Abstract
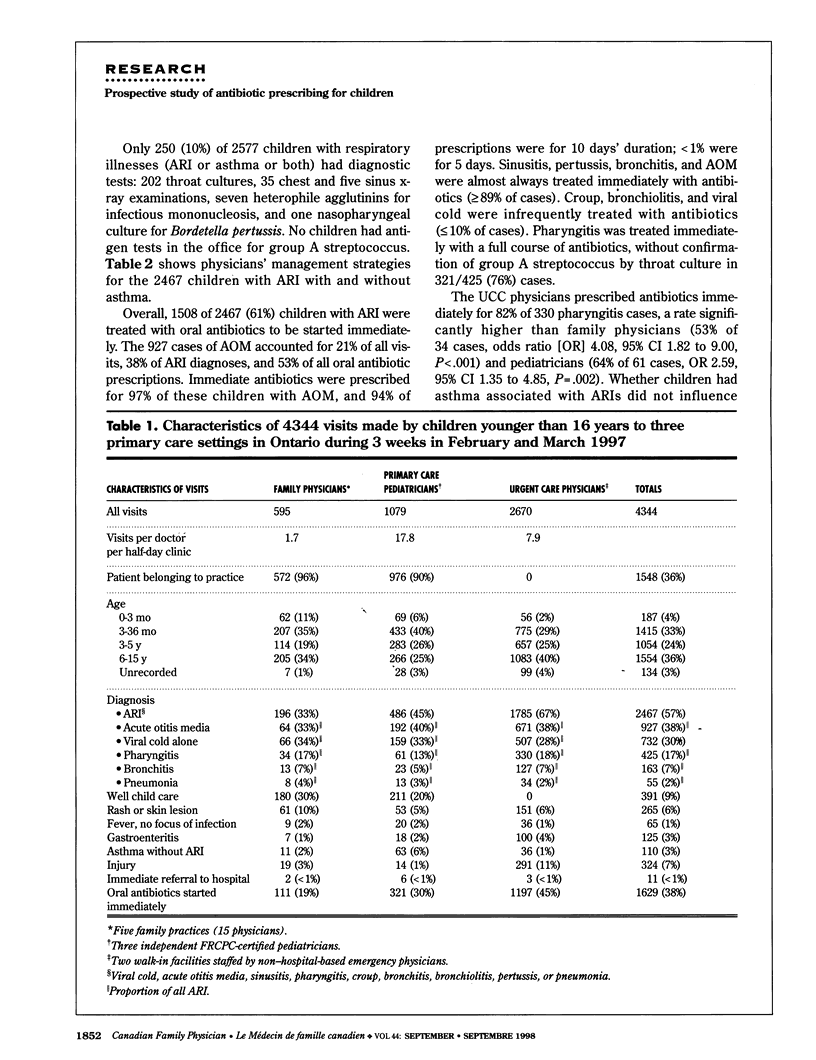
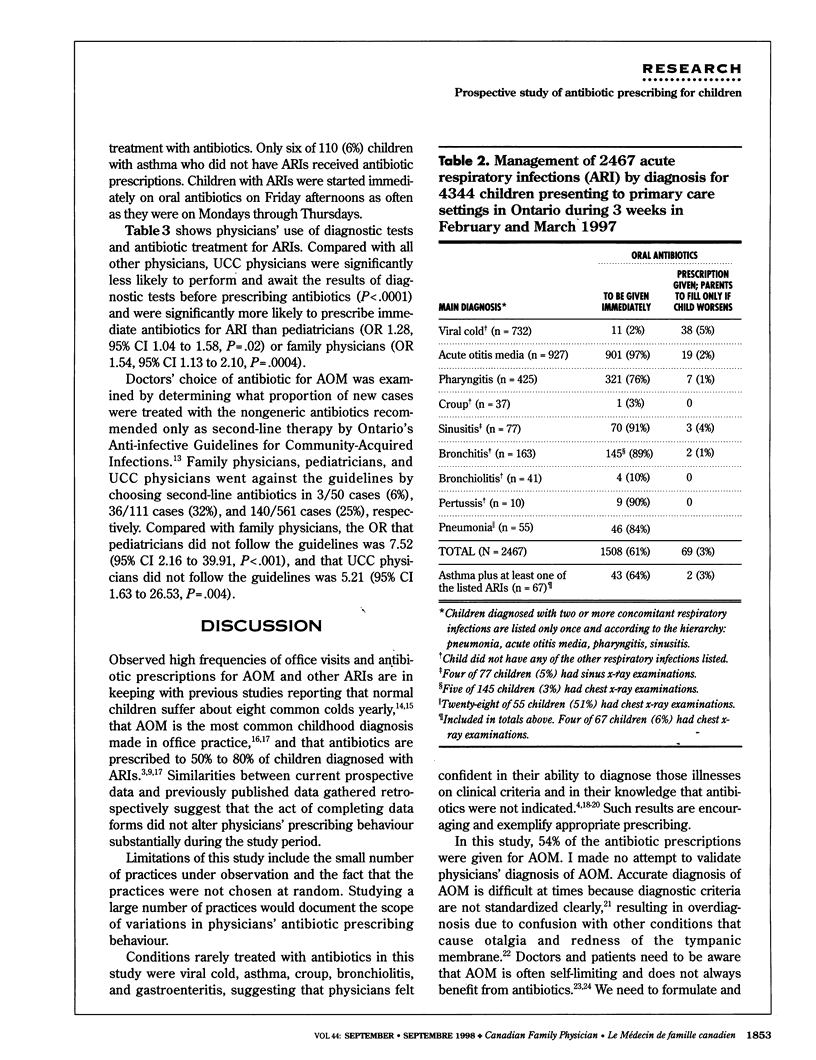
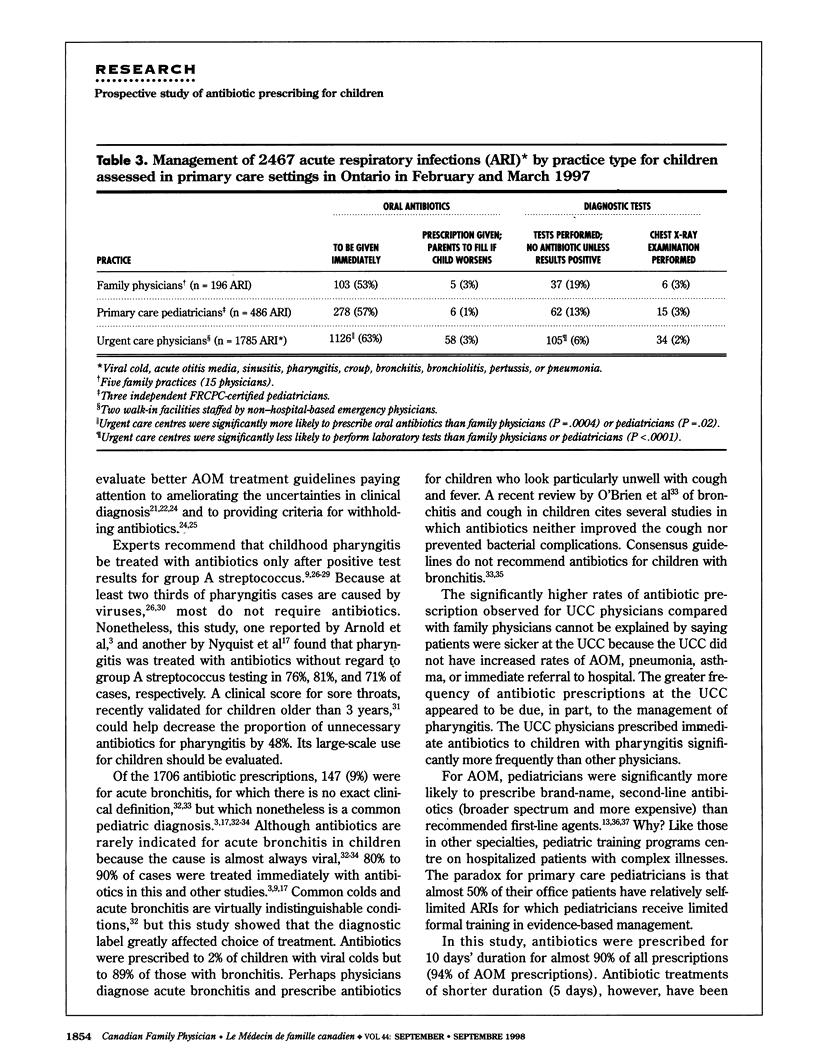
OBJECTIVES: To observe the frequency with which children in outpatient primary care settings are prescribed antibiotics and to investigate why these antibiotics are prescribed. To compare the prescribing behaviour of family doctors, primary care pediatricians, and urgent care physicians and to determine where refinements in management are most needed to reduce the number of antibiotic prescriptions appropriately. DESIGN: Prospective study using a data entry form with mostly closed-ended questions. SETTING: Ten primary care offices in urban south-central and eastern Ontario: five family practices, three pediatric practices, and two urgent care centres (UCC). PARTICIPANTS: Every child younger than 16 years visiting these offices during a 3-week period in February and March 1997. MAIN OUTCOME MEASURES: Frequency, clinical indications, and nature of the antibiotics prescribed. RESULTS: There were 4344 observed visits. Of 1706 antibiotic prescriptions, 1481 were for 10 days, and 1577 (92%) were for acute respiratory infections, 920 (53%) specifically for acute otitis media (AOM). Full courses of antibiotics were given immediately (i.e., without test results) to 321 (76%) of 425 children with pharyngitis. Antibiotics were prescribed for 145 (90%) of 163 children with bronchitis. Urgent care physicians were significantly more likely than pediatricians or family physicians to prescribe immediate antibiotics and to disregard guidelines when choosing antibiotics for uncomplicated AOM. CONCLUSIONS: Three diagnoses accounted for 82% of antibiotic prescriptions: AOM, pharyngitis, and bronchitis. Physicians should be more selective when deciding whether, and for how long, to prescribe antibiotics for those three common conditions. Substantial reductions in antibiotic use will require changes in how physicians manage suspected AOM, the most common indication for antibiotics.