Abstract
Acute brain insults, such as traumatic brain injury, status epilepticus, or stroke are common etiologies for the development of epilepsy, including temporal lobe epilepsy (TLE), which is often refractory to drug therapy. The mechanisms by which a brain injury can lead to epilepsy are poorly understood. It is well recognized that excessive glutamatergic activity plays a major role in the initial pathological and pathophysiological damage. This initial damage is followed by a latent period, during which there is no seizure activity, yet a number of pathophysiological and structural alterations are taking place in key brain regions, that culminate in the expression of epilepsy. The process by which affected/injured neurons that have survived the acute insult, along with well-preserved neurons are progressively forming hyperexcitable, epileptic neuronal networks has been termed epileptogenesis. Understanding the mechanisms of epileptogenesis is crucial for the development of therapeutic interventions that will prevent the manifestation of epilepsy after a brain injury, or reduce its severity. The amygdala, a temporal lobe structure that is most well known for its central role in emotional behavior, also plays a key role in epileptogenesis and epilepsy. In this article, we review the current knowledge on the pathology of the amygdala associated with epileptogenesis and/or epilepsy in TLE patients, and in animal models of TLE. In addition, because a derangement in the balance between glutamatergic and GABAergic synaptic transmission is a salient feature of hyperexcitable, epileptic neuronal circuits, we also review the information available on the role of the glutamatergic and GABAergic systems in epileptogenesis and epilepsy in the amygdala.
1. Introduction
Epilepsy is one of the most common, chronic neurological disorders, which is characterized by recurrent, spontaneous brain seizures. For some types of epilepsy, the etiology is unknown and may involve genetic predisposition (idiopathic epilepsy; Hirose et al., 2000; Berkovic and Scheffer, 2001), while other types of epilepsy are secondary to another disease, or to an acute brain insult, such as stroke, status epilepticus (SE), head injury, or exposure to neurotoxic substances (acquired epilepsy; Annegers, 1993; Anderson et al., 1999; Herman, 2002). In acquired epilepsy where an acute brain insult has been the etiological factor, the symptoms of epilepsy often appear after a seizure-free period following the acute injury (Angeleri et al., 1999; Gupta and Gupta, 2006; Pagni and Zenga, 2006; Statler et al., 2006). In traumatic brain injury, the incidence of such late post-traumatic seizures ranges from 5% to 18.9% in civilian populations, and 32% to 50% in military personnel (Salazar, 1985; Bushnik et al., 2004). The duration of the latent, seizure-free period can vary widely, from months to years (Treib et al., 1996; Benardo, 2003). This latent period offers the opportunity for therapeutic intervention that may prevent the development of epilepsy, or reduce the severity of the developing disease. The development of regimens that will prevent epilepsy is of vital importance, particularly considering that post-traumatic epilepsy is often refractory to current anticonvulsant therapies (Semah et al., 1998). However, for effective treatments to be developed, the alterations that occur in the structure and function of neuronal networks, which lead to the expression of epilepsy must first be understood. The process whereby, after an acute brain insult, pathological and pathophysiological alterations gradually occur in certain brain regions, leading to the expression of epilepsy, is referred to as epileptogenesis.
Temporal lobe structures, notably the hippocampus, the amygdala, and the piriform cortex are most susceptible to seizurogenic and epileptogenesis-triggering brain insults; accordingly, temporal lobe epilepsy (TLE) is the most common form of epilepsy (Engel, 1989). There is extensive literature on the pathology and pathophysiology of the hippocampus in epilepsy, and information on the hippocampal alterations associated with epileptogenesis is also becoming available (DeLorenzo et al., 2006; El Hassar et al., 2006; Lahtinen et al., 2006; Lukasiuk et al., 2006; McNamara et al., 2006; Raol et al., 2006). The amygdala, on the other hand, has received much less attention, despite the evidence that its role in epilepsy is at least as important as that of the hippocampus. The purpose of the present article is to review the current knowledge on the pathology and pathophysiology of the amygdala in epileptogenesis and epilepsy. Emphasis will be placed on the alterations in the glutamatergic and GABAergic systems, since an imbalance in the function of these two neurotransmitter systems appears to be “the final common pathway” by which molecular/biochemical, structural and pathophysiological changes contribute to hyperexcitability.
2. Is amygdala important in epilepsy?
The amygdala is most well recognized for its central role in emotional behavior, as well as in the modulation of cognitive functions (LeDoux, 1992; Davis, 1994; McGaugh et al., 1996; Fanselow and Gale, 2003; Sah et al., 2003). What is the evidence that the amygdala also plays a central role in epilepsy? In TLE, in addition to hippocampal damage, extensive neuropathology is also present in the amygdala in a significant subpopulation of patients (Cendes et al., 1993b; Saukkonen et al., 1994; Pitkanen et al., 1998). The epileptic focus, in TLE, resides in the amygdala, or the hippocampus, or in both regions ( Quesney, 1986; Isokawa-Akesson et al., 1987; Dewar et al., 1996; Pitkanen et al., 1998; Morimoto et al., 2004). Accordingly, although hippocampal resection of varying degrees is often necessary in drug-refractory TLE, in some cases amygdalectomy alone is sufficient to eliminate seizures (Feindel and Rasmussen, 1991; Jooma et al., 1995; Wieser 2000). Since the amygdala modulates cognitive functions and plays a central role in emotional behavior (LeDoux, 1992; Davis, 1994; McGaugh et al., 1996; Fanselow and Gale, 2003; Sah et al., 2003) and affective disorders (Drevets, 1999; Rauch et al., 2000; Chen et al., 2005), as well as in sexual behavior (Kostarczyk, 1986; Salamon et al., 2005), amygdala dysfunction in TLE is important not only for its role in the generation of seizures, but also for its role in the emotional and cognitive disorders (Kanner, 2006; Swinkels et al., 2006; Briellmann et al., 2007; Richardson et al., 2007; Seethalakshmi and Krishnamoorthy, 2007), and in sexual dysfunction (Herzog et al., 2003; Harden, 2006) that often accompany epilepsy.
Studies in animals have suggested that the amygdala is even more prone to generating seizure activity than the hippocampus (Goddard, 1967; Kairiss et al., 1984; Racine et al., 1988). Thus, kindling develops much faster by repeated electrical stimulation of the amygdala than the hippocampus (Goddard, 1967, 1969; McIntyre and Racine, 1986), and interictal discharges tend to be initiated in the amygdala/piriform cortex regardless of the site of kindling (Kairiss et al., 1984; Racine et al., 1988). Additional evidence for a central role of the amygdala in the generation and spread of seizure activity comes from studies on the mechanisms by which nerve agents induce brain seizures. These studies have demonstrated that, after exposure to toxic levels of the nerve agent soman, the amygdala displays the earliest and most rapid increase in extracellular glutamate, suggesting an early involvement of the amygdala in the development of soman-induced seizures (Lallement et al., 1991). Moreover, after nerve agent exposure, the amygdala displays the most extensive seizure induced-damage (Shih et al., 2003), which is consistent with its exceptionally high susceptibility to seizurogenic insults.
From the more than 10 nuclei that amygdala is composed of (McDonald, 2003; Sah et al., 2003), the basolateral nucleus of the amygdala (BLA) plays the most important role in the initiation and spread of seizures. Activation of the BLA is primarily responsible for the generation of widespread SE, even in animal models where seizures are evoked in extra-amygdalar regions (White and Price, 1993a, 1993b). Furthermore, prolonged electrical stimulation triggers SE more readily when the stimulation is applied to the BLA than to the central and medial amygdala, or to the adjacent piriform cortex (Mohapel et al., 1996).
Thus, both clinical findings and animal studies indicate that the amygdala plays a prominent role in the pathogenesis and the symptomatology of epilepsy. The basolateral region of the amygdala appears to be most susceptible to seizure generation.
3. Amygdala pathology in epilepsy
Amygdala damage is often present in TLE, regardless of the etiology of the disease. It can be present in patients with no prior history of SE (Margerison and Corsellis, 1966; Bruton, 1988; Hudson et al.,1993), or it may develop, with variable timecourses, after SE (Fowler, 1957; Norman, 1964). Although in many cases amygdala damage is co-present with damage in other brain regions and particularly the hippocampus (Bruton, 1988; Guerreiro et al., 1999), it can also be an isolated pathological finding in TLE patients (Hudson et al., 1993; Miller et al. 1994; Guerreiro et al., 1999). Magnetic resonance imaging has revealed that a common pathology of the amygdala in TLE is atrophy (reduced volume associated with neuronal loss), which can range from 10% to 57% volume reduction (Pitkanen et al., 1998). Although amygdala atrophy can be present bilaterally, most often it coincides with the hemisphere that harbors the epileptic focus (Cendes et al., 1993b, 1993c, 1993d; Saukkonen et al., 1994; Van Paesshen et al., 1996). The severity of the atrophy does not appear to correlate with the frequency of seizures, the age of the patient, or the age of onset of epilepsy (Cendes et al., 1993a; Guerreiro et al., 1999; Salmenpera et al., 2001). A correlation of amygdala atrophy with the chronicity of epilepsy has been found in some studies (Kalviainen et al., 1997; Bernasconi et al., 2005), however this is not a consistent finding (Cendes et al., 1993c; Guerreiro et al., 1999; Salmenpera et al., 2001). A more severe amygdala atrophy may be associated with a history of prolonged febrile convulsions (Cendes et al., 1993a; Salmenpera et al., 2001), but this correlation has not been found consistently (Bernasconi et al., 2005). Functional consequences that accompany significant amygdala damage in TLE patients include experience of fear during seizures (Cendes et al., 1994) and prolonged postictal confusion (Guerreiro et al., 1999).
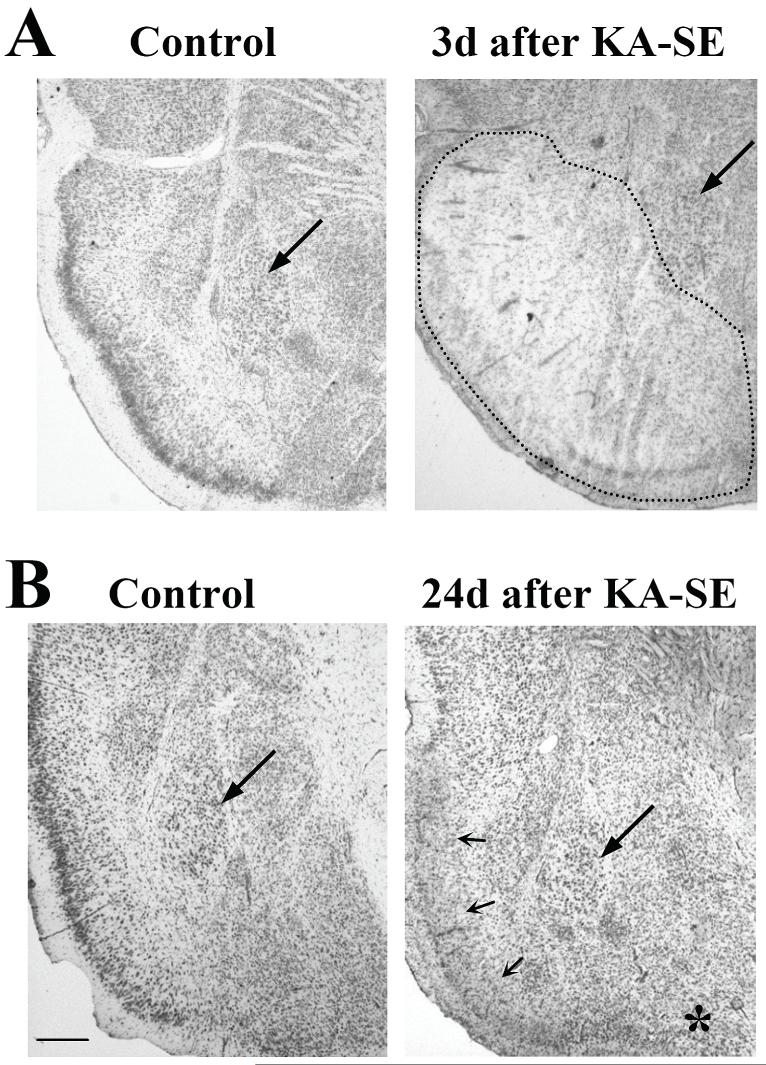
The regions of the amygdala that present the most severe damage (neuronal loss and gliosis), in TLE patients, are the lateral and basal nuclei (Meyer et al., 1955; Margerison and Corsellis, 1966; Hudson et al., 1993; Pitkanen et al., 1998). Similarly, in non-human primates, the basolateral portions of the amygdala are the most susceptible to seizure-induced damage (Meldrum and Brierley, 1973; Wasterlain et al., 1996; Pitkanen et al., 1998). In rat models of SE, the greatest cell loss in the amygdala is also observed in portions of the lateral and basal nuclei, as well as in the deep layers of the anterior cortical and medial nuclei, and the posterior cortical nucleus (Tuunanen et al., 1996). Interestingly, Tuunanen et al. (1997) found that somatostatin-immunoreactive neurons (the majority of which are GABAergic neurons; McDonald and Pearson, 1989; McDonald and Mascagni, 2002) in the medial division of the lateral nucleus and magnocellular division of the basal nucleus, in the rat, are most susceptible to damage even by a relatively small number of kindling-induced seizures, while overall the magnocellular division of the basal nucleus appears well preserved even after SE (Tuunanen, 1996, 1997). Our observations in rats, after kainic acid-induced SE, also show a well-preserved magnocellular division in the basal nucleus, despite extensive damage in other regions of the amygdala, as well as in the piriform cortex (Fig. 1). Thus, it appears that a subpopulation of inhibitory neurons in an important projection nucleus of the amygdala is very susceptible to seizure-induced damage, while projection neurons remain relatively intact. This would facilitate the spread of seizures from the damaged, epileptic amygdala to other brain regions (for a discussion on this implication see Tuunanen, 1996, 1997).
