-JB | −79 | PR | R |
| 061-CM | −77 | PR | R |
| 115-CB | −69 | PR | R |
| 059-MT | −65 | PR | R |
| 244-FP | −52 | PR | R |
| 222-PEM | −44 | SD | NR |
| 119-PM | −39 | SD | NR |
| 223-GB | −29 | SD | NR |
| 196-TD | −27 | SD | NR |
| 73-PD | −20 | SD | NR |
| 189-JR | −19 | SD | NR |
| 94-AM | −15 | SD | NR |
| 056-MC | −14 | SD | NR |
| 213-RG | −4 | SD | NR |
| 045-JC | 0 | SD | NR |
| 227-SS | 0 | SD | NR |
| 89-NC | +25 | PD | NR |
PR=partial response (decrease≥50%), SD=stable disease (neither PR nor PD criterion met), PD=progression disease (increase≥25% or appearance of new lesions); PR has to be confirmed at 4 weeks.
R=responder; NR=non-responder
Patient and tumor characteristics did not differ significantly between the responder and non-responder groups (table 2) except for chemotherapy regimen. However, if the patient treated by UFT-CAMPTO chemotherapy schedule is excluded, the comparison between high dose and standard dose FOLFIRI regimen was at the limit of statistical significance (p = 0.07). Median overall survival was 21 months.
Table 2.
Clinical and pathological characteristics of patients
| Characteristics | Responders (n=9) | Non-responders (n=12) | Total (n=21) | ||||
|---|---|---|---|---|---|---|---|
| N | (%) | N | (%) | N | (%) | p | |
| Gender | |||||||
| Male | 3 | 33 | 8 | 67 | 11 | 52 | 0.20 |
| Female | 6 | 67 | 4 | 33 | 10 | 48 | |
| Age (years), median [min-max] | 57 [45–68] | 62 [50–71] | 60 [45–71] | 0.14 | |||
| Tumor localization | |||||||
| Right colon | 1 | 11 | 0 | 0 | 1 | 5 | 0.83 |
| Transverse colon | 1 | 11 | 1 | 8 | 2 | 9 | |
| Left colon | 7 | 78 | 10 | 84 | 17 | 81 | |
| Rectum-sigmoid junction | 0 | 0 | 1 | 8 | 1 | 5 | |
| Differentiation | |||||||
| Well | 5 | 56 | 4 | 33 | 9 | 43 | 0.91 |
| Moderate | 3 | 33 | 5 | 42 | 8 | 38 | |
| Poor | 1 | 11 | 2 | 17 | 3 | 14 | |
| ND* | 0 | 0 | 1 | 8 | 1 | 5 | |
| pN | |||||||
| pN0 | 1 | 11 | 3 | 25 | 4 | 19 | 0.84 |
| pN1 | 2 | 22 | 2 | 17 | 4 | 19 | |
| pN2 | 6 | 67 | 7 | 58 | 13 | 62 | |
| pT | |||||||
| pT3 | 8 | 89 | 8 | 67 | 16 | 76 | 0.34 |
| pT4 | 1 | 11 | 4 | 33 | 5 | 24 | |
| Number of metastatic sites | |||||||
| 1 | 9 | 100 | 9 | 75 | 18 | 86 | 0.49 |
| 2 | 0 | 0 | 2 | 17 | 2 | 9 | |
| 3 | 0 | 0 | 1 | 8 | 1 | 5 | |
| Chemotherapy schedule | |||||||
| FOLFIRI | 2 | 22 | 8 | 67 | 10 | 47.5 | 0.05 |
| High IRI | 7 | 78 | 3 | 25 | 10 | 47.5 | |
| UFT-CAMPTO | 0 | 0 | 1 | 8 | 1 | 5 | |
| WHO performance status | |||||||
| 0 | 4 | 44 | 5 | 42 | 9 | 43 | 1.00 |
| 1 | 5 | 56 | 7 | 58 | 12 | 57 | |
| CEA (pretherapeutic) | |||||||
| median [min-max] | 112 [5–36812] | 92 [1–1129] | 102 [1–36812] | 0.52 | |||
| ≤10 ng/ml | 1 | 11 | 4 | 36 | 5 | 25 | |
| >10 ng/ml | 8 | 89 | 7 | 64 | 15 | 75 | 0.32 |
| LDH (pretherapeutic) | |||||||
| median [min-max] | 660 [259–3238] | 534 [276–3992] | 563.5 [259–3992] | 0.71 | |||
| ≤480 U/l | 3 | 43 | 3 | 33 | 6 | 37.5 | |
| >480 U/L | 4 | 57 | 6 | 67 | 10 | 62.5 | 1.00 |
ND = not determinated
Determination of gene signature
Expression profiling was conducted using Affymetrix U133 A and B chips. For statistical analysis we only considered genes called present in at least 50% of the patients from any one group, resulting in a selection of 19 365 genes.