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Arnold K. E., Leggiadro R. J., Breiman R. F., Lipman H. B., Schwartz B., Appleton M. A., Cleveland K. O., Szeto H. C., Hill B. C., Tenover F. C. Risk factors for carriage of drug-resistant Streptococcus pneumoniae among children in Memphis, Tennessee. J Pediatr. 1996 Jun;128(6):757–764. doi: 10.1016/s0022-3476(96)70326-8. [DOI] [PubMed] [Google Scholar]
- Carter A. O., Strachan D., Appiah Y. Physician prescribing practices: What do we know? Where do we go? How do we get there? CMAJ. 1996 Jun 1;154(11):1649–1653. [PMC free article] [PubMed] [Google Scholar]
- Chapman R. S., Henderson F. W., Clyde W. A., Jr, Collier A. M., Denny F. W. The epidemiology of tracheobronchitis in pediatric practice. Am J Epidemiol. 1981 Dec;114(6):786–797. doi: 10.1093/oxfordjournals.aje.a113249. [DOI] [PubMed] [Google Scholar]
- Dowell S. F., Schwartz B. Resistant pneumococci: protecting patients through judicious use of antibiotics. Am Fam Physician. 1997 Apr;55(5):1647-54, 1657-8. [PubMed] [Google Scholar]
- Fox J. P., Hall C. E., Cooney M. K., Luce R. E., Kronmal R. A. The Seattle virus watch. II. Objectives, study population and its observation, data processing and summary of illnesses. Am J Epidemiol. 1972 Oct;96(4):270–285. doi: 10.1093/oxfordjournals.aje.a121458. [DOI] [PubMed] [Google Scholar]
- Green S. M. Acute pharyngitis: the case for empiric antimicrobial therapy. Ann Emerg Med. 1995 Mar;25(3):404–406. doi: 10.1016/s0196-0644(95)70310-2. [DOI] [PubMed] [Google Scholar]