Figure 1.
Photomicrographs of cresyl violet-stained coronal sections (section thickness: (A) 35μm, (B) 16μm) from the rat piriform cortex-amygdala region, at different time points after kainic acid-induced SE (KA-SE), and from control animals. Sections are approximately -2.12mm from bregma (after Paxinos and Watson, 1998). Upper images (A) demonstrate the extensive edema present at 3 days after KA-SE in the piriform cortex and the amygdala (outlined with dotted line). (B) Edema is no longer present at 24 days after KA-SE, while dramatically severe neuronal loss is evident in the piriform cortex (small arrows). The cortical nucleus of the amygdala is also damaged but to a lower extent (*). The magnocellular division of the basal nucleus of the amygdala (large arrows) remains well preserved at both time points after KA-SE. Scale bar: 500 μm.
Importantly, seizure-induced cell loss in the amygdala and other brain areas is accompanied by neurogenesis; this has been observed at 24 hours after the last seizures induced by a GABAA antagonist, injected systemically for 14 consecutive days, in rats (Park et al., 2006). Neurogenesis appears to be an independent effect of recurrent epileptic seizures rather than a consequence of neuronal cell death, as there is no significant correlation between the severity of cell loss and the extent of neurogenesis (Park et al., 2006). Whether the appearance of newborn neurons signifies a potential for reorganization of the amygdala, and whether it would contribute to the pathogenesis of epilepsy, or to a gradual recovery of pathology and function after the initial insult, remains to be determined. In the studies by Tuunanen et al. (1996), there were no significant differences in the distribution or severity of amygdala damage (cell loss) at 2 days or 2 weeks after kainic acid-induced SE, in rats. Thus, at least within this timeframe of SE-induced epileptogenesis, there are no significant changes in the distribution or the extent of neuronal degeneration and regeneration in the amygdala, in this model.
When pathological alterations in the rat amygdala were examined with quantitative MRI, after SE induced by amygdala stimulation, it was found that much of the initial damage was associated with edema, which, for the most part, was reversed by 9 days after SE (Nairismagi et al., 2004). However, secondary neuronal pathology appeared and progressed with time, in the amygdala and other brain regions (Nairismagi et al., 2004). After kainic acid-induced SE, in rats, increased MRI signal intensity, suggesting the presence of edema, was observed bilaterally in the amygdala and the piriform cortex, immediately after the sustained seizures, as well as 24 hours later (Nakasu et al., 1995). This early edema is also observed with histological methods (see Fig. 1A). Reversible increases in MRI signal intensity within the medial temporal lobe, suggestive of edema, is also seen in TLE patients after prolonged seizure activity (Chan et al., 1996). The significance of this largely reversible acute tissue damage, and whether it precedes and is predictive of (further) subsequent pathological and pathophysiological alterations, is unclear. In the kainic acid-induced SE model, the area of hyperintensity in diffusion-weighted MRI images (signifying the presence of edema) was concordant with the histologic distribution of neuronal pyknosis and neuropile vacuolation (Nakasu et al., 1995). However, others have found that this early disruption in water homeostasis does not correlate significantly with the extent of the long-term pathological damage and the severity of the spontaneous, recurrent seizures (Nairismagi et al., 2004). Finally, as is the case with the hippocampus (Andre et al., 2001; Brandt et al., 2003; Francois et al., 2006), it appears that pathological damage (early or late) of the amygdala does not correlate well with the development of epileptogenesis and the severity of epilepsy. Thus, the development of spontaneous seizures after extended amygdala kindling was not accompanied by neurodegeneration in either the amygdala, or the CA1 and CA3 hippocampal areas (Brandt et al., 2004). Similarly, in rats becoming epileptic after SE induced by hippocampal stimulation, there were no significant pathological, neurodegenerative changes in the amygdala, despite the presence of pronounced pathophysiological alterations in the basal amygdala (Mangan et al., 2000).
In summary, amygdala atrophy is often present in TLE patients, but clear correlations of the presence of amygdala pathology with other parameters of the disease that would help us understand the causes and the consequences of amygdala atrophy are still not evident. In both human patients and animal models of epilepsy, certain regions of the amygdala, and in particular the basolateral nucleus are most susceptible to damage. Although pathological damage of the amygdala is prominent in some animal models of epilepsy, pathophysiological alterations that produce or contribute to the generation of spontaneous seizures and the expression of epilepsy can be present without evidence for concomitant presence of pathological damage.
4. The role of the glutamatergic system
It is well understood that excessive glutamatergic activity plays a key role in both the induction of neuronal pathology that can lead to hyperexcitability and epilepsy, and the expression of hyperexcitability and epilepsy. Thus, in experimental models, when status epilepticus (SE) is induced by injections of kainic acid, the initiation of seizures is obviously due to activation of the kainate subtype of glutamate receptors; the resulting neuronal damage is due to excessive glutamate release associated with the epileptic seizures (Liu et al., 1997; Sherwin, 1999; Pena & Tapia, 1999; Ueda et al., 2002). When SE is triggered by administration of the muscarinic agonist pilocarpine, or by acetycholinesterase inhibitors, although excessive cholinergic activity is the initial trigger of epileptic seizures, it is glutamatergic activity that reinforces and sustains seizures, and is ultimately responsible for neuronal damage (Wade et al., 1987; Lallement et al., 1991a, 1991b, 1992; McDonough and Shih, 1997; Smolders et al., 1997). Similarly, in humans, in acquired epilepsy due to an acute brain insult, such as traumatic brain injury, stroke, or status epilepticus, excessive glutamate release plays a central role in the resulting brain damage (Choi, 1988; Choi and Rothman, 1990; During & Spencer, 1993; Arundine and Tymianski, 2004; Yi and Hazell, 2006). Glutamate excitotoxicity is due to overstimulation of glutamate receptors producing excessive neuronal depolarization, which is accompanied by an overwhelming increase in free intracellular calcium, entering via glutamate receptor/channels and voltage gated calcium channels, as well as released from intracellular stores; the calcium-dependent signaling pathways that are subsequently activated lead to neuronal dysfunction (physiopathology), and/or pathology (alterations in morphology/structure), or death (Choi, 1988; Pal et al., 1999, 2000; DeLorenzo et al., 2006; McNamara et al., 2006).
After the initial damage from an acute brain insult, there is a “silent”, latent period before the expression of epilepsy. A number of alterations occur in surviving neurons during this period of epileptogenesis (Kim et al. 2006; Gorter et al., 2006; DeLorenzo et al., 2006; Lahtinen et al., 2006; McNamara et al., 2006; Lukasiuk et al., 2006; El Hassar et al., 2006.) which eventually lead to the generation of spontaneous, recurrent seizures. Glutamatergic activity does not appear to play an important role in the progression of epileptogenesis, since antiepileptic drugs, which suppress excitatory synaptic transmission, either directly or by increasing GABAergic inhibitory activity, fail to inhibit epileptogenesis if administered after the acute injury (Halonen et al. 2001; Loscher, 2002; Francois et al., 2006). However, when epilepsy has developed, the major characteristic of the hyperexcitable neuronal circuits is excessive glutamatergic activity, associated with a derangement in the balance between glutamatergic and GABAergic synaptic transmission (Bernard, 2005; El Hassar et al., 2006).
As in other brain regions, the glutamatergic system in the amygdala also plays a central role in the induction of neuronal damage and epileptogenesis, as well as in the expression of epilepsy. In kainate- or pilocarpine-induced SE animal models, pretreatment with NMDA receptor antagonists prevents the induction of epileptogenesis, despite the lack of a significant effect on the SE itself (Stafstrom et al., 1993 and Rice and DeLorenzo, 1998). However, NMDA receptor antagonists do not inhibit epileptogenesis if administered after the acute brain insult (Brandt et al., 2003), and they are also weak anticonvulsants when epilepsy has developed (McNamara et al., 1988; Sato et al., 1988; Morimoto et al., 2004). Some of the information on the role of the glutamatergic system in epileptogenesis and epilepsy in the amygdala comes from kindling experiments, where repeated electrical stimulation of a seizure-susceptible brain region lowers the threshold for seizures, and eventually triggers generalized, stage 5 seizures; spontaneous seizures also often occur after extended kindling (Brandt et al., 2004). In the kindling model, the process of epileptogenesis is not triggered by an acute brain insult, but rather it is induced and reinforced incrementally by repeated stimulation. Kindling induced by repeated electrical stimulation of the amygdala requires activation of AMPA receptors (Namba et al., 1994; Rogawski et al., 2001). Kindling can also be produced by application of glutamate. Thus, overactivation of glutamate receptors by repeated focal application of glutamate into the amygdala has a kindling-like effect (“glutamate kindling”; Mori and Wada, 1987; Croucher and Bradford, 1989). Antagonists of NMDA receptors retard or prevent amygdala kindling induced either by repeated electrical stimulation (Gilbert, 1988; McNamara et al., 1988; Sato et al., 1988; Holmes et al., 1990; Morimoto et al., 1991), or by glutamate application (Croucher and Bradford, 1990). In agreement with these results, amygdala kindling is more difficult to induce in transgenic mice expressing high neuronal levels of NR2D, which produces lower conductance NMDA receptor complexes with reduced affinity for glutamate (Bengzon et al., 1999). Taken together, these findings are consistent with the view that NMDA receptor/channels provide a major route for calcium influx during induction of epileptogenesis.
The pathophysiological alterations that take place in the amygdala as epileptogenesis is underway are largely unknown, and it is generally assumed that the alterations seen in epilepsy have developed gradually during the course of epileptogenesis. However, do these alterations progress in a more or less linear fashion during the course of epileptogenesis, or does the timing pattern of their development result in different excitability states at different time points during epileptogenesis? Answers to these questions are necessary for the development of successful pharmacological interventions that will inhibit epileptogenesis. It should be noted in this regard, that in the CA1 hippocampal pyramidal cells, the balance between glutamatergic excitation and GABAergic inhibition is actually tilted towards more inhibition at 3 to 5 days after pilocarpine-induced SE in rats, compared to controls. This is reversed, with glutamatergic drive increasing significantly to generate interictal activity by 7 to 10 days after SE (El Hassar et al., 2007). These observations suggest that the dynamics between major neurotransmitter systems can differ dramatically at different stages of epileptogenesis.