To determine the differentially expressed genes between responders and non-responders we used the SAM method. Based on an FDR of 20%, about 5000 discriminatory genes were selected and ranked according to their statistical significance. For each gene, using a non-parametric procedure, we estimated the total area (AUC) and the partial area (pAUC) under the ROC curve. Estimation of the pAUC was restricted to the region where the specificity was at least 90%. Genes were then ranked according to AUC and pAUC values, and for each indicator we retained the top 40 genes. This process was repeated twenty-one times with a training set of 20 samples (each time, one sample was left out). In order to establish a stable signature, we selected the genes common to the 21 AUC lists (8 genes) and those common to the 21 pAUC lists (11 genes). Finally, as some genes were common to both the final AUC and pAUC lists, we retained a set of 14 discriminatory genes (table 3). Unsupervised hierarchical clustering and principal component analysis were then applied to the 14 selected genes. This resulted, in both analyses, in a clear separation between responder and non-responder patients (figure 1).
Table 3.
The 14-gene signature that predicts response to FOLFIRI
| Probe set ID | Gene symbol | Gene description | GO Molecular function description | pAUC | AUC | Fold change R/NR* |
|---|---|---|---|---|---|---|
| 210731_s_at | LGALS8 | Consensus includes gb:AL136105/DEF=Human DNA sequence from clone RP4-670F13 on chromosome 1q42.2-43. Contains the gene for Po66 carbohydrate binding protein similar to soluble galactoside-binding lectin 8 (galectin 8, LGALS8). | sugar binding/sugar binding | 0.083** | 0.907 | 1.83 |
| 212190_at | SERPINE2 | Consensus includes gb:AL541302/FEA=EST/DB_XREF=gi:12872241/DB_XREF=est:AL541302/CLONE=CS0DE006YI10. | serine-type endopeptidase inhibitor activity/heparin binding | 0.075 | 0.935*** | 2.31 |
| 213001_at | ANGPTL2 | Consensus includes gb:AF007150.1/DEF=Homo sapiens clone 23767 and 23782 mRNA sequences. | receptor binding | 0.092** | 0.972*** | 1.94 |
| 216954_x_at | ATP5O | Consensus includes gb:S77356.1/DEF=Homo sapiens oligomycin sensitivity conferral protein oscp-like protein mRNA, partial cds. | transporter activity/hydrolase activity/hydrogen-transporting ATP synthase activity | 0.075 | 0.944*** | 1.61 |
| 220375_s_at | --- | gb:NM_024752.1/DEF=Homo sapiens hypothetical protein FLJ23312 (FLJ23312), mRNA. | --- | 0.092** | 0.981*** | 2.07 |
| 204398_s_at | EML2 | gb:NM_012155.1/DEF=Homo sapiens microtubule-associated protein like echinoderm EMAP (EMAP-2), mRNA. | 0.083** | 0.88 | 1.49 | |
| 205756_s_at | F8 | gb:NM_000132.2/DEF=Homo sapiens coagulation factor VIII, procoagulant component (hemophilia A) (F8), transcript variant 1, mRNA. | copper ion binding/oxidoreductase activity | 0.083** | 0.917 | 1.82 |
| 208174_x_at | U2AF1L2 | gb:NM_005089.1/DEF=Homo sapiens U2 small nuclear ribonucleoprotein auxiliary factor, small subunit 2 (U2AF1RS2), mRNA. | nucleotide binding/RNA binding | 0.092** | 0.944*** | 1.32 |