- Harnett N., Brown S., Riley G., Krishnan C. Penicillin-resistant Streptococcus pneumoniae in Ontario, 1987-1995. Can Commun Dis Rep. 1997 May 1;23(9):65–72. [PubMed] [Google Scholar]
- Hayden G. F. Acute suppurative otitis media in children. Diversity of clinical diagnostic criteria. Clin Pediatr (Phila) 1981 Feb;20(2):99–104. doi: 10.1177/000992288102000203. [DOI] [PubMed] [Google Scholar]
- Hofer C., Binns H. J., Tanz R. R. Strategies for managing group A streptococcal pharyngitis. A survey of board-certified pediatricians. Arch Pediatr Adolesc Med. 1997 Aug;151(8):824–829. doi: 10.1001/archpedi.1997.02170450074012. [DOI] [PubMed] [Google Scholar]
- Kozyrskyj A. L., Hildes-Ripstein G. E., Longstaffe S. E., Wincott J. L., Sitar D. S., Klassen T. P., Moffatt M. E. Treatment of acute otitis media with a shortened course of antibiotics: a meta-analysis. JAMA. 1998 Jun 3;279(21):1736–1742. doi: 10.1001/jama.279.21.1736. [DOI] [PubMed] [Google Scholar]
- Kunin C. M. The responsibility of the infectious disease community for the optimal use of antimicrobial agents. J Infect Dis. 1985 Mar;151(3):388–398. doi: 10.1093/infdis/151.3.388. [DOI] [PubMed] [Google Scholar]
- McIsaac W. J., White D., Tannenbaum D., Low D. E. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ. 1998 Jan 13;158(1):75–83. [PMC free article] [PubMed] [Google Scholar]
- Nyquist A. C., Gonzales R., Steiner J. F., Sande M. A. Antibiotic prescribing for children with colds, upper respiratory tract infections, and bronchitis. JAMA. 1998 Mar 18;279(11):875–877. doi: 10.1001/jama.279.11.875. [DOI] [PubMed] [Google Scholar]
- Paradise J. L. Managing otitis media: a time for change. Pediatrics. 1995 Oct;96(4 Pt 1):712–715. [PubMed] [Google Scholar]