When epilepsy has developed, alterations in glutamatergic synaptic transmission are evident in the amygdala. In brain slices from rats becoming epileptic after pilocarpine-induced SE, large amplitude depolarizing postsynaptic potentials (along with reduction of inhibition; see next section) were evoked in lateral amygdala neurons; increased spontaneous field activity was correlated with intracellularly recorded neuronal firing that was blocked by glutamate receptor antagonists (suggesting that it was induced synaptically), while the intrinsic properties of neurons were not significantly altered (Benini and Avoli, 2006). Similarly, basal amygdala neurons from rats becoming epileptic after SE induced by stimulation of the hippocampus, display hyperexcitability characterized by multiple action potential bursts in response to stimulation of the stria terminalis (Mangan et al., 2000). In brain slices from kindled rats, basolateral amygdala neurons display large amplitude AMPA and NMDA receptor-mediated EPSPs, which can be evoked with lower stimulus intensities as compared to control rats (Rainnie et al., 1992; Shoji et al., 1998). Although there are impairments also in GABAergic transmission, enhanced glutamatergic transmission in the BLA of kindled rats is still present when GABAA receptors are blocked (Rainnie et al., 1992), which is indicative of alterations in components that are directly involved in glutamatergic transmission. Recordings of whole-cell currents from basolateral amygdala neurons have shown that the rise time of evoked CNQX- and AP5-sensitive EPSCs, and the decay time constant of evoked CNQX-sensitive EPSCs are shorter in kindled rats, suggesting that excitatory synapses at the proximal dendrites and/or the somata of kindled neurons may contribute more effectively to the generation of evoked EPSCs than those at distal dendrites (Shoji et al., 1998). In addition, the frequency and amplitude of spontaneous EPSCs are increased in basolateral amygdala neurons from kindled rats, in tetrodotoxin-containing medium with either normal or low concentration of calcium, suggesting an increased probability of presynaptic glutamate release (Shoji et al., 1998). The increases in the amplitudes of spontaneous and evoked EPSCs and in the frequency of spontaneous EPSCs may contribute to the epileptiform discharges in kindled amygdala neurons (Shoji et al., 1998). The intrinsic properties of basolateral amygdala neurons (resting membrane potential, apparent input resistance, current-voltage relationship of the membrane, number of action potentials elicited in response to depolarizing current injection, as well as the threshold, amplitude, and duration of action potentials) are not altered by kindling (Rainnie et al., 1992; Shoji et al., 1998).
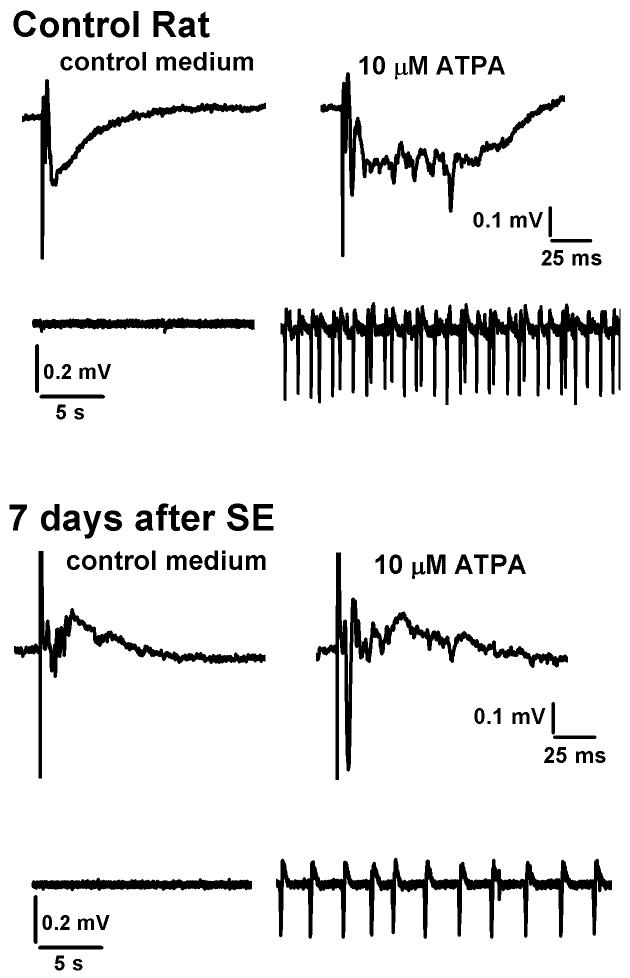
In rats where epilepsy developed after kainic acid-induced SE, evoked field potentials in the BLA contained a much greater number of population spikes compared to control rats, and these alterations were not only due to reduction of inhibition, as the differences from the control rats were also evident in the presence of GABAA receptor antagonists (Smith and Dudek, 1997). We have made similar observations of burst-like, extracellular spiking activity in field potentials recorded from rats displaying spontaneous recurrent seizures, at 7 days after kainic acid-induced SE (Fig. 2). Increased neuronal discharges can also be seen in the field potentials recorded from epileptic rats, at 7-8 weeks after SE induced by stimulation of the lateral amygdala (see fig 2C, baseline, in Niittykoski et al., 2004), although it was noted in that study that the amplitudes and slopes of the field potentials in the lateral and basal amygdala of the epileptic rats were reduced compared to controls (Niittykoski et al., 2004). We, too, have observed that higher stimulus intensities are required to evoke field potentials in the BLA of epileptic rats, after kainic acid-induced SE, at least when recordings are made up to 10 days after SE; the reduction of the field responses appears to relate to the severity of amygdala damage, as revealed by histological techniques (Qashu and Fritsch et al., unpublished data). These findings are not in discord with the larger EPSPs recorded intracellularly from the epileptic, or kindled amygdala. Thus, when recordings are obtained from single neurons, these are the surviving neurons that participate in the generation of epileptic seizures. When neuronal population responses are sampled using extracellular, field potential recordings, the extent of the damage/cell loss is also “sampled”; weaker population responses can be expected when neuronal damage is extensive and not limited to interneurons.
Figure 2.
Field potentials evoked by stimulation of the external capsule in the BLA region of in vitro brain slices. In rats which had undergone status epilepticus (SE) by systemic injection of kainic acid, eliciting field potentials required higher stimulus intensities compared to control rats (this is due at least in part to amygdala damage; see text), and the field potentials in these rats - which are already epileptic by day 7- contained multiple, low-amplitude population spikes. Bath application of the GluR5 agonist ATPA, which excites principal cells in the BLA (Gryder and Rogawski, 2003) and reduces evoked GABAA receptor-mediated inhibition (Braga et al., 2003), produced epileptiform activity in both the control rats and the SE-rats. Epileptiform activity was always stronger in the control rats compared to the SE-rats, probably due to the neuronal damage in the SE-rat. It is noteworthy however that the SE-damaged amygdala can still sustain strong epileptiform activity.
An area that deserves attention -in relation to the pathophysiology of the amygdala in epileptogenesis and epilepsy- is the role of kainate receptors, and, in particular, the kainate receptors that contain the GluR5 subunit (GluR5KRs). In rats, in contrast to the hippocampus which shows only weak expression of the GluR5 gene, the amygdala displays a markedly high expression of this kainate receptor subunit (Bettler et al., 1990; Li et al., 2001; Braga et al., 2003). The location and function of GluR5KRs in the BLA were revealed recently with electrophysiological studies; on principal cells, GluR5KRs participate in glutamatergic excitation (Gryder and Rogawski, 2003), while on GABAergic interneurons they are present both on postsynaptic sites where they participate in the glutamatergic excitation of interneurons, and on presynaptic GABAergic terminals where they inhibit GABA release (Braga et al., 2003, 2004a; Aroniadou-Anderjaska et al., 2007). Interestingly, a presynaptic facilitation of GABA release that has been seen with very low concentrations of a GluR5 agonist (ATPA; Clarke et al., 1997) in 15 to 22 day old rats (Braga et al., 2003), is no longer present in young adult and adult rats, where only inhibition of GABA release is observed (Aroniadou-Anderjaska et al., unpublished data). The net effect of GluR5KR activation in the rat BLA, in vitro, as we have seen in field potential and current-clamp whole cell recordings, is an overall increase in the BLA neuronal and circuitry excitability, with induction of spontaneous epileptiform bursting. Furthermore, when ATPA is administered to rats in vivo by intravenous infusion, or by direct application into the amygdala, it induces clonic seizures and has an epileptogenic effect (Rogawski et al., 2003; Kaminski et al., 2004). These effects of ATPA are blocked by GluR5KR antagonists. Moreover, GluR5KR antagonists do not block only seizures induced by selective activation of GluR5KRs; Smolders et al., (2002) have demonstrated that GluR5KR antagonists prevent the initiation (induction) and block the expression of limbic seizures induced by electrical stimulation, or by administration of the muscarinic cholinergic receptor agonist pilocarpine. It is important therefore to delineate the role that GluR5KRs play in the initiation and progression of epileptogenesis, and in the expression of limbic epilepsy. The importance of GluR5KRs increases further when it is considered that GluR5 antagonists are unlikely to have significant side effects (see clinical study by Sang et al., 2004) because 1) at concentrations that prevent the induction and block the expression of epileptic seizures, the GluR5 antagonists have no effect on normal excitatory synaptic transmission (Smolders et al., 2002), and 2) the distribution of GluR5KRs in the brain is relatively limited (Bettler et al., 1990; Li et al., 2001; Braga et al., 2003), and, therefore, their blockade should not significantly affect brain function.
5. The role of the GABAergic system
In hyperexcitable, epileptic neuronal circuits, regardless of the underlying mechanisms that have led to hyperexcitability, the characteristic end result is a derangement in the balance between excitatory and inhibitory activity. This imbalance could be associated with molecular and/or functional alterations in components that are directly involved in glutamatergic transmission, or glutamatergic activity could be indirectly enhanced due to impairment in the GABAergic system, or both. In the previous section we examined the role of the glutamatergic system in the induction of epileptogenesis, and reviewed the evidence indicating alterations in glutamatergic transmission in the epileptic amygdala. In this section, we will examine the role of the GABAergic system in epileptogenesis, and the evidence suggesting impairment in the function of the GABAergic system in the amygdala when epilepsy has developed.
It is well established that the GABAergic system controls neural activity and can suppress epileptic activity. For example, in animals kindled by amygdala stimulation, GABAA agonists have potent anticonvulsant effects ( Joy et al., 1984; Loscher and Schwark, 1985; Shin et al., 1986). However, little is known about the role of the GABAergic system in epileptogenesis. Reduction or blockade of inhibitory transmission produces epileptiform discharges, and, if repeated, it can induce epileptogenesis. Thus, repeated intra-amygdala applications of the GABAA receptor antagonist picrotoxin (Cain, 1987) or bicuculline ( Uemura and Kimura, 1988) produces a kindling-like effect. On the other hand, enhancing GABAergic inhibition can prevent or retard epileptogenesis. Thus, in SE animal models, pretreatment with GABA agonists can prevent the development of SE and the ensuing brain damage and epileptogenesis (Inoue et al., 1992; Morimoto et al., 2004). In addition, GABAA agonists retard kindling induced by electrical stimulation of the amygdala (Joy et al., 1984; Shin et al., 1986; Schwark and Haluska, 1987). These studies suggest that the GABAergic system can control the induction of epileptogenesis.
After epileptogenesis has been induced, does impaired GABAergic inhibition play a role in the progression of epileptogenesis? In humans, certain idiopathic epilepsies are associated with mutations affecting GABAA receptors (Lerche et al., 2005), which would suggest a causative or contributing role of impaired inhibition in the development of epilepsy. In addition, it is well-established, at least in animal models, that GABAergic neurons can suffer severe damage after an acute brain insult that triggers epileptogenesis (see next paragraph; Tuunanen et al., 1996; Pitkanen et al., 1998). Does the damage of GABAergic neurons play a major role in the progress of epileptogenesis? When GABA agonists are administered after the acute insult they do not prevent epileptogenesis (Andre et al., 2001; Halonen et al., 2001; see also reviews by Loscher, 2002 and Morimoto et al., 2004). For example, following SE induced by amygdala stimulation, subcutaneous administration of vigabatrin via osmotic minipumps -to produce a chronic elevation of brain GABA levels-for 10 weeks did not prevent the development of spontaneous seizures or pathology (Halonen et al., 2001). This suggests that the development of spontaneous seizures does not require a gradually failing inhibition. However, alterations in inhibition do occur during epileptogenesis as suggested by the pathophysiology of neuronal circuits when epilepsy has developed. GABAergic synaptic transmission is impaired in epilepsy, although the nature and the extent of the impairment differ depending on brain region, methods used to induce epilepsy in animal models, and time elapsed from the point of time the initial insult occurred (Treiman, 2001; Morimoto et al., 2004).
In the lateral amygdala of TLE patients, Yilmazer-Hanke et al. (2006) have reported a reduction in the number of axosomatic inhibitory synaptic profiles at the somata of GAD-negative projection neurons, and the magnitude of the reduction correlated with the extent of perisomatic fibrillary gliosis. In animal models, amygdala-kindled rats, at 2-6 months after experiencing three to five generalized seizures (in addition to the seizures that occurred during the induction of kindling) had a 37-64% loss of GABA-immunoreactive neurons in the basolateral amygdala (Callahan et al., 1991). Others have found that the amygdala interneurons that are most susceptible to damage by seizure activity are the somatostatin-immunoreactive neurons in the medial division of the lateral nucleus and the magnocellular division of the basal nucleus of the amygdala (Tuunanen et al., 1996; Pitkanen et al., 1998). Almost all somatostatin-containing axon terminals in the BLA form symmetrical synapses, the vast majority of which target distal dendrites of pyramidal cells (Muller et al., 2007); this suggests that the loss of somatostatin-containing neurons may have a significant impact on the excitability of the BLA circuitry. When epileptogenesis is triggered by kainic acid-induced SE, there is a 44% loss of GABAergic neurons in the lateral nucleus, and 75% loss in the basal nucleus, at two weeks after SE (Tuunanen et al., 1996).