| 208486_at | DRD5 | gb:NM_000798.1/DEF=Homo sapiens dopamine receptor D5 (DRD5), mRNA. | rhodopsin-like receptor activity/receptor activity/dopamine receptor activity | 0.083** | 0.889 | 1.33 |
| 208798_x_at | GOLGIN-67 | gb:AF204231.1/DEF=Homo sapiens 88-kDa Golgi protein (GM88) mRNA, complete cds. | --- | 0.083** | 0.926 | 1.67 |
| 209538_at | ZNF32 | gb:U69645.1/DEF=Human zinc finger protein mRNA, complete cds. | nucleic acid binding/DNA binding /zinc ion binding | 0.083** | 0.972*** | 2.09 |
| 209594_x_at | PSG9 | gb:M34421.1/DEF=Human pregnancy-specific beta-1 glycoprotein mRNA, complete cds. | --- | 0.083** | 0.87 | 1.62 |
| 236954_at | BOLL | Consensus includes gb:BF059752/FEA=EST/DB_XREF=gi:10813648/DB_XREF=est:7k65h06.x1/CLONE=IMAGE:3480442/UG=Hs.169797 ESTs. | nucleotide binding/nucleic acid binding/RNA binding | 0.075 | 0.972*** | 70.75 |
| 241602_at | ZNF582 | Consensus includes gb:BG432829/FEA=EST/DB_XREF=gi:13339335/DB_XREF=est:602496037F1/CLONE=IMAGE:4610000/UG=Hs.152174 ESTs. | nucleic acid binding/zinc ion binding | 0.083** | 0.935*** | 161.31 |
R=responder; NR=non-responder;
Genes selected by pAUC;
Genes selected by AUC;
Fig 1.
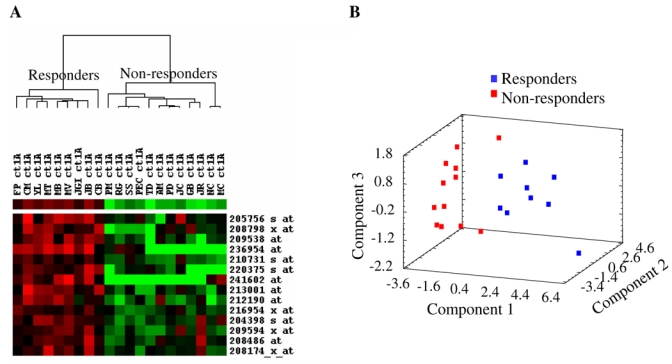
Analysis of gene signature by (A) unsupervised clustering and (B) principal component analysis (PCA). (A): column represents sample, and row represents gene. Red indicates relative high expression and green relative low expression. (B): PCA involves a mathematical procedure that represents the maximum of the data information by reducing the space dimension. Here 80% of the information was explained with the three principal components used in the graph.
Using an SVM-learning algorithm, we defined a predictor classifier and its performance was evaluated by the LOOCV. All the 9 responders (100% specificity) and 11 out of the12 non-responders (92% sensitivity) were correctly classified, for an overall accuracy of 95%. To assess the misclassification rates, we used the approach described by Michiels et al.,32 that consists in dividing the dataset into training sets of different sizes (from 5 to 19 samples). The remaining samples were considered as a validation set (size from 16 to 2 samples). A total of 500 random training sets were associated with each sample size. For a given training set, a classifier was built by SVM using the14 selected genes and tested in a designated validation test. As shown in figure 2, even with the smallest training size, the misclassification rate was only 25.6% (95 CI: 19% – 34%) and from a training set size > 13, the misclassification rate did not exceed 7.5%.
Fig 2.
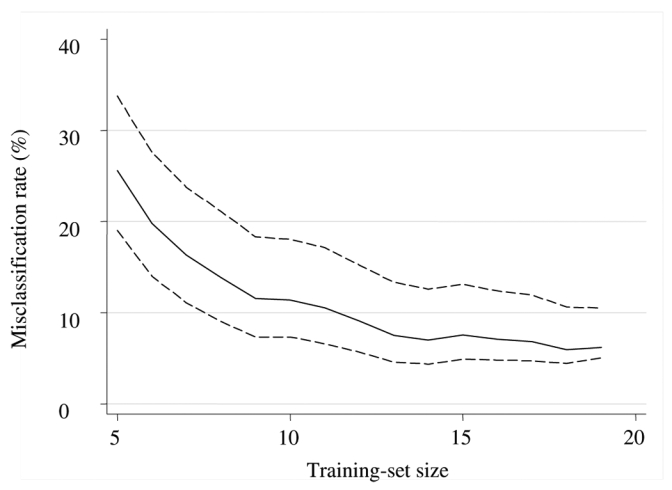
Proportion of misclassification in validation sets as a function of the corresponding training set size. Solid line represents the misclassification rate which is equal to mean proportion obtained from 500 random training-validation sets. Dotted lines represent the 95% confidence intervals.
