Minton et al add to a gathering body of evidence that poor clinical practice in the initial management of patients with bloodstream infections contributes to increased morbidity and mortality.1
We recently performed a retrospective study of 35 patients with community acquired pneumonia and septicaemia transferred within 48 hours of admission to a district general intensive care unit over a year. Outcomes were death or discharge from hospital.
Mean age was 59 (range 14-96), 19 were male, and 24 were smokers. Patients over 65 had a 53% mortality compared with 22% in those under 65. Smokers had a 46% mortality compared with 18% in non-smokers.
CURB 65 scores (Confusion, elevated Urea, elevated Respiratory rate, low Blood pressure and age at least 65) were grouped 0/1, 2/3, and 4/5. Mortality was 30% in the 0/1 and 2/3 groups. Patients scoring 4/5 on admission, however, had 80% mortality.
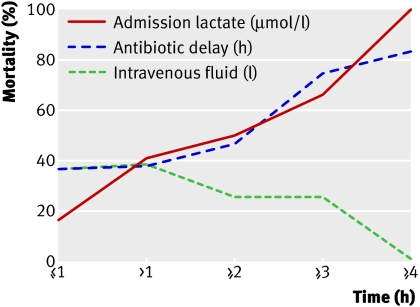
The figure shows the survival benefit of aggressive fluid resuscitation and that mortality increases progressively with increased delay to first antibiotic and increased lactate concentration at admission.
Mortality in patients with pneumonia and sepsis by lactate concentration at admission, antibiotic delay, and fluid resuscitation in first four hours
The findings suggest that timely administration of antibiotics and intravenous fluids is important. Encouraging junior doctors to give patients with suspected sepsis the first dose of antibiotics may help achieve this. We recommended that in acute assessment areas all the equipment and guidelines for sepsis treatment should be contained in a sepsis box.
Patients with admission CURB 65 scores of 4/5 had much higher mortality rates than those with lower scores, and the correlation between admission lactate and mortality suggests that it may be an important assessment factor.
Competing interests: None declared.
References
- 1.Minton J, Clayton J, Sandoe J, McGann H, Wilcox M. Improving early management of bloodstream infection a quality improvement project. BMJ 2008;336:440-3. (23 February.) [DOI] [PMC free article] [PubMed] [Google Scholar]