Some information is also available on the functional impact of the damage and/or loss of GABAergic neurons on GABAergic synaptic inhibition in the epileptic amygdala. Thus, in BLA neurons from amygdala-kindled rats, IPSPs elicited by direct electrical stimulation of interneurons are not altered (Rainnie et al., 1992; Shoji et al., 1998). However, there is a significant reduction in feedforward GABAergic synaptic inhibition and in spontaneous IPSPs (Rainnie et al., 1992), suggesting interneuronal loss and/or impairment in the excitation of interneurons. In lateral amygdala neurons of rats becoming epileptic after pilocarpine-induced SE, the peak conductance of both fast (GABAA receptor-mediated) and late (GABAB receptor-mediated) components of the IPSPs is reduced, the reversal potential of GABAA receptor-mediated IPSPs is more depolarized (increasing the likelihood that GABAA receptor-mediated synaptic transmission will have a depolarizing postsynaptic effect), the frequency of spontaneous IPSPs is reduced, and the efficacy of presynaptic GABAB receptors in inhibiting GABA release during repetitive activation of GABAergic synapses also appears reduced (Benini and Avoli, 2006). In the basolateral amygdala of rats becoming epileptic after kainic acid-induced SE, enhanced excitability and responsiveness is in part attributable to impaired inhibition (Smith and Dudek, 1997). In the basal amygdala from epileptic rats, after SE induced by hippocampal stimulation, fast inhibitory potentials had a more rapid onset and shorter duration than control or kindled rats, while no spontaneous inhibitory potentials were observed in neurons from either epileptic or kindled rats (Mangan et al., 2000). It appears therefore that in addition to interneuronal loss, which can be present in both the kindling and the SE animal models but is more extensive in the latter, presynaptic and postsynaptic alterations in GABAergic synaptic transmission have been found in the SE models.
6. Summary and Concluding Remarks
Pathology
It is clearly evident from the existing literature that the amygdala plays a central role in the pathogenesis and symptomatology of TLE. The relative importance of the amygdala in the pathogenesis of TLE differs among TLE patients, which, to a significant extent, is probably due to the varying etiologies of TLE. When amygdala pathology is part of the diagnostic profile, the nature of the pathology is atrophy, associated with neuronal loss and gliosis. Consistent among species (humans included) is that the pathological alterations occur for the most part within the lateral and basal amygdala nuclei, which are also the nuclei that are most prone to seizure generation, and provide the output pathways that spread seizure activity from the amygdala to other brain regions. Studies in animal models where epilepsy is induced by an acute brain insult have suggested that the pattern of neuronal loss (regions that suffer the most damage and types of neurons that are most sensitive) in the lateral and basal nuclei is such that seizure activity from the atrophied, epileptic amygdala can still easily spread to other brain regions. To what extent the severity and the nature of the initial amygdala pathology, after an acute brain insult, determines whether or not epileptogenesis will be induced is not yet clear. It is also unclear to what extent the severity of the overall amygdala pathology correlates with the severity of epilepsy. It should be considered, however, that regardless of the degree of correlation and the cause-effect relationship between pathology and epileptic seizures, the presence of amygdala pathology in TLE is also important as it relates to the emotional and, in part, the cognitive impairments associated with epilepsy.
Induction of epileptogenesis
Excessive activation of glutamate receptors appears to be the mechanism by which epileptogenesis is induced in the amygdala, regardless of whether enhanced glutamatergic activity is produced directly (e.g. electrical stimulation in kindling or kainic acid in SE) or indirectly (e.g. repeated disinhibition, pilocarpine). Which of the glutamate receptor subtypes are necessary to be activated, which are sufficient, and which are both necessary and sufficient for epileptogenesis to be induced is not yet clear. Their relative contribution to the induction of epileptogenesis may differ in different types of brain insults and different experimental models. However, the evidence so far suggests that NMDA receptors play a pivotal role in triggering epileptogenesis in the amygdala, as in other brain regions.
The process of epileptogenesis
The cellular alterations that take place in the amygdala during the process of epileptogenesis are largely unknown. Despite the fact that enhanced glutamatergic activity and impaired GABAergic inhibition characterize the epileptic amygdala, a gradually failing inhibitory transmission or a progressively enhanced glutamatergic transmission do not appear to be necessary for epileptogenesis to proceed. It is also notable that the severity of the early pathological damage associated with edema in the amygdala, after an acute brain insult, is not a good predictor of the outcome of epileptogenesis, that is, the extent of long-term pathological alterations and the severity of spontaneous, recurrent seizures. In attempting to unravel the mechanisms of epileptogenesis, it should be considered that as there are differences in the manifestation of epilepsy among patients and experimental animal models, there may also be differences in epileptogenesis, not only in time-course, but also in the nature of the alterations and/or their relative contribution to the development of epilepsy. Such differences may depend on brain region, as well as on other factors, most importantly the type of insult that triggers (initiates) epileptogenesis.
The GABAergic system in the epileptic amygdala
When epilepsy has developed in the amygdala, impaired GABAergic inhibition appears to be primarily due to interneuronal loss. However, in SE animal models there are also presynaptic and postsynaptic changes in GABAergic synaptic transmission between surviving neurons; the mechanisms producing and sustaining the alterations in GABAergic transmission need to be elucidated. There is also evidence suggesting that different types of GABAergic interneurons in the amygdala may have different susceptibilities to seizure-induced damage, as somatostatin-containing neurons appear to be most sensitive. What makes certain types of interneurons more vulnerable to seizures, and what the implications of such differential sensitivities are on the excitability of the amygdala circuitry remain to be determined. It is known that GABAergic neurons in the amygdala contain calcium-binding proteins (McDonald and Mascagni, 2001), and somatostatin-containing neurons exhibit calbindin- but no parvalbumin or calretinin immunoreactivity (McDonald and Mascagni, 2002). However, although it is believed that these proteins play a significant role in calcium buffering, their relative contribution to calcium homeostasis during epileptic seizures is unclear, and therefore inferences regarding cell vulnerability to seizures depending on the type of calcium-binding proteins present in the cell cannot be made at present. Whether excitation of surviving GABAergic neurons is also altered and how these alterations compare to those of the excitation of glutamatergic neurons, or how GABAA receptors are regulated in the epileptic amygdala are some more of the questions that have been examined in other brain regions (see for example Gavrilovici et al., 2006 and Qi et al., 2006) but are presently unanswered in the amygdala.
The glutamatergic system in the epileptic amygdala
Glutamatergic transmission is also altered in the epileptic amygdala, and this is not only a consequence of impaired inhibition. Increases in spontaneous glutamatergic activity and evoked AMPA and NMDA receptor-mediated synaptic responses have been observed, as well as enhanced, bursting firing in response to stimulation of afferent inputs, without significant changes in the intrinsic neuronal properties. More research is needed to delineate the mechanisms of the enhancement in glutamatergic synaptic transmission; at present, presynaptic alterations appear to be primarily involved (Shoji et al., 1998). Because the amygdala is one of the few brain structures that are rich in GluR5-containing kainate receptors, and because these receptors have been shown to play a central role in both the induction and expression of limbic seizures, the role of these receptors in epileptogenesis and epilepsy in the amygdala should be investigated.
Other mechanisms
This review has focused primarily on the literature pertaining alterations in glutamatergic and GABAergic transmission in the amygdala, associated with epileptogenesis and epilepsy. However, other alterations in the epileptic amygdala, such as those involving ion channels or neurotrophic factors, can also contribute significantly to hyperexcitability, or may counteract hyperexcitability. For example, the KCNQ2 subunit of potassium channels is upregulated in the basolateral amygdala in amygdala-kindled rats and in spontaneously epileptic rats after SE induced by hippocampal electrical stimulation (Penschuck et al., 2005); since potassium channels containing the KCNQ2 subunit serve to stabilize membrane potential, the upregulation of the KCNQ2 subunit could be an important compensatory mechanism to counteract hyperexcitability (Penschuck et al., 2005). In addition, the brain-derived neurotrophic factor (BDNF) can have both epileptogenic and antiepileptic effects (Koyama and Ikegaya, 2005), and the antiepileptic effects appear to be mediated via neuropeptide Y (Reibel et al., 2000, 2003; Koyama and Ikegaya, 2005). The amygdala, and the BLA in particular, is rich in neuropeptide Y and its receptors (Stanić et al., 2006; Oberto et al., 2007), which are upregulated by seizure activity (Lurton and Cavalheiro, 1997; Vezzani and Sperk, 2004). It is therefore important to determine the role of such ion channels and neuropeptides in the excitability of the amygdala, and exploit it for the prevention of epileptogenesis and the treatment of epilepsy. Finally, it should be noted that pathological and functional alterations in glia cells in the amygdala, and their impact on epileptogenesis and epilepsy is still a largely unexplored territory.
The recent development of two strains of rats with different susceptibilities to kindling and particularly to amygdala kindling (Racine et al., 1999, McIntyre et al., 1999) can provide invaluable insights into the mechanisms underlying predisposition to epilepsy, particularly in relation to these mechanisms in the amygdala. A number of differences have already been found between the kindling-prone and kindling-resistant rats, which include differences in their susceptibility to induction of SE by kainic acid and the nature of the resulting pathology (Xu et al., 2004; Gilby et al., 2005), the amino acid and monoamine neurotransmitter release in the amygdala during intense amygdala stimulation (Shin et al., 2004), GABAergic function in limbic structures (McIntyre et a., 2002), as well as noradrenergic function (Gilby et al., 2005; Shin and McIntyre, 2007). In regard to the noradrenergic function, it is particularly interesting that after kainic acid-induced SE, the kindling-prone rats showed a reduction in alpha1 adrenoceptor mRNA in the hippocampus and the amygdala, whereas an increase was observed in the slow-kindling rats (Gilby et al., 2005). Alpha1 adrenoceptors are involved in anxiety disorders and depression (Brunello et al., 2003; Taylor et al., 2006), the role of the alpha1A adrenoceptor subtype in the BLA is facilitation of GABAergic transmission (Braga et al., 2004b), and the function of alpha 1A adrenoceptors in the BLA is significantly impaired by stress (Braga et al., 2004b; Aroniadou-Anderjaska et al., 2007), which is, at least in part, due to reduction in alpha1A mRNA (Braga et al., unpublished). These findings point to the commonalities between epilepsy and certain emotional disorders in regard to the derangements in the regulation of neuronal excitability in the amygdala, and suggest that unraveling the mechanisms regulating neuronal excitability in the amygdala will facilitate progress in the prevention and treatment of both epilepsy and a host of affective disorders.