Functional classification of 14 genes from the signature
All the 14 genes from the signature were over expressed in the responder tumors. These genes showed a wide ratio, with 1.3 to 160-fold increases in expression in sensitive as compared with the resistant tumors. According to the GeneOntology classification, functional classes of these differentially expressed genes included RNA splicing (U2AF1L2), regulation of transcription (ZNF32 and ZNF582), cell adhesion (F8, Galectin-8, PSG9), cell differentiation (SERPINE2, BOLL), ion transport (ATP5O), signal transduction (DRD5) development (ANGPTL2) and visual perception (EML2). GOLGIN-67 is a Golgi membrane protein whose function is unknown.
DISCUSSION
Current treatment strategies for colorectal cancer are far from optimal, due in part to the appearance of drug resistance in about half of the patients. In the metastatic setting, administration of chemotherapy likely to induce a maximal response in the first course of treatment is critical to enhance overall treatment success. This is even more crucial in the case of adjuvant treatment where the rationale is to reduce the rate of tumor recurrence and mortality in patients who have undergone curative surgery (stage II and III). This emphasises the importance of identifying predictive factors of response to treatment. Despite the identification of single markers capable of predicting drug response, their predictive efficacy remains insufficient to allow their use in routine clinical practice.25
The study reported here was designed to identify a pattern of gene expression able to predict response to FOLFIRI in colorectal cancer patients with synchronous and unresectable liver metastases. This combination of irinotecan, fluorouracil, and leucovorin is considered as one of the reference first-line treatments for metastatic colorectal cancer with objective response rates of 49% and 56%.4,33 In our series of 21 patients, the response rate to FOLFIRI was 43% and median overall survival was 21 months, in agreement with the available literature data.
To determine the gene signature for response prediction from transcriptome studies, we first selected the significant differentially expressed genes from the large data set of gene expression. Then we used statistical measures of discrimination. The ROC curve provides a visual description of the trade-off between false-positive and true-positive rates for all possible threshold values. The AUC is the most commonly used index to estimate the global discriminative power of a diagnostic test. It has been suggested that the pAUC34 restricts attention to a region of the marker space associated with a high specificity (probability of detecting the responder patients). The use of both of these indices allowed us to select marker genes presenting a strong global discriminant power associated with high sensitivity and specificity. We finally obtained a 14-gene signature that accurately (95%) predicted the response to FOLFIRI. Moreover, by applying a multiple random training-validation strategy,32 we showed that from a training set of 13 patients the misclassification rate did not exceed 7.5%. This result suggests that our 14-gene signature is stable and was not affected by the small sample size.
In the gene expression profiles associated with clinical outcomes, it is not clear whether these genes are causal or merely markers. The signature does not include genes from pathways commonly known as being involved in resistance mechanisms, as for example drug inactivation, drug efflux, repair DNA damage, or defects in apoptosis.35 However, among the 14 genes, three genes, galectine-8, PSG9 and SERPINE2, could be involved in the adhesion process. Galectin-8 is a matricellular protein that positively or negatively regulates cell adhesion, depending on the extracellular context.36 Moreover, the quantitative determination of the immunohistochemical expression of galectin-8 in the series of colon cancer specimens clearly showed that the extensively invasive colon cancers exhibited significantly less galectin-8 than locally invasive ones.37 PSG9, which is ectopically upregulated in vivo by colon cancer cells, 38 has an RGD motif in a conserved region in the N-terminal domain which suggests that these genes may function as adhesion recognition signals for integrins. The serine proteinase inhibitor SERPINE2 could participate in maintaining the integrity of connective tissue matrices. SERPINE2 has been shown to inhibit tumor cell-mediated extracellular matrix destruction.39 Two other genes, FVIII and ANGPTL2, could reflect tumor vascularization. Indeed, intratumoral angiogenesis is commonly quantified by a microvessel density measurement using immunohistochemical staining with monoclonal antibodies against factor VIII.40 ANGPTL2 protein induces sprouting in vascular endothelial cells and promotes angiogenesis.41 Altogether, these results support the idea that the responders’ tumors seem more adhesive and vascularized than those of the non-responders. As it is known that adhesive interactions play a role in the metastatic process, we cannot exclude that this gene pattern also reflects mechanistic differences in metastasis formation between both groups.