- Pichichero M. E., Cohen R. Shortened course of antibiotic therapy for acute otitis media, sinusitis and tonsillopharyngitis. Pediatr Infect Dis J. 1997 Jul;16(7):680–695. doi: 10.1097/00006454-199707000-00011. [DOI] [PubMed] [Google Scholar]
- Rosenfeld R. M., Vertrees J. E., Carr J., Cipolle R. J., Uden D. L., Giebink G. S., Canafax D. M. Clinical efficacy of antimicrobial drugs for acute otitis media: metaanalysis of 5400 children from thirty-three randomized trials. J Pediatr. 1994 Mar;124(3):355–367. doi: 10.1016/s0022-3476(94)70356-6. [DOI] [PubMed] [Google Scholar]
- Scriver S. R., Walmsley S. L., Kau C. L., Hoban D. J., Brunton J., McGeer A., Moore T. C., Witwicki E. Determination of antimicrobial susceptibilities of Canadian isolates of Haemophilus influenzae and characterization of their beta-lactamases. Canadian Haemophilus Study Group. Antimicrob Agents Chemother. 1994 Jul;38(7):1678–1680. doi: 10.1128/aac.38.7.1678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soyka L. F., Robinson D. S., Lachant N., Monaco J. The misuse of antibiotics for treatment of upper respiratory tract infections in children. Pediatrics. 1975 Apr;55(4):552–556. [PubMed] [Google Scholar]
- Stephenson J. Icelandic researchers are showing the way to bring down rates of antibiotic-resistant bacteria. JAMA. 1996 Jan 17;275(3):175–175. [PubMed] [Google Scholar]
- Teele D. W., Klein J. O., Rosner B., Bratton L., Fisch G. R., Mathieu O. R., Porter P. J., Starobin S. G., Tarlin L. D., Younes R. P. Middle ear disease and the practice of pediatrics. Burden during the first five years of life. JAMA. 1983 Feb 25;249(8):1026–1029. [PubMed] [Google Scholar]
- van Buchem F. L., Peeters M. F., van 't Hof M. A. Acute otitis media: a new treatment strategy. Br Med J (Clin Res Ed) 1985 Apr 6;290(6474):1033–1037. doi: 10.1136/bmj.290.6474.1033. [DOI] [PMC free article] [PubMed] [Google Scholar]