Acknowledgements
We thank Drs. Sean Manion and Dmitriy Fayuk for stimulating discussions. This work was supported by the Uniformed Services University of the Health Sciences Grant H070SG and by the National Institutes of Health CounterACT Program through the National Institute of Neurological Disorders and Stroke (award # U01 NS058162-01). Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the federal government. This work was also supported by the Defense Threat Reduction Agency grant # 1.E0021_07_US_C.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anderson V, Hauser W, Rich S. Genetic heterogeneity and epidemiology of the epilepsies. In: Delgado-Escueta A, Porter R, editors. Jasper’s Basic Mechanisms of the Epilepsies. Lippincott Williams and Wilkins; Philadelphia: 1999. pp. 59–73. [Google Scholar]
- Andre V, Ferrandon A, Marescaux C, Nehlig A. Vigabatrin protects against hippocampal damage but is not antiepileptogenic in the lithium-pilocarpine model of temporal lobe epilepsy. Epilepsy Res. 2001;47:99–117. doi: 10.1016/s0920-1211(01)00299-6. [DOI] [PubMed] [Google Scholar]
- Angeleri F, Majkowski J, Cacchio G, Sobieszek A, D’Acunto S, Gesuita R, Bachleda A, Polonara G, Krolicki L, Signorino M, Salvolini U. Posttraumatic epilepsy risk factors: one-year prospective study after head injury. Epilepsia. 1999;40:1222–1230. doi: 10.1111/j.1528-1157.1999.tb00850.x. [DOI] [PubMed] [Google Scholar]
- Annegers J. The epidemiology of epilepsy. In: Wyllie E, editor. The Treatment of Epilepsy. Lea & Febiger; Philadelphia: 1993. pp. 157–164. [Google Scholar]
- Aroniadou-Anderjaska V, Qashu F, Braga MFM. Mechanisms Regulating GABAergic Inhibitory Transmission in the Basolateral Amygdala: Implications for Epilepsy and Anxiety Disorders. Amino Acids. 2007;32:305–315. doi: 10.1007/s00726-006-0415-x. [DOI] [PubMed] [Google Scholar]
- Arundine M, Tymianski M. Molecular mechanisms of glutamate-dependent neurodegeneration in ischemia and traumatic brain injury. Cell Mol. Life Sci. 2004;61:657–668. doi: 10.1007/s00018-003-3319-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Benardo LS. Prevention of epilepsy after head trauma: do we need new drugs or a new approach? Epilepsia. 2003;44:27–33. doi: 10.1046/j.1528-1157.44.s10.2.x. [DOI] [PubMed] [Google Scholar]
- Bengzon J, Okabe S, Lindvall O, McKay RD. Suppression of epileptogenesis by modification of N-methyl-D-aspartate receptor subunit composition. Eur. J. Neurosci. 1999;11:916–922. doi: 10.1046/j.1460-9568.1999.00500.x. [DOI] [PubMed] [Google Scholar]
- Benini R, Avoli M. Altered inhibition in lateral amygdala networks in a rat model of temporal lobe epilepsy. J. Neurophysiol. 2006;95:2143–2154. doi: 10.1152/jn.01217.2005. [DOI] [PubMed] [Google Scholar]
- Berkovic SF, Scheffer IE. Genetics of the epilepsies. Epilepsia. 2001;42:16–23. doi: 10.1046/j.1528-1157.2001.0420s5016.x. [DOI] [PubMed] [Google Scholar]
- Bernard C. Dogma and dreams: experimental lessons for epilepsy mechanism chasers. Cell Mol. Life Sci. 2005;62:1177–1181. doi: 10.1007/s00018-005-5009-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernasconi N, Natsume J, Bernasconi A. Progression in temporal lobe epilepsy: differential atrophy in mesial temporal structures. Neurology. 2005;65:223–228. doi: 10.1212/01.wnl.0000169066.46912.fa. [DOI] [PubMed] [Google Scholar]
- Bettler B, Boulter J, Hermans-Borgmeyer I, O’Shea-Greenfield A, Deneris ES, Moll C, Borgmeyer U, Hollmann M, Heinemann S. Cloning of a novel glutamate receptor subunit, GluR5: expression in the nervous system during development. Neuron. 1990;5:583–595. doi: 10.1016/0896-6273(90)90213-y. [DOI] [PubMed] [Google Scholar]
- Braga MF, Aroniadou-Anderjaska V, Xie J, Li H. Bidirectional modulation of GABA release by presynaptic GluR5 kainate receptors in the basolateral amygdala. J. Neurosci. 2003;23:442–452. doi: 10.1523/JNEUROSCI.23-02-00442.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braga MF, Aroniadou-Anderjaska V, Li H. The physiological role of kainate receptors in the amygdala. Mol. Neurobiol. 2004a;30:127–141. doi: 10.1385/MN:30:2:127. [DOI] [PubMed] [Google Scholar]
- Braga MFM, Aroniadou-Anderjaska V, Manion ST, Hough CJ, Li H. Stress impairs alpha1A adrenoceptor-mediated noradrenergic facilitation of GABAergic transmission in the basolateral amygdala. Neuropsychopharmacology. 2004b;29:45–58. doi: 10.1038/sj.npp.1300297. [DOI] [PubMed] [Google Scholar]
- Brandt C, Potschka H, Loscher W, Ebert U. N-methyl-D-aspartate receptor blockade after status epilepticus protects against limbic brain damage but not against epilepsy in the kainate model of temporal lobe epilepsy. Neuroscience. 2003;118:727–740. doi: 10.1016/s0306-4522(03)00027-7. [DOI] [PubMed] [Google Scholar]
- Brandt C, Ebert U, Loscher W. Epilepsy induced by extended amygdala-kindling in rats: lack of clear association between development of spontaneous seizures and neuronal damage. Epilepsy Res. 2004;62:135–156. doi: 10.1016/j.eplepsyres.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Briellmann RS, Hopwood MJ, Jackson GD. Major depression in temporal lobe epilepsy with hippocampal sclerosis: clinical and imaging correlates. J. Neurol. Neurosurg. Psychiatry. 2007 doi: 10.1136/jnnp.2006.104521. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brunello N, Blier P, Judd LL, Mendlewicz J, Nelson CJ, Souery D, Zohar J, Racagni G. Noradrenaline in mood and anxiety disorders: basic and clinical studies. Int. Clin. Psychopharmacol. 2003;18:191–202. doi: 10.1097/00004850-200307000-00001. [DOI] [PubMed] [Google Scholar]
- Bruton C. The Neuropathology of Temporal Lobe Epilepsy. Oxford University Press; Oxford: 1988. [Google Scholar]
- Bushnik T, Englander J, Duong T. Medical and social issues related to posttraumatic seizures in persons with traumatic brain injury. J. Head Trauma Rehabil. 2004;19:296–304. doi: 10.1097/00001199-200407000-00004. [DOI] [PubMed] [Google Scholar]
- Cain DP. Kindling by repeated intraperitoneal or intracerebral injection of picrotoxin transfers to electrical kindling. Exp. Neurol. 1987;97:243–254. doi: 10.1016/0014-4886(87)90086-0. [DOI] [PubMed] [Google Scholar]
- Callahan PM, Paris JM, Cunningham KA, Shinnick-Gallagher P. Decrease of GABA-immunoreactive neurons in the amygdala after electrical kindling in the rat. Brain Res. 1991;555:335–339. doi: 10.1016/0006-8993(91)90361-x. [DOI] [PubMed] [Google Scholar]
- Cendes F, Andermann F, Dubeau F, Gloor P, Evans A, Jones-Gotman M, Olivier A, Andermann E, Robitaille Y, Lopes-Cendes I. Early childhood prolonged febrile convulsions, atrophy and sclerosis of mesial structures, and temporal lobe epilepsy: an MRI volumetric study. Neurology. 1993a;43:1083–1087. doi: 10.1212/wnl.43.6.1083. [DOI] [PubMed] [Google Scholar]
- Cendes F, Andermann F, Gloor P, Evans A, Jones-Gotman M, Watson C, Melanson D, Olivier A, Peters T, Lopes-Cendes I. MRI volumetric measurement of amygdala and hippocampus in temporal lobe epilepsy. Neurology. 1993b;43:719–725. doi: 10.1212/wnl.43.4.719. [DOI] [PubMed] [Google Scholar]
- Cendes F, Andermann F, Gloor P, Lopes-Cendes I, Andermann E, Melanson D, Jones-Gotman M, Robitaille Y, Evans A, Peters T. Atrophy of mesial structures in patients with temporal lobe epilepsy: cause or consequence of repeated seizures? Ann. Neurol. 1993c;34:795–801. doi: 10.1002/ana.410340607. [DOI] [PubMed] [Google Scholar]
- Cendes F, Leproux F, Melanson D, Ethier R, Evans A, Peters T, Andermann F. MRI of amygdala and hippocampus in temporal lobe epilepsy. J. Comput. Assist. Tomogr. 1993d;17:206–210. doi: 10.1097/00004728-199303000-00008. [DOI] [PubMed] [Google Scholar]
- Cendes F, Andermann F, Gloor P, Gambardella A, Lopes-Cendes I, Watson C, Evans A, Carpenter S, Olivier A. Relationship between atrophy of the amygdala and ictal fear in temporal lobe epilepsy. Brain. 1994;117:739–746. doi: 10.1093/brain/117.4.739. [DOI] [PubMed] [Google Scholar]
- Chan S, Chin SS, Kartha K, Nordli DR, Goodman RR, Pedley TA, Hilal SK. Reversible signal abnormalities in the hippocampus and neocortex after prolonged seizures. AJNR Am. J. Neuroradiol. 1996;17:1725–1731. [PMC free article] [PubMed] [Google Scholar]
- Chen CH, Lennox B, Jacob R, Calder A, Lupson V, Bisbrown-Chippendale R, Suckling J, Bullmore E. Explicit and implicit facial affect recognition in manic and depressed States of bipolar disorder: a functional magnetic resonance imaging study. Biol. Psychiatry. 2006;59:31–39. doi: 10.1016/j.biopsych.2005.06.008. [DOI] [PubMed] [Google Scholar]
- Choi DW. Glutamate neurotoxicity and diseases of the nervous system. Neuron. 1988;1:623–634. doi: 10.1016/0896-6273(88)90162-6. [DOI] [PubMed] [Google Scholar]
- Choi DW, Rothman SM. The role of glutamate neurotoxicity in hypoxic-ischemic neuronal death. Annu Rev. Neurosci. 1990;13:171–182. doi: 10.1146/annurev.ne.13.030190.001131. [DOI] [PubMed] [Google Scholar]
- Clarke VR, Ballyk BA, Hoo KH, Mandelzys A, Pellizzari A, Bath CP, Thomas J, Sharpe EF, Davies CH, Ornstein PL, Schoepp DD, Kamboj RK, Collingridge GL, Lodge D, Bleakman D. A hippocampal GluR5 kainate receptor regulating inhibitory synaptic transmission. Nature. 1997;389:599–603. doi: 10.1038/39315. [DOI] [PubMed] [Google Scholar]
- Croucher MJ, Bradford HF. Kindling of full limbic seizures by repeated microinjections of excitatory amino acids into the rat amygdala. Brain Res. 1989;501:58–65. doi: 10.1016/0006-8993(89)91026-3. [DOI] [PubMed] [Google Scholar]
- Croucher MJ, Bradford HF. NMDA receptor blockade inhibits glutamate-induced kindling of the rat amygdala. Brain Res. 1990;506:349–352. doi: 10.1016/0006-8993(90)91279-p. [DOI] [PubMed] [Google Scholar]
- Davis M. The role of the amygdala in emotional learning. Int. Rev. Neurobiol. 1994;36:225–266. doi: 10.1016/s0074-7742(08)60305-0. [DOI] [PubMed] [Google Scholar]
- DeLorenzo RJ, Sun DA, Deshpande LS. Cellular mechanisms underlying acquired epilepsy: the calcium hypothesis of the induction and maintenance of epilepsy. Pharmacol Ther. 2006;111:288–325. doi: 10.1016/j.pharmthera.2004.10.015. Erratum to. [Pharmacol. Ther. 105(3) (2005) 229-266] [DOI] [PubMed] [Google Scholar]
- Dewar S, Passaro E, Fried I, Engel J., Jr. Intracranial electrode monitoring for seizure localization: indications, methods and the prevention of complications. J. Neurosci. Nurs. 1996;28:280–289. doi: 10.1097/01376517-199610000-00002. [DOI] [PubMed] [Google Scholar]
- Drevets WC. Prefrontal cortical-amygdalar metabolism in major depression. Ann N. Y. Acad. Sci. 1999;877:614–637. doi: 10.1111/j.1749-6632.1999.tb09292.x. [DOI] [PubMed] [Google Scholar]