This study provides new insights into the treatment of colorectal cancer. One major application would be to use the signature as a decision tool to assist oncologists in selecting colorectal cancer patients who could benefit from chemotherapy, both in the adjuvant and the first-line metastatic setting. Applying the 14-gene signature, we are able to detect all the responder patients from our cohort. To our knowledge, this is the first predictor classifier based on microarray gene expression in colon cancer. In this cancer, only gene signatures predicting prognosis19, 21, 42, 43 have been determined. The advantage of our prospective monocenter study is that the genomic and clinical data quality was homogeneous. However, as the results are based on a relatively small sample size it is essential to validate and if necessary to improve this 14-gene signature in a larger independent cohort of patients. We are currently undergoing a national multicenter study with 5 times as many patients. Then, a randomised phase III clinical trial could be set up comparing the signature classifier with the usual clinical characteristics in selecting colorectal cancer patients for chemotherapy.
Acknowledgments
We thank Dr. S. L. Salhi for carefully reading the manuscript.
References
- 1.Weitz J, Koch M, Debus J, et al. Colorectal cancer. Lancet. 2005;365:153–65. doi: 10.1016/S0140-6736(05)17706-X. [DOI] [PubMed] [Google Scholar]
- 2.Vanhoefer U, Harstrick A, Achterrath W, et al. Irinotecan in the treatment of colorectal cancer: clinical overview. J Clin Oncol. 2001;19:1501–1518. doi: 10.1200/JCO.2001.19.5.1501. [DOI] [PubMed] [Google Scholar]
- 3.Pelley RJ. Oxaliplatin: a new agent for colorectal cancer. Curr Oncol Rep. 2001;3:147–155. doi: 10.1007/s11912-001-0015-6. [DOI] [PubMed] [Google Scholar]
- 4.Douillard JY, Cunningham D, Roth AD, et al. Irinotecan combined with fluorouracil compared with fluorouracil alone as first-line treatment for metastatic colorectal cancer: a multicentre randomised trial. Lancet. 2000;355:1041–1047. doi: 10.1016/s0140-6736(00)02034-1. [DOI] [PubMed] [Google Scholar]
- 5.Goldberg RM, Sargent DJ, Morton RF, et al. A randomized controlled trial of fluorouracil plus leucovorin, irinotecan, and oxaliplatin combinations in patients with previously untreated metastatic colorectal cancer. J Clin Oncol. 2004;22:23–30. doi: 10.1200/JCO.2004.09.046. [DOI] [PubMed] [Google Scholar]
- 6.Cunningham D, Humblet Y, Siena S, et al. Cetuximab monotherapy and cetuximab plus irinotecan in irinotecan-refractory metastatic colorectal cancer. N Engl J Med. 2004;351:337–345. doi: 10.1056/NEJMoa033025. [DOI] [PubMed] [Google Scholar]
- 7.Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. N Engl J Med. 2004;350:2335–2342. doi: 10.1056/NEJMoa032691. [DOI] [PubMed] [Google Scholar]
- 8.Iacopetta B, Grieu F, Joseph D, et al. A polymorphism in the enhancer region of the thymidylate synthase promoter influences the survival of colorectal cancer patients treated with 5-fluorouracil. Br J Cancer. 2001;85:827–830. doi: 10.1054/bjoc.2001.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salonga D, Danenberg KD, Johnson M, et al. Colorectal tumors responding to 5-fluorouracil have low gene expression levels of dihydropyrimidine dehydrogenase, thymidylate synthase, and thymidine phosphorylase. Clin Cancer Res. 2000;6:1322–1327. [PubMed] [Google Scholar]
- 10.Kornmann M, Schwabe W, Sander S, et al. Thymidylate synthase and dihydropyrimidine dehydrogenase mRNA expression levels: predictors for survival in colorectal cancer patients receiving adjuvant 5-fluorouracil. Clin Cancer Res. 2003;9:4116–4124. [PubMed] [Google Scholar]