- During MJ, Spencer DD. Extracellular hippocampal glutamate and spontaneous seizure in the conscious human brain. Lancet. 1993;341:1607–1610. doi: 10.1016/0140-6736(93)90754-5. [DOI] [PubMed] [Google Scholar]
- El-Hassar L, Milh M, Wendling F, Ferrand N, Esclapez M, Bernard C. Cell domain-dependent changes in the glutamatergic and GABAergic drives during epileptogenesis in the rat CA1 region. J. Physiol. 2007;578:193–211. doi: 10.1113/jphysiol.2006.119297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Engel J. Seizures and Epilepsy. F.A. Davis; Philadelphia: 1989. [Google Scholar]
- Fanselow MS, Gale GD. The amygdala, fear, and memory. Ann N Y Acad. Sci. 2003;985:125–134. doi: 10.1111/j.1749-6632.2003.tb07077.x. [DOI] [PubMed] [Google Scholar]
- Feindel W, Rasmussen T. Temporal lobectomy with amygdalectomy and minimal hippocampal resection: review of 100 cases. Can. J. Neurol. Sci. 1991;18:603–605. doi: 10.1017/s0317167100032807. [DOI] [PubMed] [Google Scholar]
- Fowler M. Brain damage after febrile convulsions. Arch. Dis. Child. 1957;32:67–76. doi: 10.1136/adc.32.162.67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Francois J, Koning E, Ferrandon A, Nehlig A. The combination of topiramate and diazepam is partially neuroprotective in the hippocampus but not antiepileptogenic in the lithium-pilocarpine model of temporal lobe epilepsy. Epilepsy Res. 2006;72:147–163. doi: 10.1016/j.eplepsyres.2006.07.014. [DOI] [PubMed] [Google Scholar]
- Gavrilovici C, D’Alfonso S, Dann M, Poulter MO. Kindling-induced alterations in GABAA receptor-mediated inhibition and neurosteroid activity in the rat piriform cortex. Eur. J. Neurosci. 2006;24:1373–1384. doi: 10.1111/j.1460-9568.2006.05012.x. [DOI] [PubMed] [Google Scholar]
- Gilbert ME. The NMDA-receptor antagonist, MK-801, suppresses limbic kindling and kindled seizures. Brain Res. 1988;463:90–99. doi: 10.1016/0006-8993(88)90530-6. [DOI] [PubMed] [Google Scholar]
- Gilby KL, Da Silva AG, McIntyre DC. Differential GABA(A) subunit expression following status epilepticus in seizure-prone and seizure-resistant rats: a putative mechanism for refractory drug response. Epilepsia. 2005;46:3–9. doi: 10.1111/j.1528-1167.2005.01001.x. [DOI] [PubMed] [Google Scholar]
- Goddard GV. Development of epileptic seizures through brain stimulation at low intensity. Nature. 1967;214:1020–1021. doi: 10.1038/2141020a0. [DOI] [PubMed] [Google Scholar]
- Gorter JA, van Vliet EA, Aronica E, Breit T, Rauwerda H, Lopes da Silva FH, Wadman WJ. Potential new antiepileptogenic targets indicated by microarray analysis in a rat model for temporal lobe epilepsy. J. Neurosci. 2006;26:11083–11110. doi: 10.1523/JNEUROSCI.2766-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gryder DS, Rogawski MA. Selective antagonism of GluR5 kainate-receptor-mediated synaptic currents by topiramate in rat basolateral amygdala neurons. J. Neurosci. 2003;23:7069–7074. doi: 10.1523/JNEUROSCI.23-18-07069.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerreiro C, Cendes F, Li LM, Jones-Gotman M, Andermann F, Dubeau F, Piazzini A, Feindel W. Clinical patterns of patients with temporal lobe epilepsy and pure amygdalar atrophy. Epilepsia. 1999;40:453–461. doi: 10.1111/j.1528-1157.1999.tb00740.x. [DOI] [PubMed] [Google Scholar]
- Gupta YK, Gupta M. Post traumatic epilepsy: a review of scientific evidence. Indian J. Physiol. Pharmacol. 2006;50:7–16. [PubMed] [Google Scholar]
- Halonen T, Nissinen J, Pitkanen A. Chronic elevation of brain GABA levels beginning two days after status epilepticus does not prevent epileptogenesis in rats. Neuropharmacology. 2001;40:536–550. doi: 10.1016/s0028-3908(00)00183-0. [DOI] [PubMed] [Google Scholar]
- Harden CL. Sexuality in men and women with epilepsy. CNS Spectr. 2006;11:13–18. doi: 10.1017/s1092852900026717. [DOI] [PubMed] [Google Scholar]
- Herman ST. Epilepsy after brain insult: targeting epileptogenesis. Neurology. 2002;59:S21–26. doi: 10.1212/wnl.59.9_suppl_5.s21. [DOI] [PubMed] [Google Scholar]
- Herzog AG, Coleman AE, Jacobs AR, Klein P, Friedman MN, Drislane FW, Schomer DL. Relationship of sexual dysfunction to epilepsy laterality and reproductive hormone levels in women. Epilepsy Behav. 2003;4:407–413. doi: 10.1016/s1525-5050(03)00121-5. [DOI] [PubMed] [Google Scholar]
- Hirose S, Okada M, Kaneko S, Mitsudome A. Are some idiopathic epilepsies disorders of ion channels?: A working hypothesis. Epilepsy Res. 2000;41:191–204. doi: 10.1016/s0920-1211(00)00141-8. [DOI] [PubMed] [Google Scholar]
- Holmes KH, Bilkey DK, Laverty R, Goddard GV. The N-methyl-D-aspartate antagonists aminophosphonovalerate and carboxypiperazinephosphonate retard the development and expression of kindled seizures. Brain Res. 1990;506:227–235. doi: 10.1016/0006-8993(90)91255-f. [DOI] [PubMed] [Google Scholar]
- Hudson LP, Munoz DG, Miller L, McLachlan RS, Girvin JP, Blume WT. Amygdaloid sclerosis in temporal lobe epilepsy. Ann Neurol. 1993;33:622–631. doi: 10.1002/ana.410330611. [DOI] [PubMed] [Google Scholar]
- Inoue K, Morimoto K, Sato K, Yamada N, Otsuki S. Mechanisms in the development of limbic status epilepticus and hippocampal neuron loss: an experimental study in a model of status epilepticus induced by kindling-like electrical stimulation of the deep prepyriform cortex in rats. Acta Med. Okayama. 1992;46:129–139. doi: 10.18926/AMO/32652. [DOI] [PubMed] [Google Scholar]
- Isokawa-Akesson M, Wilson CL, Babb TL. Structurally stable burst and synchronized firing in human amygdala neurons: auto- and cross-correlation analyses in temporal lobe epilepsy. Epilepsy Res. 1987;1:17–34. doi: 10.1016/0920-1211(87)90047-7. [DOI] [PubMed] [Google Scholar]
- Jooma R, Yeh HS, Privitera MD, Rigrish D, Gartner M. Seizure control and extent of mesial temporal resection. Acta Neurochir. (Wien) 1995;133:44–49. doi: 10.1007/BF01404946. [DOI] [PubMed] [Google Scholar]
- Joy RM, Albertson TE, Stark LG. An analysis of the actions of progabide, a specific GABA receptor agonist, on kindling and kindled seizures. Exp. Neurol. 1984;83:144–154. doi: 10.1016/0014-4886(84)90053-0. [DOI] [PubMed] [Google Scholar]
- Kairiss EW, Racine RJ, Smith GK. The development of the interictal spike during kindling in the rat. Brain Res. 1984;322:101–110. doi: 10.1016/0006-8993(84)91185-5. [DOI] [PubMed] [Google Scholar]
- Kalviainen R, Salmenpera T, Partanen K, Vainio P, Riekkinen P, Pitkanen A. MRI volumetry and T2 relaxometry of the amygdala in newly diagnosed and chronic temporal lobe epilepsy. Epilepsy Res. 1997;28:39–50. doi: 10.1016/s0920-1211(97)00029-6. [DOI] [PubMed] [Google Scholar]
- Kaminski RM, Banerjee M, Rogawski MA. Topiramate selectively protects against seizures induced by ATPA, a GluR5 kainate receptor agonist. Neuropharmacology. 2004;46:1097–1104. doi: 10.1016/j.neuropharm.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Kanner AM. Depression and Epilepsy: A New Perspective on Two Closely Related Disorders. Epilepsy Curr. 2006;6:141–146. doi: 10.1111/j.1535-7511.2006.00125.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JE, Kwak SE, Kim DS, Won MH, Choi HC, Song HK, Kim YI, Kang TC. Up-regulation of P/Q-type voltage-gated Ca(2+) channel immunoreactivity within parvalbumin positive neurons in the rat hippocampus following status epilepticus. Neurosci. Res. 2007;57:379–386. doi: 10.1016/j.neures.2006.11.007. [DOI] [PubMed] [Google Scholar]
- Kostarczyk EM. The amygdala and male reproductive functions: I. Anatomical and endocrine bases. Neurosci. Biobehav. Rev. 1986;10:67–77. doi: 10.1016/0149-7634(86)90019-9. [DOI] [PubMed] [Google Scholar]
- Koyama R, Ikegaya Y. To BDNF or not to BDNF: that is the epileptic hippocampus. Neuroscientist. 2005;11:282–7. doi: 10.1177/1073858405278266. [DOI] [PubMed] [Google Scholar]
- Lahtinen L, Lukasiuk K, Pitkanen A. Increased expression and activity of urokinase-type plasminogen activator during epileptogenesis. Eur. J. Neurosci. 2006;24:1935–1945. doi: 10.1111/j.1460-9568.2006.05062.x. [DOI] [PubMed] [Google Scholar]
- Lallement G, Carpentier P, Collet A, Pernot-Marino I, Baubichon D, Blanchet G. Effects of soman-induced seizures on different extracellular amino acid levels and on glutamate uptake in rat hippocampus. Brain Res. 1991a;563:234–240. doi: 10.1016/0006-8993(91)91539-d. [DOI] [PubMed] [Google Scholar]
- Lallement G, Carpentier P, Collet A, Pernot-Marino I, Baubichon D, Sentenac-Roumanou H, Blanchet G. Involvement of glutamatergic system of amygdala in generalized seizures induced by soman: comparison with the hippocampus. C R Acad. Sci. III. 1991b;313:421–426. [PubMed] [Google Scholar]
- Lallement G, Denoyer M, Collet A, Pernot-Marino I, Baubichon D, Monmaur P, Blanchet G. Changes in hippocampal acetylcholine and glutamate extracellular levels during soman-induced seizures: influence of septal cholinoceptive cells. Neurosci. Lett. 1992;139:104–107. doi: 10.1016/0304-3940(92)90868-8. [DOI] [PubMed] [Google Scholar]
- LeDoux JE. Brain mechanisms of emotion and emotional learning. Curr. Opin. Neurobiol. 1992;2:191–197. doi: 10.1016/0959-4388(92)90011-9. [DOI] [PubMed] [Google Scholar]
- Lerche H, Weber YG, Jurkat-Rott K, Lehmann-Horn F. Ion channel defects in idiopathic epilepsies. Curr. Pharm. Des. 2005;11:2737–2752. doi: 10.2174/1381612054546815. [DOI] [PubMed] [Google Scholar]
- Li H, Chen A, Xing G, Wei ML, Rogawski MA. Kainate receptor-mediated heterosynaptic facilitation in the amygdala. Nat. Neurosci. 2001;4:612–620. doi: 10.1038/88432. [DOI] [PubMed] [Google Scholar]
- Liu Z, Stafstrom CE, Sarkisian MR, Yang Y, Hori A, Tandon P, Holmes GL. Seizure-induced glutamate release in mature and immature animals: an in vivo microdialysis study. Neuroreport. 1997;8:2019–2023. doi: 10.1097/00001756-199705260-00043. [DOI] [PubMed] [Google Scholar]
- Loscher W, Schwark WS. Evaluation of different GABA receptor agonists in the kindled amygdala seizure model in rats. Exp. Neurol. 1985;89:454–460. doi: 10.1016/0014-4886(85)90104-9. [DOI] [PubMed] [Google Scholar]
- Loscher W. Animal models of epilepsy for the development of antiepileptogenic and disease-modifying drugs. A comparison of the pharmacology of kindling and post-status epilepticus models of temporal lobe epilepsy. Epilepsy Res. 2002;50:105–123. doi: 10.1016/s0920-1211(02)00073-6. [DOI] [PubMed] [Google Scholar]
- Lurton D, Cavalheiro EA. Neuropeptide-Y immunoreactivity in the pilocarpine model of temporal lobe epilepsy. Exp. Brain Res. 1997;116:186–90. doi: 10.1007/pl00005739. [DOI] [PubMed] [Google Scholar]
- Lukasiuk K, Dabrowski M, Adach A, Pitkanen A. Epileptogenesis-related genes revisited. Prog. Brain Res. 2006;158:223–241. doi: 10.1016/S0079-6123(06)58011-2. [DOI] [PubMed] [Google Scholar]
- Mangan PS, Scott CA, Williamson JM, Bertram EH. Aberrant neuronal physiology in the basal nucleus of the amygdala in a model of chronic limbic epilepsy. Neuroscience. 2000;101:377–391. doi: 10.1016/s0306-4522(00)00358-4. [DOI] [PubMed] [Google Scholar]
- Margerison JH, Corsellis JA. Epilepsy and the temporal lobes. A clinical, electroencephalographic and neuropathological study of the brain in epilepsy, with particular reference to the temporal lobes. Brain. 1966;89:499–530. doi: 10.1093/brain/89.3.499. [DOI] [PubMed] [Google Scholar]
- McDonald AJ, Pearson JC. Coexistence of GABA and peptide immunoreactivity in non-pyramidal neurons of the basolateral amygdala. Neurosci. Lett. 1989;100:53–58. doi: 10.1016/0304-3940(89)90659-9. [DOI] [PubMed] [Google Scholar]
- McDonald AJ, Mascagni F. Colocalization of calcium-binding proteins and GABA in neurons of the rat basolateral amygdala. Neuroscience. 2001;105:681–693. doi: 10.1016/s0306-4522(01)00214-7. [DOI] [PubMed] [Google Scholar]
- McDonald AJ, Mascagni F. Immunohistochemical characterization of somatostatin containing interneurons in the rat basolateral amygdala. Brain Res. 2002;943:237–244. doi: 10.1016/s0006-8993(02)02650-1. [DOI] [PubMed] [Google Scholar]
- McDonald AJ. Is there an amygdala and how far does it extend? An anatomical perspective. Ann N Y Acad. Sci. 2003;985:1–21. doi: 10.1111/j.1749-6632.2003.tb07067.x. [DOI] [PubMed] [Google Scholar]
- McDonough JH, Shih TM. Neuropharmacological mechanisms of nerve agent-induced seizure and neuropathology. Neurosci. Biobehav. Rev. 1997;21:559–579. doi: 10.1016/s0149-7634(96)00050-4. [DOI] [PubMed] [Google Scholar]
- McGaugh JL, Cahill L, Roozendaal B. Involvement of the amygdala in memory storage: interaction with other brain systems. Proc. Natl. Acad. Sci. U S A. 1996;93:13508–13514. doi: 10.1073/pnas.93.24.13508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McIntyre DC, Racine RJ. Kindling mechanisms: current progress on an experimental epilepsy model. Prog. Neurobiol. 1986;27:1–12. doi: 10.1016/0301-0082(86)90010-9. [DOI] [PubMed] [Google Scholar]
- McIntyre DC, Kelly ME, Dufresne C. FAST and SLOW amygdala kindling rat strains: comparison of amygdala, hippocampal, piriform and perirhinal cortex kindling. Epilepsy Res. 1999;35:197–209. doi: 10.1016/s0920-1211(99)00012-1. [DOI] [PubMed] [Google Scholar]
- McIntyre DC, Poulter MO, Gilby K. Kindling: some old and some new. Epilepsy Res. 2002;50:79–92. doi: 10.1016/s0920-1211(02)00071-2. [DOI] [PubMed] [Google Scholar]
- McNamara JO, Russell RD, Rigsbee L, Bonhaus DW. Anticonvulsant and antiepileptogenic actions of MK-801 in the kindling and electroshock models. Neuropharmacology. 1988;27:563–568. doi: 10.1016/0028-3908(88)90176-1. [DOI] [PubMed] [Google Scholar]
- McNamara JO, Huang YZ, Leonard AS. Molecular signaling mechanisms underlying epileptogenesis. Sci STKE. 2006;2006:re12. doi: 10.1126/stke.3562006re12. [DOI] [PubMed] [Google Scholar]
- Meldrum BS, Brierley JB. Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch. Neurol. 1973;28:10–17. doi: 10.1001/archneur.1973.00490190028002. [DOI] [PubMed] [Google Scholar]
- Meyer A, Beck E, Shepherd M. Unusually severe lesions in the brain following status epilepticus. J. Neurol. Neurosurg. Psychiatry. 1955;18:24–33. doi: 10.1136/jnnp.18.1.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller LA, McLachlan RS, Bouwer MS, Hudson LP, Munoz DG. Amygdalar sclerosis: preoperative indicators and outcome after temporal lobectomy. J. Neurol. Neurosurg. Psychiatry. 1994;57:1099–1105. doi: 10.1136/jnnp.57.9.1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mohapel P, Dufresne C, Kelly ME, McIntyre DC. Differential sensitivity of various temporal lobe structures in the rat to kindling and status epilepticus induction. Epilepsy Res. 1996;23:179–187. doi: 10.1016/0920-1211(95)00084-4. [DOI] [PubMed] [Google Scholar]
- Mori N, Wada JA. Bidirectional transfer between kindling induced by excitatory amino acids and electrical stimulation. Brain Res. 1987;425:45–48. doi: 10.1016/0006-8993(87)90481-1. [DOI] [PubMed] [Google Scholar]
- Morimoto K, Katayama K, Inoue K, Sato K. Effects of competitive and noncompetitive NMDA receptor antagonists on kindling and LTP. Pharmacol. Biochem. Behav. 1991;40:893–899. doi: 10.1016/0091-3057(91)90103-9. [DOI] [PubMed] [Google Scholar]
- Morimoto K, Fahnestock M, Racine RJ. Kindling and status epilepticus models of epilepsy: rewiring the brain. Prog. Neurobiol. 2004;73:1–60. doi: 10.1016/j.pneurobio.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Muller JF, Mascagni F, McDonald AJ. Postsynaptic targets of somatostatin-containing interneurons in the rat basolateral amygdala. J Comp Neurol. 2007;500:513–529. doi: 10.1002/cne.21185. [DOI] [PubMed] [Google Scholar]
- Nairismagi J, Grohn OH, Kettunen MI, Nissinen J, Kauppinen RA, Pitkanen A. Progression of brain damage after status epilepticus and its association with epileptogenesis: a quantitative MRI study in a rat model of temporal lobe epilepsy. Epilepsia. 2004;45:1024–1034. doi: 10.1111/j.0013-9580.2004.08904.x. [DOI] [PubMed] [Google Scholar]
- Nakasu Y, Nakasu S, Morikawa S, Uemura S, Inubushi T, Handa J. Diffusion-weighted MR in experimental sustained seizures elicited with kainic acid. AJNR Am. J. Neuroradiol. 1995;16:1185–1192. [PMC free article] [PubMed] [Google Scholar]
- Namba T, Morimoto K, Sato K, Yamada N, Kuroda S. Antiepileptogenic and anticonvulsant effects of NBQX, a selective AMPA receptor antagonist, in the rat kindling model of epilepsy. Brain Res. 1994;638:36–44. doi: 10.1016/0006-8993(94)90630-0. [DOI] [PubMed] [Google Scholar]
- Niittykoski M, Nissinen J, Penttonen M, Pitkanen A. Electrophysiologic changes in the lateral and basal amygdaloid nuclei in temporal lobe epilepsy: an in vitro study in epileptic rats. Neuroscience. 2004;124:269–281. doi: 10.1016/j.neuroscience.2003.11.027. [DOI] [PubMed] [Google Scholar]
- Norman RM. The Neuropathology of Status Epilepticus. Med. Sci. Law. 1964;14:46–51. doi: 10.1177/002580246400400112. [DOI] [PubMed] [Google Scholar]
- Oberto A, Acquadro E, Bus T, Sprengel R, Eva C. Expression patterns of promoters for NPY Y(1) and Y(5) receptors in Y(5)RitTA and Y(1)RVenus BAC-transgenic mice. Eur. J. Neurosci. 2007;26:155–170. doi: 10.1111/j.1460-9568.2007.05631.x. [DOI] [PubMed] [Google Scholar]
- Pagni CA, Zenga F. Prevention and treatment of post-traumatic epilepsy. Expert Rev. Neurother. 2006;6:1223–1233. doi: 10.1586/14737175.6.8.1223. [DOI] [PubMed] [Google Scholar]
- Pal S, Sombati S, Limbrick DD, Jr., DeLorenzo RJ. In vitro status epilepticus causes sustained elevation of intracellular calcium levels in hippocampal neurons. Brain Res. 1999;851:20–31. doi: 10.1016/s0006-8993(99)02035-1. [DOI] [PubMed] [Google Scholar]
- Pal S, Limbrick DD, Jr., Rafiq A, DeLorenzo RJ. Induction of spontaneous recurrent epileptiform discharges causes long-term changes in intracellular calcium homeostatic mechanisms. Cell Calcium. 2000;28:181–193. doi: 10.1054/ceca.2000.0146. [DOI] [PubMed] [Google Scholar]
- Park JH, Cho H, Kim H, Kim K. Repeated brief epileptic seizures by pentylenetetrazole cause neurodegeneration and promote neurogenesis in discrete brain regions of freely moving adult rats. Neuroscience. 2006;140:673–684. doi: 10.1016/j.neuroscience.2006.02.076. [DOI] [PubMed] [Google Scholar]
- Paxinos G, Watson C. The Rat Brain in Stereotaxic Coordinates. Fourth Edition Academic Press; San Diego: 1998. [Google Scholar]
- Pena F, Tapia R. Relationships among seizures, extracellular amino acid changes, and neurodegeneration induced by 4-aminopyridine in rat hippocampus: a microdialysis and electroencephalographic study. J. Neurochem. 1999;72:2006–2014. doi: 10.1046/j.1471-4159.1999.0722006.x. [DOI] [PubMed] [Google Scholar]
- Penschuck S, Bastlund JF, Jensen HS, Stensbol TB, Egebjerg J, Watson WP. Changes in KCNQ2 immunoreactivity in the amygdala in two rat models of temporal lobe epilepsy. Brain Res. Mol. Brain Res. 2005;141:66–73. doi: 10.1016/j.molbrainres.2005.08.004. [DOI] [PubMed] [Google Scholar]
- Pitkanen A, Tuunanen J, Kalviainen R, Partanen K, Salmenpera T. Amygdala damage in experimental and human temporal lobe epilepsy. Epilepsy Res. 1998;32:233–253. doi: 10.1016/s0920-1211(98)00055-2. [DOI] [PubMed] [Google Scholar]
- Qi JS, Yao J, Fang C, Luscher B, Chen G. Downregulation of tonic GABA currents following epileptogenic stimulation of rat hippocampal cultures. J. Physiol. 2006;577:579–90. doi: 10.1113/jphysiol.2006.113134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quesney LF. Clinical and EEG features of complex partial seizures of temporal lobe origin. Epilepsia. 1986;27:S27–45. doi: 10.1111/j.1528-1157.1986.tb05738.x. [DOI] [PubMed] [Google Scholar]
- Racine RJ, Paxinos G, Mosher JM, Kairiss EW. The effects of various lesions and knife-cuts on septal and amygdala kindling in the rat. Brain Res. 1988;454:264–274. doi: 10.1016/0006-8993(88)90826-8. [DOI] [PubMed] [Google Scholar]
- Racine RJ, Steingart M, McIntyre DC. Development of kindling-prone and kindling-resistant rats: selective breeding and electrophysiological studies. Epilepsy Res. 1999;35:183–195. doi: 10.1016/s0920-1211(99)00013-3. [DOI] [PubMed] [Google Scholar]
- Rainnie DG, Asprodini EK, Shinnick-Gallagher P. Kindling-induced long-lasting changes in synaptic transmission in the basolateral amygdala. J. Neurophysiol. 1992;67:443–454. doi: 10.1152/jn.1992.67.2.443. [DOI] [PubMed] [Google Scholar]
- Raol YH, Lund IV, Bandyopadhyay S, Zhang G, Roberts DS, Wolfe JH, Russek SJ, Brooks-Kayal AR. Enhancing GABA(A) receptor alpha 1 subunit levels in hippocampal dentate gyrus inhibits epilepsy development in an animal model of temporal lobe epilepsy. J. Neurosci. 2006;26:11342–11346. doi: 10.1523/JNEUROSCI.3329-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rauch SL, Whalen PJ, Shin LM, McInerney SC, Macklin ML, Lasko NB, Orr SP, Pitman RK. Exaggerated amygdala response to masked facial stimuli in posttraumatic stress disorder: a functional MRI study. Biol. Psychiatry. 2000;47:769–776. doi: 10.1016/s0006-3223(00)00828-3. [DOI] [PubMed] [Google Scholar]
- Reibel S, Larmet Y, Carnahan J, Marescaux C, Depaulis A. Endogenous control of hippocampal epileptogenesis: a molecular cascade involving brain-derived neurotrophic factor and neuropeptide Y. Epilepsia. 2000;41:S127–33. doi: 10.1111/j.1528-1157.2000.tb01571.x. [DOI] [PubMed] [Google Scholar]
- Reibel S, Benmaamar R, Lê BT, Larmet Y, Kalra SP, Marescaux C, Depaulis A. Neuropeptide Y delays hippocampal kindling in the rat. Hippocampus. 2003;13:557–560. doi: 10.1002/hipo.10110. [DOI] [PubMed] [Google Scholar]