- 11.Ribic CM, Sargent DJ, Moore MJ, et al. Tumor microsatellite-instability status as a predictor of benefit from fluorouracil-based adjuvant chemotherapy for colon cancer. N Engl J Med. 2003;349:247–257. doi: 10.1056/NEJMoa022289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Paradiso A, Xu J, Mangia A, et al. Topoisomerase-I, thymidylate synthase primary tumor expression and clinical efficacy of 5-FU/CPT-11 chemotherapy in advanced colorectal cancer patients. Int J Cancer. 2004;111:252–258. doi: 10.1002/ijc.20208. [DOI] [PubMed] [Google Scholar]
- 13.Shirota Y, Stoehlmacher J, Brabender J, et al. ERCC1 and thymidylate synthase mRNA levels predict survival for colorectal cancer patients receiving combination oxaliplatin and fluorouracil chemotherapy. J Clin Oncol. 2001;19:4298–304. doi: 10.1200/JCO.2001.19.23.4298. [DOI] [PubMed] [Google Scholar]
- 14.Adlard JW, Richman SD, Seymour MT, et al. Prediction of the response of colorectal cancer to systemic therapy. Lancet Oncol. 2002;3:75–82. doi: 10.1016/s1470-2045(02)00648-4. [DOI] [PubMed] [Google Scholar]
- 15.Ahmed FE. Molecular markers that predict response to colon cancer therapy. Expert Rev Mol Diagn. 2005;5:353–575. doi: 10.1586/14737159.5.3.353. [DOI] [PubMed] [Google Scholar]
- 16.Mariadason JM, Arango D, Shi Q, et al. Gene expression profiling-based prediction of response of colon carcinoma cells to 5-fluorouracil and camptothecin. Cancer Res. 2003;63:8791–8812. [PubMed] [Google Scholar]
- 17.Bertucci F, Salas S, Eysteries S, et al. Gene expression profiling of colon cancer by DNA microarrays and correlation with histoclinical parameters. Oncogene. 2004;23:1377–1391. doi: 10.1038/sj.onc.1207262. [DOI] [PubMed] [Google Scholar]
- 18.Birkenkamp-Demtroder K, Christensen LL, Olesen SH, et al. Gene expression in colorectal cancer. Cancer Res. 2002;62:4352–4363. [PubMed] [Google Scholar]
- 19.Wang Y, Jatkoe T, Zhang Y, et al. Gene expression profiles and molecular markers to predict recurrence of Dukes’ B colon cancer. J Clin Oncol. 2004;22:1564–1571. doi: 10.1200/JCO.2004.08.186. [DOI] [PubMed] [Google Scholar]
- 20.Notterman DA, Alon U, Sierk AJ, et al. Transcriptional gene expression profiles of colorectal adenoma, adenocarcinoma, and normal tissue examined by oligonucleotide arrays. Cancer Res. 2001;61:3124–3130. [PubMed] [Google Scholar]
- 21.Eschrich S, Yang I, Bloom G, et al. Molecular staging for survival prediction of colorectal cancer patients. J Clin Oncol. 2005;23:3526–3535. doi: 10.1200/JCO.2005.00.695. [DOI] [PubMed] [Google Scholar]
- 22.Chang JC, Wooten EC, Tsimelzon A, et al. Gene expression profiling for the prediction of therapeutic response to docetaxel in patients with breast cancer. Lancet. 2003;362:362–369. doi: 10.1016/S0140-6736(03)14023-8. [DOI] [PubMed] [Google Scholar]
- 23.Iwao-Koizumi K, Matoba R, Ueno N, et al. Prediction of docetaxel response in human breast cancer by gene expression profiling. J Clin Oncol. 2005;23:422–431. doi: 10.1200/JCO.2005.09.078. [DOI] [PubMed] [Google Scholar]
- 24.Jansen MP, Foekens JA, van Staveren IL, et al. Molecular classification of tamoxifen-resistant breast carcinomas by gene expression profiling. J Clin Oncol. 2005;23:732–740. doi: 10.1200/JCO.2005.05.145. [DOI] [PubMed] [Google Scholar]
- 25.Mariadason JM, Arango D, Augenlicht LH. Customizing chemotherapy for colon cancer: the potential of gene expression profiling. Drug Resist Updat. 2004;7:209–218. doi: 10.1016/j.drup.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 26.Ghadimi BM, Grade M, Difilippantonio MJ, et al. Effectiveness of gene expression profiling for response prediction of rectal adenocarcinomas to preoperative chemoradiotherapy. J Clin Oncol. 2005;23:1826–1838. doi: 10.1200/JCO.2005.00.406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Copois V, Bibeau F, Bascoul-Mollevi C, et al. Impact of RNA degradation on gene expression profiles: Assessment of different methods to reliably determine RNA quality. J Biotechnol. 