- Rice AC, DeLorenzo RJ. NMDA receptor activation during status epilepticus is required for the development of epilepsy. Brain Res. 1998;782:240–247. doi: 10.1016/s0006-8993(97)01285-7. [DOI] [PubMed] [Google Scholar]
- Richardson EJ, Griffith HR, Martin RC, Paige AL, Stewart CC, Jones J, Hermann BP, Seidenberg M. Structural and functional neuroimaging correlates of depression in temporal lobe epilepsy. Epilepsy Behav. 2007;10:242–249. doi: 10.1016/j.yebeh.2006.11.013. [DOI] [PubMed] [Google Scholar]
- Rogawski MA, Kurzman PS, Yamaguchi SI, Li H. Role of AMPA and GluR5 kainate receptors in the development and expression of amygdala kindling in the mouse. Neuropharmacology. 2001;40:28–35. doi: 10.1016/s0028-3908(00)00112-x. [DOI] [PubMed] [Google Scholar]
- Rogawski MA, Gryder D, Castaneda D, Yonekawa W, Banks MK, Lia H. GluR5 kainate receptors, seizures, and the amygdala. Ann N Y Acad. Sci. 2003;985:150–162. doi: 10.1111/j.1749-6632.2003.tb07079.x. [DOI] [PubMed] [Google Scholar]
- Sah P, Faber ES, Lopez De Armentia M, Power J. The amygdaloid complex: anatomy and physiology. Physiol. Rev. 2003;83:803–834. doi: 10.1152/physrev.00002.2003. [DOI] [PubMed] [Google Scholar]
- Salamon E, Esch T, Stefano GB. Role of amygdala in mediating sexual and emotional behavior via coupled nitric oxide release. Acta Pharmacol. Sin. 2005;26:389–395. doi: 10.1111/j.1745-7254.2005.00083.x. [DOI] [PubMed] [Google Scholar]
- Salazar AM, Jabbari B, Vance SC, Grafman J, Amin D, Dillon JD. Epilepsy after penetrating head injury. I. Clinical correlates: a report of the Vietnam Head Injury Study. Neurology. 1985;35:1406–1414. doi: 10.1212/wnl.35.10.1406. [DOI] [PubMed] [Google Scholar]
- Salmenpera T, Kalviainen R, Partanen K, Pitkanen A. Hippocampal and amygdaloid damage in partial epilepsy: a cross-sectional MRI study of 241 patients. Epilepsy Res. 2001;46:69–82. doi: 10.1016/s0920-1211(01)00258-3. [DOI] [PubMed] [Google Scholar]
- Sato K, Morimoto K, Okamoto M. Anticonvulsant action of a non-competitive antagonist of NMDA receptors (MK-801) in the kindling model of epilepsy. Brain Res. 1988;463:12–20. doi: 10.1016/0006-8993(88)90521-5. [DOI] [PubMed] [Google Scholar]
- Saukkonen A, Kalviainen R, Partanen K, Vainio P, Riekkinen P, Pitkanen A. Do seizures cause neuronal damage? A MRI study in newly diagnosed and chronic epilepsy. Neuroreport. 1994;6:219–223. doi: 10.1097/00001756-199412300-00055. [DOI] [PubMed] [Google Scholar]
- Schwark WS, Haluska M. Prophylaxis of amygdala kindling-induced epileptogenesis: comparison of a GABA uptake inhibitor and diazepam. Epilepsy Res. 1987;1:63–69. doi: 10.1016/0920-1211(87)90052-0. [DOI] [PubMed] [Google Scholar]
- Seethalakshmi R, Krishnamoorthy ES. Depression in epilepsy: phenomenology, diagnosis and management. Epileptic Disord. 2007;9:1–10. doi: 10.1684/epd.2007.0063. [DOI] [PubMed] [Google Scholar]
- Semah F, Picot MC, Adam C, Broglin D, Arzimanoglou A, Bazin B, Cavalcanti D, Baulac M. Is the underlying cause of epilepsy a major prognostic factor for recurrence? Neurology. 1998;51:1256–1262. doi: 10.1212/wnl.51.5.1256. [DOI] [PubMed] [Google Scholar]
- Sherwin AL. Neuroactive amino acids in focally epileptic human brain: a review. Neurochem Res. 1999;24:1387–1395. doi: 10.1023/a:1022580506443. [DOI] [PubMed] [Google Scholar]
- Shih TM, Duniho SM, McDonough JH. Control of nerve agent-induced seizures is critical for neuroprotection and survival. Toxicol. Appl. Pharmacol. 2003;188:69–80. doi: 10.1016/s0041-008x(03)00019-x. [DOI] [PubMed] [Google Scholar]
- Shin C, Rigsbee LC, McNamara JO. Anti-seizure and anti-epileptogenic effect of gamma-vinyl gamma-aminobutyric acid in amygdaloid kindling. Brain Res. 1986;398:370–374. doi: 10.1016/0006-8993(86)91498-8. [DOI] [PubMed] [Google Scholar]
- Shin RS, Anisman H, Merali Z, McIntyre DC. Amygdala amino acid and monoamine levels in genetically Fast and Slow kindling rat strains during massed amygdala kindling: a microdialysis study. Eur. J. Neurosci. 2004;20:185–94. doi: 10.1111/j.1460-9568.2004.03477.x. [DOI] [PubMed] [Google Scholar]
- Shin RS, McIntyre DC. Differential noradrenergic influence on seizure expression in genetically Fast and Slow kindling rat strains during massed trial stimulation of the amygdala. Neuropharmacology. 2007;52:321–332. doi: 10.1016/j.neuropharm.2006.08.004. [DOI] [PubMed] [Google Scholar]
- Shoji Y, Tanaka E, Yamamoto S, Maeda H, Higashi H. Mechanisms underlying the enhancement of excitatory synaptic transmission in basolateral amygdala neurons of the kindling rat. J. Neurophysiol. 1998;80:638–646. doi: 10.1152/jn.1998.80.2.638. [DOI] [PubMed] [Google Scholar]
- Smith BN, Dudek FE. Enhanced population responses in the basolateral amygdala of kainate-treated, epileptic rats in vitro. Neurosci. Lett. 1997;222:1–4. doi: 10.1016/s0304-3940(97)13326-2. [DOI] [PubMed] [Google Scholar]
- Smolders I, Khan GM, Lindekens H, Prikken S, Marvin CA, Manil J, Ebinger G, Michotte Y. Effectiveness of vigabatrin against focally evoked pilocarpine-induced seizures and concomitant changes in extracellular hippocampal and cerebellar glutamate, gamma-aminobutyric acid and dopamine levels, a microdialysis-electrocorticography study in freely moving rats. J. Pharmacol. Exp. Ther. 1997;283:1239–1248. [PubMed] [Google Scholar]
- Smolders I, Bortolotto ZA, Clarke VR, Warre R, Khan GM, O’Neill MJ, Ornstein PL, Bleakman D, Ogden A, Weiss B, Stables JP, Ho KH, Ebinger G, Collingridge GL, Lodge D, Michotte Y. Antagonists of GLU(K5)-containing kainate receptors prevent pilocarpine-induced limbic seizures. Nat. Neurosci. 2002;5:796–804. doi: 10.1038/nn880. [DOI] [PubMed] [Google Scholar]
- Stafstrom CE, Holmes GL, Thompson JL. MK801 pretreatment reduces kainic acid-induced spontaneous seizures in prepubescent rats. Epilepsy Res. 1993;14:41–48. doi: 10.1016/0920-1211(93)90073-g. [DOI] [PubMed] [Google Scholar]
- Stanić D, Brumovsky P, Fetissov S, Shuster S, Herzog H, Hökfelt T. Characterization of neuropeptide Y2 receptor protein expression in the mouse brain. I. Distribution in cell bodies and nerve terminals. J. Comp. Neurol. 2006;499:357–190. doi: 10.1002/cne.21046. [DOI] [PubMed] [Google Scholar]
- Statler KD. Pediatric posttraumatic seizures: epidemiology, putative mechanisms of epileptogenesis and promising investigational progress. Dev. Neurosci. 2006;28:354–363. doi: 10.1159/000094162. [DOI] [PubMed] [Google Scholar]
- Swinkels WA, van Emde Boas W, Kuyk J, van Dyck R, Spinhoven P. Interictal depression, anxiety, personality traits, and psychological dissociation in patients with temporal lobe epilepsy (TLE) and extra-TLE. Epilepsia. 2006;47:2092–2103. doi: 10.1111/j.1528-1167.2006.00808.x. [DOI] [PubMed] [Google Scholar]
- Taylor FB, Lowe K, Thompson C, McFall MM, Peskind ER, Kante,r ED, Allison N, Williams J, Martin P, Raskind MA. Daytime prazosin reduces psychological distress to trauma specific cues in civilian trauma posttraumatic stress disorder. Biol Psychiatry. 2006;59:577–81. doi: 10.1016/j.biopsych.2005.09.023. [DOI] [PubMed] [Google Scholar]
- Treib J, Haass A, Grauer MT. High-velocity bullet causing indirect trauma to the brain and symptomatic epilepsy. Mil. Med. 1996;161:61–64. [PubMed] [Google Scholar]
- Treiman DM. GABAergic mechanisms in epilepsy. Epilepsia. 2001;42:8–12. doi: 10.1046/j.1528-1157.2001.042suppl.3008.x. [DOI] [PubMed] [Google Scholar]
- Tuunanen J, Halonen T, Pitkanen A. Status epilepticus causes selective regional damage and loss of GABAergic neurons in the rat amygdaloid complex. Eur. J. Neurosci. 1996;8:2711–2725. doi: 10.1111/j.1460-9568.1996.tb01566.x. [DOI] [PubMed] [Google Scholar]
- Tuunanen J, Halonen T, Pitkanen A. Decrease in somatostatin-immunoreactive neurons in the rat amygdaloid complex in a kindling model of temporal lobe epilepsy. Epilepsy Res. 1997;26:315–327. doi: 10.1016/s0920-1211(96)00900-x. [DOI] [PubMed] [Google Scholar]
- Ueda Y, Yokoyama H, Nakajima A, Tokumaru J, Doi T, Mitsuyama Y. Glutamate excess and free radical formation during and following kainic acid-induced status epilepticus. Exp. Brain Res. 2002;147:219–226. doi: 10.1007/s00221-002-1224-4. [DOI] [PubMed] [Google Scholar]
- Uemura S, Kimura H. Amygdaloid kindling with bicuculline methiodide in rats. Exp. Neurol. 1988;102:346–353. doi: 10.1016/0014-4886(88)90230-0. [DOI] [PubMed] [Google Scholar]
- Van Paesschen W, Connelly A, Johnson CL, Duncan JS. The amygdala and intractable temporal lobe epilepsy: a quantitative magnetic resonance imaging study. Neurology. 1996;47:1021–1031. doi: 10.1212/wnl.47.4.1021. [DOI] [PubMed] [Google Scholar]
- Vezzani A, Sperk G. Overexpression of NPY and Y2 receptors in epileptic brain tissue: an endogenous neuroprotective mechanism in temporal lobe epilepsy? Neuropeptides. 2004;38:245–52. doi: 10.1016/j.npep.2004.05.004. [DOI] [PubMed] [Google Scholar]
- Wade JV, Samson FE, Nelson SR, Pazdernik TL. Changes in extracellular amino acids during soman- and kainic acid-induced seizures. J. Neurochem. 1987;49:645–650. doi: 10.1111/j.1471-4159.1987.tb02912.x. [DOI] [PubMed] [Google Scholar]
- Wasterlain C, Baldwin R, Itabashi H. Status epilepticus induces widespread neuronal injury in newborn marmosets. Epilepsia. 1996;37:141. [Google Scholar]
- White LE, Price JL. The functional anatomy of limbic status epilepticus in the rat. I. Patterns of 14C-2-deoxyglucose uptake and Fos immunocytochemistry. J. Neurosci. 1993a;13:4787–4809. doi: 10.1523/JNEUROSCI.13-11-04787.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White LE, Price JL. The functional anatomy of limbic status epilepticus in the rat. II. The effects of focal deactivation. J. Neurosci. 1993b;13:4810–4830. doi: 10.1523/JNEUROSCI.13-11-04810.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wieser HG. Mesial temporal lobe epilepsy versus amygdalar epilepsy: late seizure recurrence after initially successful amygdalotomy and regained seizure control following hippocampectomy. Epileptic Disord. 2000;2:141–152. [PubMed] [Google Scholar]
- Xu B, McIntyre DC, Fahnestock M, Racine RJ. Strain differences affect the induction of status epilepticus and seizure-induced morphological changes. Eur. J. Neurosci. 2004;20:403–18. doi: 10.1111/j.1460-9568.2004.03489.x. [DOI] [PubMed] [Google Scholar]
- Yi JH, Hazell AS. Excitotoxic mechanisms and the role of astrocytic glutamate transporters in traumatic brain injury. Neurochem. Int. 2006;48:394–403. doi: 10.1016/j.neuint.2005.12.001. [DOI] [PubMed] [Google Scholar]
- Yilmazer-Hanke DM, Faber-Zuschratter H, Blumcke I, Bickel M, Becker A, Mawrin C, Schramm J. Axo-somatic inhibition of projection neurons in the lateral nucleus of amygdala in human temporal lobe epilepsy: an ultrastructural study. Exp. Brain Res. 2006;177:384–399. doi: 10.1007/s00221-006-0680-7. [DOI] [PubMed] [Google Scholar]