2006 Aug 2; doi: 10.1016/j.jbiotec.2006.07.032. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 28.Miller AB, Hoogstraten B, Staquet M, et al. Reporting results of cancer treatment. Cancer. 1981;47:207–214. doi: 10.1002/1097-0142(19810101)47:1<207::aid-cncr2820470134>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 29.Tusher VG, Tibshirani R, Chu G. Significance analysis of microarrays applied to the ionizing radiation response. Proc Natl Acad Sci U S A. 2001;98:5116–5121. doi: 10.1073/pnas.091062498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dodd LE, Pepe MS. Partial AUC estimation and regression. Biometrics. 2003;59:614–623. doi: 10.1111/1541-0420.00071. [DOI] [PubMed] [Google Scholar]
- 31.Brown MP, Grundy WN, Lin D, et al. Knowledge-based analysis of microarray gene expression data by using support vector machines. Proc Natl Acad Sci U S A. 2000;97:262–267. doi: 10.1073/pnas.97.1.262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Michiels S, Koscielny S, Hill C. Prediction of cancer outcome with microarrays: a multiple random validation strategy. Lancet. 2005;365:488–492. doi: 10.1016/S0140-6736(05)17866-0. [DOI] [PubMed] [Google Scholar]
- 33.Tournigand C, Andre T, Achille E, et al. FOLFIRI followed by FOLFOX6 or the reverse sequence in advanced colorectal cancer: a randomized GERCOR study. J Clin Oncol. 2004;22:229–237. doi: 10.1200/JCO.2004.05.113. [DOI] [PubMed] [Google Scholar]
- 34.Pepe MS, Longton G, Anderson GL, et al. Selecting differentially expressed genes from microarray experiments. Biometrics. 2003;59:133–142. doi: 10.1111/1541-0420.00016. [DOI] [PubMed] [Google Scholar]
- 35.Gatti L, Zunino F. Overview of tumor cell chemoresistance mechanisms. Methods Mol Med. 2005;111:127–148. doi: 10.1385/1-59259-889-7:127. [DOI] [PubMed] [Google Scholar]
- 36.Levy Y, Arbel-Goren R, Hadari YR, et al. Galectin-8 functions as a matricellular modulator of cell adhesion. J Biol Chem. 2001;276:31285–31295. doi: 10.1074/jbc.M100340200. [DOI] [PubMed] [Google Scholar]
- 37.Nagy N, Bronckart Y, Camby I, et al. Galectin-8 expression decreases in cancer compared with normal and dysplastic human colon tissue and acts significantly on human colon cancer cell migration as a suppressor. Gut. 2002;50:392–401. doi: 10.1136/gut.50.3.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Salahshor S, Goncalves J, Chetty R, et al. Differential gene expression profile reveals deregulation of pregnancy specific beta1 glycoprotein 9 early during colorectal carcinogenesis. BMC Cancer. 2005;5:66–80. doi: 10.1186/1471-2407-5-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bergman BL, Scott RW, Bajpai A, et al. Inhibition of tumor-cell-mediated extracellular matrix destruction by a fibroblast proteinase inhibitor, protease nexin I. Proc Natl Acad Sci U S A. 1986;83:996–1000. doi: 10.1073/pnas.83.4.996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Weidner N, Semple JP, Welch WR, et al. Tumor angiogenesis and metastasis--correlation in invasive breast carcinoma. N Engl J Med. 1991;324:1–8. doi: 10.1056/NEJM199101033240101. [DOI] [PubMed] [Google Scholar]
- 41.Oike Y, Yasunaga K, Suda T. Angiopoietin-related/angiopoietin-like proteins regulate angiogenesis. Int J Hematol. 2004;80:21–28. doi: 10.1532/ijh97.04034. [DOI] [PubMed] [Google Scholar]
- 42.Barrier A, Lemoine A, Boelle PY, et al. Colon cancer prognosis prediction by gene expression profiling. Oncogene. 2005;24:6155–6164. doi: 10.1038/sj.onc.1208984. [DOI] [PubMed] [Google Scholar]
- 43.Barrier A, Boelle PY, Roser F, et al. Stage II Colon Cancer Prognosis Prediction by Tumor Gene Expression Profiling. J Clin Oncol. 2006 Sep 11; doi: 10.1200/JCO.2005.05.0229. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


